Abstract
Background
Although the term “polytrauma” has been in use for decades, no generally accepted definition exists. The aim of this study was to demonstrate that different polytrauma definitions applied to a specific patient population result in diverse subgroups of individuals, who in turn present a varying outcome.
Methods
All patients (≥18 years) treated at our level I trauma center within a time period of three years were classified according to 11 selected polytrauma definitions and included in our study, if they were rated “polytraumatized” by at least one of these definitions. All patients, who met the criteria of a certain definition, were combined to the relevant definition-positive group, thus resulting in 11 patient subgroups. Their demographic data (number of patients, mean patient age, mean Injury Severity Score value, median number of ventilator days, median length of stay at the intensive care unit and at the hospital, mortality rate and odds ratio) were statistically compared.
Results
Three hundred seventy-five patients (73% male) with a mean age of 47 years met the inclusion criteria and were allocated to the relevant subgroups; their patient number varied from 55 to 346 and their mean Injury Severity Score value ranged from 4 to 75. Not surprisingly, all examined parameters were subject to variations. Whereas most definition-positive groups showed a mortality rate of about 21% to 30%, 18% of the individuals, who met the criteria according to Blacker, and 40% of the polytrauma victims according to Schalamon died. The Pape 1-, Schalamon-, and Berlin-positive groups presented a significant odds ratio with regard to mortality that considerably exceeded 1.
Discussion
A polytrauma definition can only be a reliable tool in classifying trauma victims if it provides a significant odds ratio with regard to mortality that considerably exceeds 1 and if it succeeds in capturing patients with multiple severe injuries and a higher mortality rate without reducing the number of polytraumatized patients to a not representatively small number.
Conclusions
Solely the Berlin definition resulted in a patient number reflecting clinical reality, thus enabling a transparent evaluation of treatment results provided by different institutions and allowing objective comparison of published studies.
Similar content being viewed by others
Background
Worldwide, trauma is an important public health concern. Every year more than 5 million people die from non-intentional traumatic injuries, homicide and suicide, representing 9% of global deaths [1]. Additionally, 20 to 50 million people suffer non-fatal injuries, many of them resulting in disability [2]. The severity of trauma is classified by the Abbreviated Injury Scale (AIS) that was introduced in 1969 and most recently modified in 2008 [3]. In order to quantify the overall severity of multiple injured patients the Injury Severity Score (ISS) was presented in 1974 [4]. It is calculated as the sum of the squares of the highest AIS code in each of the three most severely affected body regions.
Following the initial definition by Tscherne [5] et al, it is generally standard that “polytrauma” denotes multiple and severely injured patients with a high risk of morbidity and mortality, which is higher than the sum of morbidity and mortality of the individual injuries, and with a high risk of cost consuming therapeutic demands. Although this term has been in use for many decades, there is no consensus among clinicians and researchers about the most appropriate definition to identify multiple injured patients with a substantial systemic inflammatory response [6]. A review article, published in 2009, revealed 47 different definitions [7]. They focused on the number of injuries, body regions or organ systems involved [8, 9], pattern or mechanism of injury [10, 11], injuries representing a threat to life [12, 13], ISS [14, 15], and threat to life plus ISS [16]. Since then, even further definitions have been published, wholly or partially based on the AIS [17, 18]. At present, the ISS is used as a standard classification of multiple trauma in the United States, many European countries, and Australia [17].
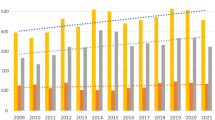
Undoubtedly, a generally accepted polytrauma definition is crucial for scientific and clinical reasons such as the adequate comparison of results that are presented by different research groups as well as for the benchmarking of care. Polytrauma management is highly resource intensive. Due to the present financial situation, economic aspects gain in relevance. In many countries trauma networks are established and specialized centers are graded in different levels according to their infrastructural capacities and a required minimal caseload of polytraumatized patients [19]. Furthermore, critical quality management including objective measurable parameters such as hospital costs per inpatient day, length of stay at the intensive care unit (ICU), or mortality rate has to be based on a clearly specified patient population. As a result of missed standardization, data in regard to mortality rate of multiple injured patients range from 9 to 48% in the previous literature [20,21,22,23]. In order to demonstrate that polytrauma definition and case number are closely connected we exemplarily focused on the annual report of the German Trauma Register DGU® [24]. The official inclusion criteria of this database require patient’s admission to the resuscitation room and a subsequent stay at the ICU, resulting in 38,046 recorded patients in the year 2014. Among these individuals 16,843 met the criterion “ISS ≥ 16”. The addition of one physiological risk factor (age ≥70 years, acidosis, unconsciousness, hypotension, coagulopathy) [19] resulted in 9,486 severely injured. This number was reduced to 4,524 by the application of the additional criterion “two body areas with AIS ≥ 3”. Focusing solely on numbers, a high mortality rate of a certain trauma center may be misinterpreted as the result of insufficient treatment and probably lead to budget cuts or restriction of the provided therapy spectrum. In contrast, a low number of in-hospital deaths may cause unjustified benefits or even inappropriate treatment appraisal.
