Abstract
Background
Traditional testing of miscarriage products involved culture of tissue followed by G-banded chromosome analysis; this approach has a high failure rate, is labour intensive and has a resolution of around 10 Mb. G-banded chromosome analysis has been replaced by molecular techniques in some laboratories; we previously introduced a QF-PCR/MLPA testing strategy in 2007. To improve diagnostic yield and efficiency we have now updated our testing strategy to a more comprehensive QF-PCR assay followed by array CGH. Here we describe the results from the last 5 years of service.
Methods
Fetal tissue samples and products of conception were tested using QF-PCR which will detect aneuploidy for chromosomes 13, 14, 15, 16, 18, 21, 22, X and Y. Samples that were normal were then tested by aCGH and all imbalance >1Mb and fully penetrant clinically significant imbalance <1Mb was reported.
Results
QF-PCR analysis identified aneuploidy/triploidy in 25.6% of samples. aCGH analysis detected imbalance in a further 9.6% of samples; this included 1.8% with submicroscopic imbalance and 0.5% of uncertain clinical significance. This approach has a failure rate of 1.4%, compared to 30% for G-banded chromosome analysis.
Conclusions
This efficient QF-PCR/aCGH strategy has a lower failure rate and higher diagnostic yield than karyotype or MLPA strategies; both findings are welcome developments for couples with recurrent miscarriage.
Similar content being viewed by others
Background
Around 15% of clinically recognized pregnancies end in miscarriage, usually toward the end of the first trimester [1], and approximately 1% of couples suffer from recurrent miscarriage (defined as three or more consecutive miscarriages). Identifying the cause of pregnancy loss is important for couples and may be critical for the management of their future pregnancies.
Traditional cytogenetic testing of miscarriage products involved culture of chorionic villi or fetal tissue, followed by G-banded chromosome analysis. This approach is labour-intensive and has a significant failure rate, especially when the sample quality is poor; in our laboratory the karyotype failure rate for these samples was approximately 30% [2]. We replaced G-banded chromosome analysis in 2007 with a combined QF-PCR/MLPA approach (samples were tested by QF-PCR for chromosomes 13, 18 21, X and Y followed, in cases with normal results, by MLPA for subtelomeres) [2]. We have now replaced this service with an extended QF-PCR assay (testing chromosomes 13, 14, 15, 16, 18, 21, 22, X and Y) followed in cases with normal results, by array comparative genomic hybridisation (aCGH).
Array analysis is now the method of choice for the identification of chromosome abnormality in postnatal samples. In our laboratory aCGH analysis is the first line test for postnatal samples [3] and for prenatal samples requiring genome-wide copy number analysis following a normal QF-PCR result [4]; ~25,000 postnatal and ~1,000 prenatal samples have been tested. Array CGH-based diagnosis has improved diagnostic yield for both postnatal and prenatal samples. However, the clinical utility of arrays for investigating pregnancy loss is still being established; the extent to which submicroscopic imbalance contributes to pregnancy loss and/or fetal abnormalities is unknown. The application of arrays for testing of fetal tissues was first described in 2004 [5]; since then there have been a limited number of published clinical cohorts [6–11]. Interpreting and reporting copy number variants (CNV) detected by aCGH in miscarriage samples is complex, given potential implications for familial testing and future pregnancies, and best practice has yet to be determined.
In addition, the UK Royal College of Obstetricians and Gyneacologists (RCOG) issued new guidelines in 2011 [12] following a review of the evidence regarding chromosome analysis of couples who suffer recurrent miscarriages [13]. It is now recommended that chromosome analysis should be performed on products of conception (POCs) and fetal tissues rather than parental blood samples. This resulted in an increase in the number of miscarriage samples received, precipitating the need for a high throughput and efficient testing strategy.
Here we describe the results from five years of our QF-PCR/aCGH testing service, including our CNV reporting criteria. This strategy has proven to be an efficient and streamlined method of testing POCs and fetal tissue samples with a lower failure rate and higher abnormality detection rate than previous testing strategies.
