Abstract
Purpose
To analyze the changes of the clinical characteristics, injury patterns, and mortality rates of polytraumatized patients within the past 25 years in a European Level I trauma center.
Methods
953 consecutive polytraumatized patients treated at a single-level 1 trauma center between January 1995 and December 2019 were enrolled retrospectively. Polytrauma was defined as AIS ≥ 3 points in at least two different body regions. Retrospective data analysis on changes of clinical characteristics and mortality rates over time.
Results
A significant increase of the average age by 2 years per year of the study could be seen with a significant increase of geriatric patients over time. No changes of the median Injury Severity Score (ISS) could be seen over time, whereas the ISS significantly decreased by patient’s year. The rates of concomitant severe traumatic brain injury (TBI) remained constant over time, and did not increase with rising age of the patients. Although, the mortality rate remained constant over time the relative risk of overall in-hospital mortality increased by 1.7% and the relative risk of late-phase mortality increased by 2.2% per patient’s year.
Conclusion
The number of polytraumatized patients remained constant over the 25-year study period. Also, the mortality rates remained stable over time, although a significant increase of the average age of polytraumatized patients could be seen with stable injury severity scores. Severe TBI and age beyond 65 years remained independent prognostic factors on the late-phase survival of polytraumatized patients.
Trial registration: NCT04723992.
Level of evidence: Prognostic study, level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although a decline in trauma-related deaths in adults can be seen over time, trauma remains one of the leading causes of death world-wide [1]. After survival of the acute phase, nearly 80% of the late-phase deaths were due to sepsis and multiple-organ failure (MOF) [2]. Within the last years, the incidence of MOF [3,4,5,6] as well as death rates due to sepsis and acute respiratory distress syndrome (ARDS) in trauma patients [4, 5, 7] showed a significant decrease. A decline of the mortality rates in multiple injured patients was found, especially between the years 1970 and 2000 [4, 5, 8] with a change of the injury patterns of trauma patients: although motor vehicle accidents remain the most common cause of injury [4, 8, 9], a decline in car crashes has been found [4]. Furthermore, an increase in the mean age of polytraumatized patients (reflecting the rapidly aging population world-wide) could be detected in recent studies [9, 10]. The incidence of traumatic brain injury (TBI) in elderly trauma patients has increased over time [11]. Recent studies suggest TBI and rising age as a strong predicting factor for survival in trauma patients [12,13,14,15]. Low-energy trauma is responsible for the late-phase mortality in about 40% of patients with traumatic brain injury as cause of death in about 26% of cases [16]. Severe TBI remains the most common cause of death in trauma patients [17,18,19,20,21,22,23]. Furthermore, concomitant injuries seem to have a significant effect on the mortality in patients with moderate TBI [24]. A recent study was able to demonstrate a markedly decrease in TBI-related mortality in geriatric patients over time [25].
There are few published studies reviewing the changes in trauma mechanisms, injury patterns, and outcome of polytraumatized patients over time [4, 5, 8]. The aim of this study was to integrate the above-mentioned possible prognostic factors in the analysis of a large cohort of adult polytraumatized patients regarding the possible changes over a 25-year period. Therefore, we try to answer the following questions:
-
Does the mean age of polytraumatized patients increase significantly in recent years with an increase of the prevalence of geriatric polytraumatized patients over the past 25 years?
-
Has the prevalence of severe TBI changed over the past 25 years?
-
Can a change of trauma mechanisms with different injury patterns be seen within the past 25 years?
-
Is there a decline in mortality rates of polytrauma patients over time?
Materials and methods
In this study, 952 consecutive patients who were admitted to our level 1 trauma center with critical injuries (ISS ≥ 18 points and an Abbreviated Injury Score (AIS) ≥ 3 points in at least two body regions [26]) were enrolled retrospectively from January 1, 1995 to December 31, 2019.
Exclusion criteria
Patients with an isolated traumatic brain injury, patients with minor injuries (AIS < 3 points or ISS < 18 points), and patients ≤ 16 years of age were excluded from this study.
Three time-dependent events for the analysis of mortality were defined: acute-phase death (death within the first 24 h or on arrival at the hospital), late-phase death (death after the first 24 h within the hospital stay), and overall death (death at any time within the hospital stay).