Therefore, the objective of our study was to point out that polytrauma definitions applied to a specific patient population result in different subgroups of individuals, who in turn present a varying outcome in general with great differences in mortality rate and duration of hospitalization in particular.
Methods
After study approval by our local ethics committee all patients with a minimum age of 18 years, who had been treated at our level I trauma center from January 1, 2009 to December 31, 2011 were classified by 11 well-known and widely used polytrauma definitions [8,9,10,11,12,13,14,15,16,17,18], introduced in Table 1.
Apart from two exceptions [16, 17], the name of the first author of the paper including the respective definition was epynomous. An individual was classified “definition-positive” (for example “McLain-positive”), if he/she met the criteria of the relevant definition; otherwise he/she was deemed “definition-negative”. All definition-positive patients according to a given polytrauma classification were combined to a corresponding polytrauma group, therefore resulting in 11 different patient groups. Statistical analysis was performed using IBM SPSS Statistics 20. For each patient age, ISS value, number of ventilator days, length of stay at the ICU (ICU LOS) and overall length of stay (LOS) were collected and combined to a mean and median value, respectively, as appropriate. The Kolmogorov-Smirnov test was used to check for normal distribution. The Chi-square test was applied to analyze significance of odds ratios. A p-value of <0.05 was considered significant. Data are presented as mean and standard deviation (SD) for normally distributed parameters, as median and interquartile range (IQR) for skew distributions, or as absolute numbers and percentages.
Results
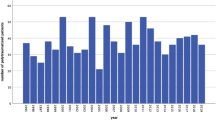
Over the 3-year study period 375 patients (73% male) with a mean age of 47 ± 19.8 years met the inclusion criteria of at least one definition. Of these individuals, the most frequently injured body region was the head (67%), followed by the thorax (53%) and the upper (45%) and lower extremities (45%). 22% died. The ISS values of 31 trauma victims were lower than 16 (see Fig. 1). Of interest, the lowest value of 4 was found in a patient, who suffered fractures in the diaphysis of two long bones of the same extremity. He was included in the study population according to the definition of Pape 2, not requiring an ISS or AIS cut-off value. In 23 patients the highest ISS value of 75 was calculated. Surprisingly, 133 patients (35.5%) did not spend a single day at the ICU; 111 patients (29.6%) were treated there for one to 10 days. Table 2 illustrates relevant data referring to the different definition-positive groups. Patient numbers varied widely.
Noteworthy, all individuals diagnosed as polytrauma victims according to Schalomon were also rated polytraumatized by at least five other classifications. Whereas most definition-positive groups showed a mortality rate of about 21% to 30%, 18% of the individuals, who met the criteria according to Blacker, and 40% of the polytrauma victims according to Schalamon died. Furthermore, there were substantial differences in most corresponding data between the Schalamon-group and the other groups (Table 2). Table 3 displays the odds ratios for mortality. Solely the ratios referring to the Pape 1-, Schalamon-, Sikand- and Berlin-groups significantly exceeded 1, indicating that for those people, who had been classified definition-positive, the odds to die was two to four times higher, respectively, compared to the relevant definition-negative group.