Methods
Samples
Nearly all samples were obtained from miscarriage products with a small number obtained from medical terminations or still births. Tested tissue types included chorionic villi, cord, skin, gonad, bone, muscle, lung, liver, spleen and central nervous system. Fetal tissues were always tested in preference to placental tissues, with lowest priority given to tissues from spleen, liver and lung as DNA quality is often poor from these tissues. For some pregnancies (approximately 50%) only placental material was available. The type of tissue tested was given in the report.
Gestation varied from 8 to 40 weeks. Samples where no fetal or placental material (based on morphological analysis) could be categorically identified were reported as ‘unsuitable’ and no further analysis was carried out. DNA was prepared from all samples where fetal or placental material was identified, including samples that were delayed or were macerated and which would not previously have been considered suitable for culture and karyotyping. Cultures were not routinely established.
Testing strategy
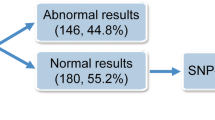
The testing strategy and sample numbers are summarised in Fig. 1. All samples that were not classed as unsuitable were investigated using QF-PCR assays for chromosomes 13, 16, 18, 21, X and Y following QF-PCR for aneuploidy Best Practice Guidelines [14]. Primers for chromosomes 15 and 22 were added to the multiplexes in October 2012, whilst primers for chromosome 14 were added in April 2016. QF-PCR identifies both non-mosaic and mosaic chromosome aneuploidies, molar and triploid pregnancies and maternal cell contamination (MCC). Additional cell lines, such as in cases of mosaicism and MCC, are reliably detected if they contribute at least 20% of the tested cell population. If MCC was present at a significant level (approximately 30%), such that the QF-PCR result could not be confidently interpreted, a second sample was prepared and tested. Abnormal QF-PCR results were reported and in most cases no further testing of the sample was carried out. Samples where QF-PCR detected partial chromosome imbalance were tested by MLPA or aCGH. Parental samples were requested where aneuploidies associated with a possible recurrence risk in future pregnancies were detected. Samples with a normal QF-PCR result went on to be tested using either MLPA (prior to October 2012) or aCGH (October 2012 to present). MLPA is generally considered unable to detect mosaicism whereas aCGH detects mosaicism if present at ≥20% (dependent on quality of DNA).
DNA extraction
Forty milligrams of fetal tissue was roughly chopped or 15 mg chorionic villi was cleaned of any residual maternal decidua; these samples were incubated overnight at 56 °C with proteinase K. DNA was then extracted using a Chemagen DNA extraction robot according to the manufacturer’s instructions (Chemagen, Baesweiler, Germany). DNA was quantified using a Nanodrop spectrophotometer according to the manufacturer’s instructions (Thermo Scientific), and the DNA quality was checked by agarose gel electrophoresis. Samples with completely degraded DNA were tested by QF-PCR only and, if necessary, a second DNA sample was prepared for MLPA/aCGH analysis.
QF-PCR testing and analysis
Amplification of microsatellite markers was carried out as described previously [15]. Details of primer sequences and multiplexes are given in Table 1. Briefly, DNA was amplified using two multiplexes that include a total of 31 markers; assay 1 contains primers for chromosomes 13, 18, 21 and 22, and assay 2, primers for chromosomes 14, 15 and 16 and the X and Y chromosomes. Supplementary markers were used as required. PCR products were separated on an ABI 3100 capillary genetic analyser, and results were analyzed using ABI Genotyper software.