Patients’ population
Nine-hundred-and-fifty-three consecutive polytraumatized patients were enrolled consecutively from January 1995 to December 2019. The data were gained from our ongoing in-hospital database of polytraumatized patients. Patients’ hospital records were reviewed and the baseline characteristics, such as gender, age, injury mechanism, and injury patterns as well as the outcomes, were reported. Geriatric patients were defined as polytraumatized patients beyond 65 years of age. Severe traumatic brain injury (TBI) was defined as AIS ≥ 3 points in the anatomical region accompanied by a Glasgow Coma Scale (GCS) ≤ 12 points. The combination of anatomical measures such as the AIS with GCS has been suggested and used before [27, 28]. Possible prognostic factors such as severe TBI, age, injury severity (ISS score), and different injury patterns were detected. The follow-up period was counted from the date of trauma to the date of the last known contact.
Statistical analysis
Continuous variables are presented as means and standard deviations or medians and interquartile ranges depending on normal or skew distribution of the certain value. Normal distribution was assessed using the Kolmogorov–Smirnov-test. Categorical variables are provided with percentages. Descriptive statistics were used for demographic variables and clinical characteristics. Trauma mechanism, injury characteristics, and severity of injuries [classified with the injury severity score (ISS)] were examined. For the detection of associations between qualitative variables, a Chi-square test was performed. For the comparison between categorical and continuous variables, the Student’s t test or the Mann–Whitney U test were performed.
Statistical evaluation of changes over the time
To detect time-dependent changes, we created a continuous numerical variable (“day of accident”) for each patient separately (t = 1,2,…) from January 1995 to December 2019. Linear regression analysis was used for numerical variables, and logistic regression analysis was used for categorical variables. For statistical analysis, the variable time in years (day of accident/365.25) was used. A two-sided p value of less than 0.05 was considered to indicate statistical significance. The Kaplan–Meier method was used to provide survival estimates, which were assessed with a log-rank test. For the mortality assessment, three time-dependent events were defined: acute-phase death (within the first 24 h after the trauma), late-phase death (after the acute phase within the hospital stay), and overall survival (death at any time after the trauma). Patients who died of unrelated causes were considered to have been censored. Univariate Cox regression analysis was performed for evaluation of potential prognostic factors on the late-phase survival. Age, severe TBI (AIS ≥ 3 points), and injury severity (ISS score) were included in the univariate Cox regression analysis as potential confounders. Only significant factors (p < 0.05) in the univariate analysis were entered into the multivariate analysis. Stepwise forward multivariate Cox regression analysis was performed for identification of outcome prognosticators. All statistical analyses were performed using IBM SPSS Statistics Version 26.0.
Results
Study population
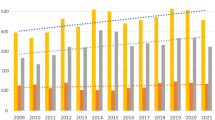
From January 1995 to December 2019, 953 adult polytraumatized patients were enrolled consecutively. The number of polytraumatized patients remained constant over time (linear regression: p = 0.291, Fig. 1). Clinical characteristics are listed in Table 1. Linear regression revealed an increase of age per study year by 2 years on average (p = 0.014). Logistic regression revealed a significant increase of the rates of geriatric (age beyond 65 years) polytraumatized patients over time (HR 1.289; 95% CI 1.020–1.630; p = 0.034) (Fig. 2).
Injury severity, trauma mechanism, and injury pattern
No changes of the injury severity as seen by the ISS could be detected over time (linear regression: p = 0.488), although the ISS decreased significantly with rising age of the patients (linear regression: p = 0.002). No increase in the rates of severe TBI could be seen over time or with rising age of the patients. Traumatic brain injury (TBI) was seen in 66.9% (n = 638) of patients, in whom a severe TBI was detected in 65.7% (n = 419). There was a significant increase of falls from lesser height (< 3 m height) over time (logistic regression: HR 1.550; 95% CI 1.087–2.211, p = 0.015) and of penetrating injuries (logistic regression: HR 1.864; 95% CI 1.133–3.066, p = 0.014). Additionally, a significant change of the injury patterns could be seen with rising age: a significant increase in falls from lesser height (logistic regression: HR 1.051; 95% CI 1.037–1.066, p < 0.001) as well as a significant decrease in falls from greater height (HR 0.987; 95% CI 0.979–0.995, p = 0.002) could be documented with rising age of the patients. Geriatric polytraumatized patients did not show significantly higher rates of severe TBI compared to younger ones (p = 0.420). Falls from lesser height were found significantly more often in the geriatric group of patients as mechanism of injury compared to younger ones (Chi-square: 20.1% vs. 3.9%, p < 0.001).
