Abstract
Background
This study aimed to evaluate trends and predictors of survival after cancer diagnosis in persons living with HIV in the Caribbean, Central, and South America network for HIV epidemiology cohort.
Methods
Demographic, cancer, and HIV-related data from HIV-positive adults diagnosed with cancer ≤ 1 year before or any time after HIV diagnosis from January 1, 2000-June 30, 2015 were retrospectively collected. Cancer cases were classified as AIDS-defining cancers (ADC) and non-AIDS-defining cancers (NADC). The association of mortality with cancer- and HIV-related factors was assessed using Kaplan-Meier curves and Cox proportional hazards models stratified by clinic site and cancer type.
Results
Among 15,869 patients, 783 had an eligible cancer diagnosis; 82% were male and median age at cancer diagnosis was 39 years (interquartile range [IQR]: 32–47). Patients were from Brazil (36.5%), Argentina (19.9%), Chile (19.7%), Mexico (19.3%), and Honduras (4.6%). A total of 564 ADC and 219 NADC were diagnosed. Patients with NADC had similar survival probabilities as those with ADC at one year (81% vs. 79%) but lower survival at five years (60% vs. 69%). In the adjusted analysis, risk of mortality increased with detectable viral load (adjusted hazard ratio [aHR] = 1.63, p = 0.02), age (aHR = 1.02 per year, p = 0.002) and time between HIV and cancer diagnoses (aHR = 1.03 per year, p = 0.01).
Conclusion
ADC remain the most frequent cancers in the region. Overall mortality was related to detectable viral load and age. Longer-term survival was lower after diagnosis of NADC than for ADC, which may be due to factors unrelated to HIV.
Similar content being viewed by others

Background
Since the beginning of the epidemic, human immunodeficiency virus (HIV) and cancer have been intimately linked. People living with HIV have an increased cancer risk in comparison to the general population, not only for AIDS-defining cancers (ADC) but also for several non-AIDS-defining cancers (NADC) including Hodgkin lymphoma, anal cancer, lung cancer, liver cancer and certain skin cancers [1,2,3]. In high-income countries, although ADC were the most prevalent malignancies observed in the early years of the HIV epidemic, NADC increasingly account for cancer morbidity in the era of widespread availability of combined antiretroviral therapy (cART) [4,5,6,7,8,9]. As life expectancy increases for persons living with HIV, long-term exposure to known cancer risk factors such as oncogenic viruses (hepatitis B and C, Epstein Barr [EBV], and human papillomavirus [HPV]) and tobacco, and aging itself have contributed to an increase in the occurrence of NADC [1, 4,5,6]. Particularly in resource-rich countries with broad access to cART, causes of death have similarly shifted from AIDS-related conditions to other diseases [10, 11]. Cancer, particularly NADC, has become one of the most important causes of death in HIV-positive adults receiving cART [4, 7, 9, 12].
Several studies from high-income settings have examined predictors of mortality following cancer diagnosis in adults living with HIV. While cART use is associated with improved survival following ADC, it has not been associated with increased survival following NADC diagnosis [13, 14]. Additionally, CD4 count at cancer diagnosis has been less consistently associated with survival in patients with NADC [13, 15]. Poorer survival following NADC has also been associated with behavioral factors such as intravenous drug use and smoking in HIV cohorts [13, 15]. For some NADC, HIV- positive persons are more likely to be diagnosed at more advanced stage and may be less likely to receive standard chemotherapy compared to their uninfected peers, resulting in worse outcomes [13, 14, 16].
As cART has become increasingly available in Latin America, several studies have shown a growing prevalence of non-AIDS causes of morbidity and mortality, including cancer related deaths [15,16,17,18,19,20]. However, ADC remain frequent, and were the most common cause of cancer observed in a previous study from the region [20, 21]. Survival after cancer diagnosis has been described for resources-rich settings but there is a paucity of data from low- and middle-income countries, including Latin America, where cancer epidemiology and treatments may differ throughout the region [22,23,24,25]. This study aimed to describe cancer frequency and survival among HIV-positive individuals in Latin America. We also aimed to identify HIV clinical factors associated with survival following cancer diagnosis.
Methods
Cohort description and population
The Caribbean, Central and South America Network for HIV Epidemiology (CCASAnet) includes HIV clinical sites from seven countries (Argentina, Brazil, Chile, Haiti, Honduras, Mexico and Peru) and constitutes part of the International Epidemiologic Databases to Evaluate AIDS (IeDEA) [26]. Five sites contributed data to this study – Argentina (Fundación Huésped/Hospital Fernández [FH/HF], Buenos Aires, Argentina); Brazil (Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz, Rio de Janeiro, Brazil); Chile (Fundación Arriarán [FA], Santiago, Chile); Honduras (Instituto Hondureño de Seguridad Social [IHHS] and Hospital Escuela Universitario [HE], Tegucigalpa, Honduras); and Mexico (Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán [INNSZ], Mexico City, Mexico). HIV-positive individuals aged ≥18 years with at least one cancer diagnosis no more than one year before the date of HIV diagnosis or any time after HIV diagnosis and occurring between January 1, 2000 and June 30, 2015 were included in this study. HIV diagnosis date was considered as the reported date of HIV diagnosis, independently from the cancer diagnosis. Patients were excluded if they had an undetectable viral load at cART initiation, suggesting likely inaccurate cART data. Cancer cases were validated and categorized retrospectively as ADC (Kaposi sarcoma, non-Hodgkin lymphoma, invasive cervical cancer) or NADC (all other cancers) according to the CDC definition [27].