Discussion
To our knowledge this is the first study investigating the influence of 11 different, well-known and widespread polytrauma definitions on patient population and outcome of a single level I trauma center. Depending on the applied definition we revealed widely varying numbers of polytraumatized patients providing major differences in mortality rates and mean ISS values. Unfortunately, some definitions are not spelled out clearly and their concrete application had to be clarified. According to McLain a significant injury “requires hospital admission and active management” [8]. This specification leaves room for subjective interpretation especially in regards to “active management”. Furthermore, the term “life-threatening” is an integral part of four of the applied definitions, although never explained in detail [10, 12, 13, 16]. Because vague phrases are subject to high inter-observer variation comparison of results is difficult in terms of reliability and accuracy. Schalamon’s definition inherently targets the critically injured [12], thus resulting in a small number of patients, presenting a high mortality rate of 40%. The polytrauma definition of Sikand, however, resulted in a more than six time larger patient group with a mortality rate of 23%. The remarkably high (yet statistically not significant) odds ratio referring to mortality has to be interpreted with caution due to the fact that the Sikand-negative group was particularly small, comprising solely individuals with ISS values lower than 16. The low lethality rate and the low ISS values in the group classified according to Blacker were mainly caused by the fact that patients’ admission to the ICU is part of the definition [9]. Because individuals, who died at the trauma resuscitation room had to be excluded polytrauma victims according to Blacker do not represent the actual patient population of a level I trauma center. The same applies to polytrauma definitions solely based on cut-off values (e.g. ISS ≥ 16 or ISS ≥ 18) because they also include individuals with a severe monotrauma (e.g. head trauma) [18]. Undoubtedly, applying such a definition impedes the inter-institutional comparison of mortality and resource utilisation as it fails to discriminate those centers, which treat the most severely injured of the trauma patient population, and eventually leads to an inappropriate budget distribution and use of infrastructural capacities [18]. Using higher ISS cut-off values (e.g. ISS > 20 or ISS > 25) results in an increased specificity but excludes patients with two injuries rated AIS = 3. In general, the exclusive use of an anatomical score ignores the physiological aspects of polytrauma, which are supposed to pose an extremely important additional factor in polytrauma rating [25, 26]. Of the 11 definitions scrutinized here, solely the Berlin definition includes five independent physiologic parameters, which were chosen by a panel of international experts after extensive research. For evaluation of parameter levels all polytraumatized rated patients of the nationwide trauma registry of the DGU were used. Cut-off values for each specific parameter of the Berlin definition were then calculated in such a way that the trauma victims provided a mortality rate of 30%, which is twice as high as the mortality rate of the patient population with an ISS of 16 points [17].
To our opinion a polytrauma definition can only be a reliable tool in classifying trauma victims if it provides a significant odds ratio with regard to mortality that considerably exceeds 1 and if it succeeds in capturing patients with multiple severe injuries and a higher mortality rate without reducing the number of polytraumatized patients to a not representatively small number.
Limitations of this study include the fact that it primarily focuses on mortality, also showing differences in patient number and age, ISS value, number of ventilator days, ICU LOS, and LOS between the 11 definition-positive groups. However, important factors in multiple injured patients such as the risk for major inflammatory complications and multiple organ failure as well as the need of a well-trained multidisciplinary team have not been taken into consideration.
Conclusions
The Berlin definition reflects clinical reality, thus enabling a transparent evaluation of treatment results provided by different institutions, which is indispensable for adequate and reliable benchmarking of care and outcomes.
Abbreviations
- AIS:
-
Abbreviated Injury Scale
- ICU:
-
Intensive care unit
- ISS:
-
Injury Severity Score
References
Injuries and violence: the facts [http://www.who.int/violence_injury_prevention/media/news/2015/Injury_violence_facts_2014/en/]
Road traffic injuries (Fact sheet N°358) [http://www.who.int/mediacentre/factsheets/fs358/en/]
American Association for the Advancement of Automotive Medicine (AAAM): The Abbreviated Injury Scale 2005. Update 2008. Des Plaines, IL 2008
Baker SP, O'Neill B, Haddon WJ, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Tscherne H, Oestern HJ, Sturm JA. Stress tolerance of patients with multiple injuries and its significance for operative care. Langenbecks Arch Chir. 1984;364:71–7.
Butcher NE, Enninghorst N, Sisak K, Balogh ZJ. The definition of polytrauma: variable interrater versus intrarater agreement - a prospective international study among trauma surgeons. J Trauma Acute Care Surg. 2013;74:884–9.
Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40:S12–22.