Mortality and late-phase survival
There was no statistically significant change of the overall, acute-phase, or late-phase mortality over time (Fig. 2). Logistic regression revealed a significant influence of age on the overall mortality (HR 1.017; 95% CI 1.010–1.025, p < 0.001) and on the late-phase mortality (HR 1.026; 95% CI 1.015–1.037, p < 0.001). The relative risk of in-hospital mortality and late-phase mortality increased with rising age of the patients by 1.7% and 2.2% per patient’s year. The injury severity had a significant influence on the overall mortality (HR 1.087; 95% CI 1.073–1.101, p < 0.001) and on the acute-phase mortality (HR 1.117; 95% CI 1.099–1.135, p < 0.001) but not on the late-phase mortality (HR 0.992; 95% CI 0.977–1.008, p = 0.327). Severe TBI (HR 2.737; 95% CI 1.763–4.248; p < 0.001) and age beyond 65 years (HR 2.507; 95% CI 1.666–3.772; p < 0.001) were identified as independent prognostic factors on the late-phase survival after multivariate regression analysis (Figs. 3, 4).
Discussion
Our study contributes several new insights reporting the epidemiology and outcomes of adult polytraumatized patients within the past 25 years.
First, we were able to show a significant increase in the median age of our polytraumatized patients by 2 years in average as well as a significant increase in the rate of geriatric polytraumatized patients within the past 25 years, similar to previous reports [5, 9, 10]. In contrast to that, the injury severity stayed stable over the study period, but showed a significant decrease with rising age of the patients. Although an increase of the incidence of TBI in elderly trauma patients mainly caused by road injuries and falls has been shown [11], the rates of severe TBI remained constant in our study cohort over time.
Second, characteristic changes were seen in our study cohort regarding the injury mechanism of polytraumatized patients. In accordance with the observed changes in the injury patterns, the number of traffic-related accidents in our study cohort decreased significantly within the past 25 years as demonstrated in the previous studies [5, 7]. A significant increase in penetrating injuries (stab wounds and gun-shot wounds) could be seen over time, although penetrating injuries remain uncommon in most European countries [29, 30]. Another remarkable result of our study is a significant increase of polytrauma due to falls from lesser height over time and with rising age of the patients, especially in the geriatric cohort of our polytraumatized patients. These findings might reflect the frailty of this specific patient cohort leading to major trauma despite low-energy trauma as injury pattern.
Third, no significant change of the overall, acute-phase, or late-phase death rates over time could be seen in our study cohort, although reports from the late 90s showed a continuous reduction of mortality in multiple trauma patients [5]. Within the last years, remarkable changes in trauma care systems have been achieved including different transfusion protocols [31] and different pre-hospital treatment strategies [32]. As demonstrated in recent studies, exsanguination is still the predominant cause for acute-phase deaths of polytraumatized patients [33], whereas TBI remains the main cause of death within the late-phase of the trauma [9, 33]. We were able to demonstrate that the injury severity is a significant prognostic factor for the acute-phase survival of polytraumatized patients, whereas, in contrast to that, the rising age of our patients had a significant influence on the overall- and especially the late-phase mortality of our polytraumatized patients. With rising age, the relative risk of overall in-hospital mortality and late-phase mortality increased by 1.7% and 2.2% per patient’s year. In contrast to that, our younger polytraumatized patients tend to die more often within the acute phase. After multivariate analysis, severe TBI and age beyond 65 years were identified as independent prognostic factors in the late-phase survival of polytraumatized patients.
Limitation
This retrospective non-randomized, single-center analysis has the characteristic limitations of registry data and post hoc analyses. There are no data on functional outcome and quality-of-life parameters available. Furthermore, long-term mortality was not evaluated in this study. Due to the retrospective design of this study, there might be an inherent selection bias. The strength of this study and sign of quality is the careful analysis of data in all consecutively included patients.
Conclusion
The number of polytraumatized patients remained constant over the 25-year study period. Also, the mortality rates remained stable over time, although a significant increase of the average age of polytraumatized patients could be seen with stable injury severity scores. Severe TBI and age beyond 65 years remained independent prognostic factors on the late-phase survival of polytraumatized patients.