Data management
Demographic, clinical, and laboratory data were collected at each site, de-identified, and sent to the CCASAnet Data Coordinating Center at Vanderbilt University (VDCC), Nashville, TN, USA, for data harmonization and processing. The data were checked for internal consistency and missing data, and quality assessments, including onsite audits, were performed. Institutional Ethics Review Boards from all sites and Vanderbilt approved the project, waiving the requirement for individual patient informed consent.
Study outcomes
The primary outcome was time from cancer diagnosis to death due to any cause.
Death was ascertained by different means at the different sites. At IHSS/HE-Honduras, death was recorded when field workers were notified by family members after a call due to patients missing a visit. At all other sites, relatives of patients informed staff of the death (unless it occurred, and was already recorded, at the hospital), and in addition, study staff checked government death registry databases at least annually for subjects lost to follow-up for the FIOCRUZ-Brazil, FA-Chile, and INNSZ-Mexico sites. Patients were considered to be lost to follow- up if their vital status was unknown, and they had no clinical visit within the year prior to the database closing date at their site [28]. Closing dates for the databases were February 11, 2014 for FH/HF-Argentina, January 5, 2015 for FIOCRUZ-Brazil, August 11, 2014 for FA-Chile, October 29, 2015 for IHSS/HE-Honduras, and May 14, 2015 for INNSZ-Mexico.
Statistical analysis
Demographic and clinical characteristics at the time of cancer diagnosis were summarized by site using median (Interquartile Range [IQR]) or percent (frequency), as appropriate.
The association of mortality with potential risk factors was assessed using Kaplan-Meier curves (overall, by cancer type, and by clinic site), log-rank tests, and Cox proportional hazard models, stratified (i.e., separate baseline hazards estimated) by site and type of cancer (ADC or NADC). Unadjusted models as well as multivariable models were fit. Additional analyses fit separate models for ADC and NADC. To investigate whether risk factors for mortality differed by type of cancer, separate analyses included type of cancer as a covariate and examined interaction terms between type of cancer and other predictor variables. Covariates included in the Cox models were selected a priori and included age, CD4 count (square root transformed), and plasma HIV-1 RNA level (VL) dichotomized to detectable versus undetectable using the threshold of 400 copies/mL at the time of cancer diagnosis, sex, timing of the cancer diagnosis relative to cART initiation (before/on vs. after cART initiation), and years from HIV diagnosis to cancer diagnosis. Baseline CD4 count was the closest non-missing value within a window 180 days before to 30 days after the date of cancer diagnosis. Baseline VL was considered the closest non-missing value using a window of 180 days before to 7 days after the date of cancer diagnosis. CD4 was included in models using restricted cubic splines to avoid assuming a linear relationship with the outcome. Missing data were present for CD4 (31%), VL (46%), and years from HIV diagnosis to cancer diagnosis (1.4%). Multiple imputation, using five imputation replications, was used to account for missing data in the multivariable models. All analyses were performed using R statistical software, Version 3.3.0 (https://www.R-project.org). Analysis code is posted at http://biostat.mc.vanderbilt.edu/ArchivedAnalyses.
Results
Among 15,869 eligible adult patients (FH/HF- Argentina: 4912, FIOCRUZ-Brazil: 5807, FA-Chile: 2476, IHSS/HE-Honduras: 1326, INNSZ-Mexico: 1348), 954 (6%) had at least one cancer diagnosis, of which 783 (5%) were eligible for this analysis. Of those patients excluded, 126 were diagnosed with cancer before the year 2000, 23 were diagnosed with cancer on the last day of their follow up, five had inaccurate cART information, 16 had an unknown date of cancer diagnosis, and one had cancer diagnosis at < 18 years old.
Table 1 shows the characteristics of patients with cancer diagnoses overall and by site. In all sites except IHSS/HE-Honduras the majority of the patients were male. Median age at cancer diagnosis was 39 years (IQR 32–47); patients with cancer were older in FIOCRUZ-Brazil and IHSS/HE-Honduras (41 years) and younger in INNSZ-Mexico (34 years). Median time between HIV diagnosis and cancer diagnosis was 1.7 years (IQR 0.2–6.7), ranging from a median of 0.4 years in INNSZ-Mexico to 4.0 years in FIOCRUZ-Brazil. Median time between HIV diagnosis and cART start was 0.5 years (IQR 0.1–3.1), being longer for FIOCRUZ-Brazil (0.6) and FA-Chile (1.0) and shorter for IHSS/HE-Honduras (0.3) and INNSZ-Mexico (0.2). Median CD4 count at cancer diagnosis was 148 cells/μL (IQR 44–364), ranging from 82 cells/μL for patients in FH/HF-Argentina to 190 cells/μL in FIOCRUZ-Brazil. Forty-two percent of the patients were diagnosed with cancer before or concomitant to cART initiation, ranging from 36% in FIOCRUZ-Brazil and IHSS/HE-Honduras to 54% in INNSZ-Mexico. Approximately 4% of patients never started cART. Among the 306 patients on cART at cancer diagnosis with available viral load, 185 (60%) had an undetectable VL (< 400 copies/ml).