MLPA testing and analysis
All MLPA procedures were carried out as described in Donaghue et al., 2010 [2].
aCGH testing and analysis
DNA samples were labelled using CGH Labelling kit for Oligo Arrays (Enzo Life Sciences, Exeter, UK) and purified by QIA quick PCR purification kit (Qiagen, Manchester, UK) both as per the manufacturer’s instructions. Array CGH was carried out using an oligonucleotide array platform comprising 60,000 probes (Agilent, Wokingham, UK; design ID:028469), as described previously [16]. The arrays were hybridized, washed and scanned using an Agilent scanner, and output from the scanner analysed using Feature Extraction and Genomic Workbench (Agilent) in order to quantify the images and detect CNVs. Agilent ADM-2 algorithm at threshold 6 (with a 3 probe sliding window providing a median detection of 120 kb) was used to call CNVs.
A patient vs patient hybridization strategy was employed where differentially-labelled patients were hybridised against each other. For any detected imbalance, average signal intensity level for each dye was compared with intensities for that region in 10 other samples from the same array run, in order to inform “ownership” of the imbalance. Although any shared imbalance would not be detected, the risk of this was minimised by mismatching phenotypes of hybridization partners where possible and by comparing the signal intensities for each chromosome across the whole array run (typically 48 arrays) to detect any arrays where both hybridization partners carried the same whole chromosome aneuploidy. This strategy provided substantial cost savings.
All CNVs (outside established population polymorphisms) greater than 1 Mb in size were reported. For CNVs smaller than 1 Mb, only those interpreted as of fully penetrant clinical significance or as being associated with fetal abnormalities were reported.
Results
Sample numbers
In the five year period April 2011 to March 2016, 3805 samples, including samples classed as ‘unsuitable’ were received. Figure 2 shows samples numbers received per quarter between April 2011 and March 2016. Period 1 (April 11 - March 12, n = 447) was prior to the implementation of the RCOG guidelines, period 2 (April 12 – March 13, n = 634) was the first year of the new referral criteria and was seen as a consolidation period, whilst for periods 3 (n = 757), 4 (n = 940) and 5 (n = 1027) all referral centres were expected to be referring samples in line with the new RCOG guidelines. This correlated with an increase in sample numbers of 130% between periods 1 and 5.
Unsuitable samples
Three hundred ninety-four (10.4%) of samples were classed as unsuitable where no fetal or placental material was identified by morphological examination. The percentage of samples in periods 1 to 5 were 9.6%, 11.2%, 12.3, 10.2 and 8.8% respectively.
Gestation
Gestation was available for 1126 samples, received between April 11 and March 14. For these samples the mean and median gestational age of samples over this 3 year period was 16 weeks and 14 weeks respectively. The change to the RCOG guidelines correlated with samples from the first trimester increasing from 39 to 52% between periods 1 and 3 (Fig. 3).
Failed tests
0.4% of samples (12/3411) could not be tested due to high levels of maternal cell contamination. QF-PCR analysis failed for a further 0.4% (13/3411) of samples, whilst aCGH failed to give a result for 1.3% of samples (24/1911). The combined failure rate was 1.4% of samples (49/3411).
Reporting times
Using the QF-PCR/aCGH testing strategy, 89% of samples were reported within 28 days; UK guidelines are 90% within 28 days [17]. This compares to 88% reported within 28 days using a QF-PCR/MLPA testing strategy [2].
Abnormalities identified by QF-PCR
In the five year period, 874 of 3411 samples (25.6%) tested by QF-PCR were found to have a chromosome abnormality (see Fig. 4); no further testing of these samples was carried out in most cases. Testing for trisomies 15 and 22 was introduced in October 2012. Overall, trisomy 16 had the highest incidence followed by triploidy and trisomy 21. When abnormalities were detected in placental samples, the possibility of confined placental mosaicism (CPM) was considered and its significance to the miscarriage and/or fetal abnormalities was discussed.