Taken together, our study demonstrates significant characteristic changes in the demographic variables and clinical characteristics of polytraumatized patients in a European level 1 trauma center over the past 25 years. The lack of improvement in mortality rates could be explained by the constant increase of the median age accompanied by a constant percentage of severe TBI over time reflecting the frail polytraumatized patient.
Availability of data and materials
The data used/analyzed are available from the corresponding author upon reasonable request.
References
Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA, Centers for Disease C et al (2014) CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013. MMWR Suppl 63(4):3–27
Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD (1980) Epidemiology of trauma deaths. Am J Surg 140(1):144–150
Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A (2005) A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg 140(5):432–438 (discussion 8–40)
Regel G, Lobenhoffer P, Grotz M, Pape HC, Lehmann U, Tscherne H (1995) Treatment results of patients with multiple trauma: an analysis of 3406 cases treated between 1972 and 1991 at a German Level I Trauma Center. J Trauma 38(1):70–78
Probst C, Pape HC, Hildebrand F, Regel G, Mahlke L, Giannoudis P et al (2009) 30 years of polytrauma care: an analysis of the change in strategies and results of 4849 cases treated at a single institution. Injury 40(1):77–83
Dewar DC, Tarrant SM, King KL, Balogh ZJ (2013) Changes in the epidemiology and prediction of multiple-organ failure after injury. J Trauma Acute Care Surg 74(3):774–779
van Breugel JMM, Niemeyer MJS, Houwert RM, Groenwold RHH, Leenen LPH, van Wessem KJP (2020) Global changes in mortality rates in polytrauma patients admitted to the ICU-a systematic review. World J Emerg Surg 15(1):55
Di Saverio S, Gambale G, Coccolini F, Catena F, Giorgini E, Ansaloni L et al (2014) Changes in the outcomes of severe trauma patients from 15-year experience in a Western European trauma ICU of Emilia Romagna region (1996–2010). A population cross-sectional survey study. Langenbecks Arch Surg. 399(1):109–26
Weihs V, Heel V, Dedeyan M, Lang NW, Frenzel S, Hajdu S et al (2020) Age and traumatic brain injury as prognostic factors for late-phase mortality in patients defined as polytrauma according to the New Berlin Definition: experiences from a level I trauma center. Arch Orthop Trauma Surg
Aldrian S, Wernhart S, Negrin L, Halat G, Schwendenwein E, Vecsei V et al (2012) Epidemiological and economic aspects of polytrauma management in Austria. Wien Klin Wochenschr 124(3–4):78–84
Injury GBDTB, Spinal Cord Injury C (2019) Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(1):56–87
da Costa LGV, Carmona MJC, Malbouisson LM, Rizoli S, Rocha-Filho JA, Cardoso RG et al (2017) Independent early predictors of mortality in polytrauma patients: a prospective, observational, longitudinal study. Clinics (Sao Paulo) 72(8):461–468
Yucel N, Ozturk Demir T, Derya S, Oguzturk H, Bicakcioglu M, Yetkin F (2018) Potential risk factors for in-hospital mortality in patients with moderate-to-severe blunt multiple trauma who survive initial resuscitation. Emerg Med Int 2018:6461072
Kristiansen T, Lossius HM, Rehn M, Kristensen P, Gravseth HM, Roislien J et al (2014) Epidemiology of trauma: a population-based study of geographical risk factors for injury deaths in the working-age population of Norway. Injury 45(1):23–30
de Vries R, Reininga IHF, de Graaf MW, Heineman E, El Moumni M, Wendt KW (2019) Older polytrauma: mortality and complications. Injury
Evans JA, van Wessem KJ, McDougall D, Lee KA, Lyons T, Balogh ZJ (2010) Epidemiology of traumatic deaths: comprehensive population-based assessment. World J Surg 34(1):158–163
Gennarelli TA, Champion HR, Sacco WJ, Copes WS, Alves WM (1989) Mortality of patients with head injury and extracranial injury treated in trauma centers. J Trauma 29(9):1193–1201 (discussion 201–202)