McLain RF, Benson DR. Urgent surgical stabilization of spinal fractures in polytrauma patients. Spine (Phila Pa 1976). 1999;24:1646–54.
Blacker DJ, Wijdicks EF. Clinical characteristics and mechanisms of stroke after polytrauma. Mayo Clin Proc. 2004;79:630–5.
Pape HC, Zelle B, Lohse R, Stalp M, Hildebrand F, Krettek C, Panzica M, Duhme V, Sittaro NA. Evaluation and outcome of patients after polytrauma - can patients be recruited for long-term follow-up? Injury. 2006;37:1197–203.
Dick WF, Baskett PJ. Recommendations for uniform reporting of data following major trauma--the Utstein style. A report of a working party of the International Trauma Anaesthesia and Critical Care Society (ITACCS). Resuscitation. 1999;42:81–100.
Schalamon J, v Bismarck S, Schober PH, Hollwarth ME. Multiple trauma in pediatric patients. Pediatr Surg Int. 2003;19:417–23.
Zelle BA, Brown SR, Panzica M, Lohse R, Sittaro NA, Krettek C, Pape HC. The impact of injuries below the knee joint on the long-term functional outcome following polytrauma. Injury. 2005;36:169–77.
Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504.
Sikand M, Williams K, White C, Moran CG. The financial cost of treating polytrauma: implications for tertiary referral centres in the United Kingdom. Injury. 2005;36:733–7.
Stürmer KM, Dresnig K, Blauth M, Bonnaire F, Braun W, Meenen NM. Recommended Guidelines for Diagnostics and Therapy in Trauma Surgery. Eur J Trauma Emerg Surg. 2001;27:137–50.
Pape HC, Lefering R, Butcher N, Peitzman A, Leenen L, Marzi I, Lichte P, Josten C, Bouillon B, Schmucker U, et al. The definition of polytrauma revisited: An international consensus process and proposal of the new 'Berlin definition'. J Trauma Acute Care Surg. 2014;77:780–6.
Butcher N, Balogh ZJ. AIS > 2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury. 2012;43:196–9.
Paffrath T, Lefering R, Flohé S, TraumaRegister DGU. How to define severely injured patients? - an Injury Severity Score (ISS) based approach alone is not sufficient. Injury. 2014;45:S64–9.
Bouillon B, Lefering R, Vorweg M, Tiling T, Neugebauer E, Troidl H. Trauma score systems: cologne validation study. J Trauma. 1997;42:652–8.
Oestern HJ, Tscherne H, Sturm J, Nerlich M. Classification of the severity of injury. Unfallchirurg. 1985;88:465–72.
Schweiberer L, Nast-Kolb D, Duswald KH, Waydhas C, Müller K. Polytrauma - treatment by the staged diagnostic and therapeutic plan. Unfallchirurg. 1987;90:529–38.
Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LWJ, Flanagan ME, Frey CF. The Major Trauma Outcome Study: establishing national norms for trauma care. Trauma. 1990;30:1356–65.
Trauma Register DGU: Annual Report 2015 http://www.traumaregister-dgu.de/fileadmin/user_upload/traumaregister-dgu.de/docs/Downloads/TR-DGU-Jahresbericht_2015.pdf.
Butcher NE, Balogh ZJ. The practicality of including the systemic inflammatory response syndrome in the definition of polytrauma: experience of a level one trauma centre. Injury. 2013;44:12–7.
Butcher NE, Balogh ZJ. Update on the definition of polytrauma. Eur J Trauma Emerg Surg. 2014;40:107–11.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
All data that are relevant for the study are included in this published article. Further datasets analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
LLN and TH designed the study. SF and PK analyzed the data, which were interpreted by SF, PK, TH, and LLN. SF and LLN performed the literature review and wrote the manuscript. PK and TH proofread the manuscript and revised it critically. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The present study is in line with the publication guidelines of the Ethics Committee of the Medical University of Vienna and registered as 1387/2012. As patient data are assessed anonymously, individual informed consent is not required.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Frenzel, S., Krenn, P., Heinz, T. et al. Does the applied polytrauma definition notably influence outcome and patient population? – a retrospective analysis. Scand J Trauma Resusc Emerg Med 25, 87 (2017). https://doi.org/10.1186/s13049-017-0400-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-017-0400-2