Abnormalities identified by aCGH
One thousand nine hundred-eleven samples that were normal by QF-PCR were tested by aCGH (from a total of 2718 suitable samples in this period). All chromosome imbalances >1 Mb in size were reported. In addition, imbalance <1 Mb in size associated with a fully penetrant phenotype or associated with fetal abnormalities were reported. Using these criteria, chromosome imbalance was detected and reported for 260 samples (9.6% of 2718 samples). See Fig. 5.
aCGH abnormalities >10 Mb, causative of the miscarriage/fetal abnormalities
One hundred ninety-seven (7.2%) samples had abnormalities >10 Mb in size (Table 2); all were considered to be causative of the miscarriage and/or fetal abnormalities. Of these, 155 (5.7%) samples had whole chromosome aneuploidy including six with complex aneuploidy and nine with mosaic aneuploidy. Eighteen samples (0.7%) were found to have an unbalanced genotype indicative of a structural rearrangement; two arose from known parental rearrangements whilst sixteen samples were subsequently found to be derived from balanced parental rearrangements.
aCGH abnormalities <10 Mb, likely causative of the miscarriage/fetal abnormalities
Twenty-five (0.9%) samples had a reported submicroscopic abnormality (Table 3) which were either considered to be or likely to be the cause of the miscarriage and/or fetal abnormalities. These included well characterised syndrome regions eg Di-George (OMIM 188400), Williams (OMIM 194050) and Miller-Dieker syndrome (OMIM 247200) regions as well as smaller imbalances with imbalance of critical genes eg PAFAH1B1 (OMIM 601545) and HCCS (OMIM 300056) genes.
aCGH abnormalities <10 Mb, not causative of the miscarriage/fetal abnormalities but clinically significant
Twenty-four (0.9%) samples had a reported submicroscopic abnormality which were considered to be clinically significant but unrelated to the miscarriage and/or fetal abnormalities (Table 4).
An additional fourteen (0.5%) samples had imbalances >1 Mb of unknown significance.
For all abnormalities with a recurrence risk, parental samples were requested for follow up studies.
Discussion
Identifying the cause of pregnancy loss is important for couples and may have significance for the management of future pregnancies. Around 50% of early pregnancy loss is caused by sporadic chromosome aneuploidy or triploidy following meiotic or postzygotic mitotic error [18]; in these cases, the prognosis for future pregnancies is good. However, where the chromosome complement is normal, other possible reasons for miscarriage (e.g. antiphospholipid syndrome) can be considered.
We report an efficient, cost effective QF-PCR/aCGH testing strategy for POCs and fetal tissues that has a considerably lower failure rate and higher diagnostic yield compared to other approaches. The overall abnormality rate was 35.2%; 33.8% of samples were found to have a chromosome imbalance with associated fully penetrant phenotype, likely to be causative of the miscarriage or fetal abnormalities; 1.8% of these imbalances were submicroscopic (<10 Mb) and would likely not be identified by karyotype analysis. The finding of chromosome imbalance can be used to predict the risk of recurrence of both miscarriage and fetal abnormality as well as providing reasons for pregnancy loss, thus reducing further investigations.
The combined use of QF-PCR and aCGH is also more cost-effective than testing by aCGH alone. 25.6% of samples were found to be abnormal by QF-PCR; with the extended QF-PCR panel now including chromosome 14, this figure will increase. For these cases, the additional expense of the genome-wide test is avoided. In addition, QF-PCR detects triploidy (3.6% of our samples) and molar pregnancies (0.2% of our samples), neither of which are identified by MLPA or aCGH.
QF-PCR is also significantly more robust than either aCGH, MLPA or karyotype analysis; failure rates are found to be 0.4%, 1.3, 5% [2] and 30% [13] respectively. QF-PCR genotyping also identifies and quantifies MCC; an important quality check.
The oligo array platform used has an average resolution of 120 kb; however, due to the lack of data regarding the clinical significance of submicroscopic imbalance in fetal tissues and POCs, a cautious reporting approach was adopted; all imbalance >1 Mb was reported in addition to smaller regions of known fully penetrant clinical significance. In our cohort, 1.5% (40/2718) of samples were found to have a fully penetrant clinically significant submicroscopic (<10 Mb) CNV, whilst 0.3% (9/2718) were found to have a neurosusceptibility CNVs (nsCNV) >1 Mb in size. Other published cohorts found clinically significant submicroscopic imbalance in 0.6% [6], 0.8% [10], 1.6% [8] of samples, although the Levy study [10] included nsCNV and CNVs of unknown significance in this group. The patient vs patient aCGH strategy provides a significant cost reduction compared with patient vs control testing.