Roozenbeek B, Lingsma HF, Lecky FE, Lu J, Weir J, Butcher I et al (2012) Prediction of outcome after moderate and severe traumatic brain injury: external validation of the International Mission on Prognosis and Analysis of Clinical Trials (IMPACT) and Corticoid Randomisation After Significant Head injury (CRASH) prognostic models. Crit Care Med 40(5):1609–1617
Di Deo P, Lingsma H, Nieboer D, Roozenbeek B, Citerio G, Beretta L et al (2016) Clinical results and outcome improvement over time in traumatic brain injury. J Neurotrauma 33(22):2019–2025
Rau CS, Wu SC, Chien PC, Kuo PJ, Chen YC, Hsieh HY et al (2017) Prediction of mortality in patients with isolated traumatic subarachnoid hemorrhage using a decision tree classifier: a retrospective analysis based on a trauma registry system. Int J Environ Res Public Health 14(11)
Cnossen MC, Lingsma HF, Tenovuo O, Maas AIR, Menon D, Steyerberg EW et al (2017) Rehabilitation after traumatic brain injury: A survey in 70 European neurotrauma centres participating in the CENTER-TBI study. J Rehabil Med 49(5):395–401
Lingsma H, Andriessen TM, Haitsema I, Horn J, van der Naalt J, Franschman G et al (2013) Prognosis in moderate and severe traumatic brain injury: external validation of the IMPACT models and the role of extracranial injuries. J Trauma Acute Care Surg 74(2):639–646
Lingsma HF, Roozenbeek B, Steyerberg EW, Murray GD, Maas AI (2010) Early prognosis in traumatic brain injury: from prophecies to predictions. Lancet Neurol 9(5):543–554
Leitgeb J, Mauritz W, Brazinova A, Majdan M, Wilbacher I (2013) Impact of concomitant injuries on outcomes after traumatic brain injury. Arch Orthop Trauma Surg 133(5):659–668
Hosomi S, Sobue T, Kitamura T, Ogura H, Shimazu T (2022) Nationwide improvements in geriatric mortality due to traumatic brain injury in Japan. BMC Emerg Med 22(1):24
Butcher N, Balogh ZJ (2012) AIS>2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury 43(2):196–199
Foreman BP, Caesar RR, Parks J, Madden C, Gentilello LM, Shafi S et al (2007) Usefulness of the abbreviated injury score and the injury severity score in comparison to the Glasgow Coma Scale in predicting outcome after traumatic brain injury. J Trauma 62(4):946–950
Bendinelli C, Ku D, King KL, Nebauer S, Balogh ZJ (2020) Trauma patients with prehospital Glasgow Coma Scale less than nine: not a homogenous group. Eur J Trauma Emerg Surg 46(4):873–878
Hundersmarck D, Reinders Folmer E, de Borst GJ, Leenen LPH, Vriens P, Hietbrink F (2019) Penetrating neck injury in two Dutch level 1 trauma centres: the non-existent problem. Eur J Vasc Endovasc Surg 58(3):455–462
Waes OV, Lieshout EV, Silfhout DV, Halm JA, Wijffels M, Vledder MV et al (2020) Selective non-operative management for penetrating abdominal injury in a Dutch trauma centre. Ann R Coll Surg Engl 102(5):375–382
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM et al (2015) Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 313(5):471–482
Thompson L, Hill M, Davies C, Shaw G, Kiernan MD (2017) Identifying pre-hospital factors associated with outcome for major trauma patients in a regional trauma network: an exploratory study. Scand J Trauma Resusc Emerg Med 25(1):83
Callcut RA, Kornblith LZ, Conroy AS, Robles AJ, Meizoso JP, Namias N et al (2019) The why and how our trauma patients die: a prospective Multicenter Western Trauma Association study. J Trauma Acute Care Surg 86(5):864–870
Funding
Open access funding provided by Medical University of Vienna. There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest were declared.
Ethics approval
The local Ethics Committee approved the study protocol. The study was conducted according to the principles expressed in the Declaration of Helsinki.
Consent for publication
The manuscript was approved by all authors for publication.
Informed consent
No informed consent was needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weihs, V., Frenzel, S., Dedeyan, M. et al. 25-Year experience with adult polytraumatized patients in a European level 1 trauma center: polytrauma between 1995 and 2019. What has changed? A retrospective cohort study. Arch Orthop Trauma Surg 143, 2409–2415 (2023). https://doi.org/10.1007/s00402-022-04433-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04433-1