Use of the aCGH analysis and reporting strategy described here minimises some of the reporting and counselling complexities caused by CNVs of uncertain significance, and unexpected or incidental findings of incomplete penetrance. Relatively little is known about the genes and pathways involved in miscarriage; many CNVs identified will therefore be classed as of unknown significance and even those that are found to contain genes involved in fetal development will not be useful diagnostically or clinically without further evidence and studies [19]. If reported, CNVs of uncertain significance may require follow-up studies and raise complex counselling and ethical issues particularly regarding recurrence risks. Giving a definitive assessment of clinical significance is not possible and it is important that these results are not over-interpreted. In addition, CNVs that are linked to postnatal phenotypes may be problematic to interpret in the context of fetal abnormalities and recurrent miscarriage; for many genes more data is needed.
Neurosusceptibility CNV (nsCNV) pose further interpretation and ethical issues. As these are associated with neurodevelopmental phenotypes with incomplete penetrance they are unlikely to be the cause of the miscarriage and are therefore unexpected findings. However, as many are inherited, these findings may have clinical implications, unrelated to fetal demise, for the family and any future offspring [20]. Nondisclosure of nsCNVs is widely practised when reporting prenatal results in Europe. Our reporting policy similarly aims to minimise the disclosure of all ambiguous findings; CNVs <1 Mb are only reported if the imbalance causes a known phenotype of complete penetrance or is linked to the pregnancy loss and/or fetal abnormalities.
Imbalances associated with a well-defined and fully penetrant clinical phenotype but which are unrelated to the pregnancy loss or fetal abnormalities are further examples of unexpected findings. These are identified at low frequency; fifteen in this study. For prenatal samples there is a general consensus that if associated with a severe early onset phenotype or late onset treatable condition then these CNVs should be disclosed. A similar strategy could be applied for fetal tissue/POC samples where there is a possible recurrence risk; prenatal diagnosis may be available for future pregnancies. Given the possibility of unexpected findings, pre-test information, counselling and informed consent for aCGH testing is an essential part of the testing process; patients must be provided with information regarding both unexpected and uncertain findings and, if appropriate, nondisclosure of results.
Conclusions
A combined QF-PCR aCGH approach is a cost-effective strategy with a higher diagnostic yield than other approaches; in more cases the cause of the miscarriage is identified and future reproductive risk determined. These outcomes are welcome developments for couples with recurrent miscarriages.
References
ACGS General Genetic Laboratory Reporting Recommendations: http://www.acgs.uk.com/media/949852/acgs_general_genetic_laboratory_reporting_recommendations_2015.pdf Accessed 14th Mar 2017
Gardner RJM, Sutherland GR. Chromosome Abnormalities and Genetic Counseling. 3rd ed. New York: Oxford University Press; 2004. p. 384.
Donaghue C, Mann K, Docherty Z, et al. Combined QF-PCR and MLPA molecular analysis of miscarriage products: an efficient and robust alternative to karyotype analysis. Prenat Diagn. 2010;30(2):133–7.
Ahn JW, Bint S, Bergbaum A, et al. Array CGH as a first line diagnostic test in place of karyotyping for postnatal referrals - results from four years' clinical application for over 8,700 patients. Mol Cytogenet. 2013;6(1):16.
Ahn JW, Bint S, Irving MD, et al. A new direction for prenatal chromosome microarray testing: software-targeting for detection of clinically significant chromosome imbalance without equivocal findings. Peer J. 2014;2:e354.
Schaeffer A, Chung J, Heretis K, et al. Comparative Genomic Hybridization–Array Analysis Enhances the Detection of Aneuploidies and Submicroscopic Imbalances in Spontaneous Miscarriages. Am J Hum Genet. 2004;74:1168–74.
Kooper AJ, Faas BH, Feenstra I, et al. Best diagnostic approach for the genetic evaluation of fetuses after intrauterine death in first, second or third trimester: QF-PCR, karyotyping and/or genome wide SNP array analysis. Mol Cytogenet. 2014;7(1):6.
Bug S, Solfrank B, Schmitz F, et al. Diagnostic utility of novel combined arrays for genome-wide simultaneous detection of aneuploidy and uniparental isodisomy in losses of pregnancy. Mol Cytogenet. 2014;7:43.
Levy B, Sigurjonsson S, Pettersen B, et al. Genomic Imbalance in Products of Conception. Obstet Gynecol. 2014;124(2 Pt 1):202–9.
Lin SB, Xie YJ, Chen Z, et al. Improved assay performance of single nucleotide polymorphism array over conventional karyotyping in analyzing products of conception. J Chin Med Assoc. 2015;78:408–13.
Sahoo T, Dzidic N, Strecker MN, et al. Comprehensive genetic analysis of pregnancy loss by chromosomal microarrays: outcomes, benefits, and challenges. Genet Med. 2017;19(1):83–9.
Wou K, Hyun Y, Chitayat D, et al. Analysis of tissue from products of conception and perinatal losses using QF-PCR and microarray: A three-year retrospective study resulting in an efficient protocol. Eur J Med Genet. 2016;59(8):417–24.
The Royal College of Obstetricians and Gynaecologists website. RCOG GTG17: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg17/ Accessed 14 Mar 2017
Barber JC, Cockwell AE, Grant E, et al. Is karyotyping couples experiencing recurrent miscarriage worth the cost? BJOG. 2010;117(7):885–8.
Association for Clinical Cytogenetics and Clinical Molecular Genetics Society website. http://www.acgs.uk.com/media/765524/acc.cmgs_qfpcr_bp_jan2012_3.01.pdf Accessed 14 Mar 2017
Mann K, Hills A, Donaghue C, et al. Quantitative fluorescence PCR analysis of >40,000 prenatal samples for the rapid diagnosis of trisomies 13, 18 and 21 and monosomy X. Prenat Diagn. 2012;32(12):1197–204.
Ahn JW, Mann K, Walsh S, et al. Validation and implementation of array comparative genomic hybridisation as a first line test in place of postnatal karyotyping for genome imbalance. Mol Cytogenet. 2010;3:9.
Association for Clinical Genetic Science website http://www.acgs.uk.com/media/949852/acgs_general_genetic_laboratory_reporting_recommendations_2015.pdf Accessed 14 March 2017
Ljunger E, Cnattingius S, Lundin C, et al. Chromosomal anomalies in first-trimester miscarriages. Acta Obstet Gynecol Scand. 2005;84(11):1103–7.
Viaggi CD, Cavani S, Malacarne M, et al. First-trimester euploid miscarriages analysed by array-CGH. J Appl Genet. 2013;54(3):353–9.
Rosenfeld JA, Coe BP, Eichler EE, Cuckle H, et al. Estimates of penetrance for recurrent pathogenic copy-number variations. Genet Med. 2013;15(6):478–81.
Acknowledgements
Andrew Bond for export and collation of data from databases.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Authors’ contributions
Testing strategy designed by CO, JWA and KM. Test validation carried out by JWA, HT and CD. Laboratory processing, analysis and reporting of samples was carried out by HT, CD, ND, JWA, KM and CO. Manuscript preparation by CD, KM and CO. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Donaghue, C., Davies, N., Ahn, J.W. et al. Efficient and cost-effective genetic analysis of products of conception and fetal tissues using a QF-PCR/array CGH strategy; five years of data. Mol Cytogenet 10, 12 (2017). https://doi.org/10.1186/s13039-017-0313-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-017-0313-9