As shown in Table 1, 564 of the 783 (72%) cancer cases were ADC, ranging from 66% in FIOCRUZ-Brazil to 82% in FH/HF-Argentina. Overall, Kaposi sarcoma (KS) was the most frequent cancer (48%), followed by non-Hodgkin lymphoma (19%) and cervical cancer (5%). Among NADC, anal cancer (42 cases, 5%) was the most common cancer followed by skin cancer (37 cases, 5%) and Hodgkin lymphoma (23 cases, 3%).
Table 2 compares characteristics of persons diagnosed with ADC and NADC. ADC were more likely to be diagnosed in males than NADC (86% vs 72%). Patients diagnosed with ADC were younger at cancer diagnosis than those diagnosed with NADC (median 37 vs 45 years), had a more recent HIV diagnosis (median 0.8 vs 5.3 years), had spent less time on cART (median 0.0 vs 3.1 years), had lower CD4 count at cancer diagnosis (median 89 vs 376 cells/μL), and were more likely to have a detectable VL (69% vs 30%). A higher percentage of NADC were diagnosed in the later periods of our study (65% of all NADC were diagnosed after 2008 vs. 52% of all ADC). Specifically, 12% (17 of 137), 29% (60 of 210), 32% (83 of 256), and 33% (59 of 180) of the cancers diagnosed during 2000–2003, 2004–2007, 2008–2011 and 2012–2015, respectively, were NADC.
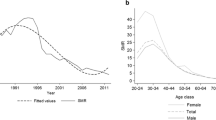
A total of 231 (30%) patients diagnosed with cancer died of any cause during the follow-up period; the median follow-up after cancer diagnosis was 2.5 years (IQR 0.7–6.1). Overall survival probabilities at 1, 3, and 5 years after diagnosis were 80%, 72%, and 67%, respectively. Survival probabilities for those with ADC and NADC are shown in Fig. 1.
Survival was initially higher for those with NADC than ADC, but at the end of one year it was similar (81% vs 79%), and at three and five years it was lower (67% vs 74% and 60% vs 69%, respectively). Overall survival curves did not statistically differ (p = 0.18). Survival after cancer diagnosis differed by site (p < 0.001); at five years it was estimated as 79% for INNSZ-Mexico, 78% for FH/HF-Argentina, 67% for FA-Chile, 56% for FIOCRUZ-Brazil and 49% for IHSS/HE-Honduras (Fig. 2).
Table 3 shows results from univariate and multivariable Cox proportional hazard models assessing associations between patient characteristics at cancer diagnosis and mortality, stratified by cancer type and clinic site. In the unadjusted analyses, patients with lower CD4 count tended to have higher hazards of mortality (18% higher for patients with 100 CD4 cells/μl vs 350 cells/μl), but this association became less pronounced after adjusting for other variables (p = 0.80). In the adjusted analysis, patients with a detectable VL at cancer diagnosis (≥ 400 copies/mL) had a 63% higher hazard of death than patients with an undetectable VL (95% confidence interval [CI] for adjusted hazard ratio [aHR] =1.08–2.47; p = 0.02). Similarly, age at cancer diagnosis and time from HIV diagnosis to cancer diagnosis were also significantly associated with mortality. Risk of mortality increased with age at cancer diagnosis (2% for each year; 95% CI 1.01–1.03; p = 0.002). From the time of HIV diagnosis, cancers diagnosed one year later were associated with a 3% higher hazard of mortality (95% CI 1.01–1.06; p = 0.01).
Results were fairly similar when ADC and NADC were considered separately (Table 4). Detectable viral load at diagnosis of an ADC was associated with an 83% increase in the adjusted hazard of mortality (95% CI 1.03–3.24; p = 0.04). In contrast, a detectable viral load at the time of NADC diagnosis was not associated with a higher hazard of mortality (aHR = 0.98; 95% CI 0.41–2.30; p = 0.96), although these hazard ratios did not statistically differ between ADC and NADC (p = 0.81, test for interaction). In general, there was little evidence that hazard ratios differed between ADC and NADC for any of the patient characteristics considered (p > 0.15 for all variables).
Discussion
In this multisite cohort study of HIV patients diagnosed with cancer across Latin America, we found that age, time since HIV diagnosis, and detectable viral load were predictive of mortality after accounting for cancer type, sex, cART use, and CD4 count. While ADC were the most prevalent cancers diagnosed, an increasing proportion of NADC were diagnosed in more recent years. Despite marked clinical differences in patient characteristics at cancer diagnosis, there was no meaningful difference in survival in the first year after cancer diagnosis for patients diagnosed with ADC versus those diagnosed with NADC, though there was a suggestion that NADC may be associated with increased mortality 3 and 5 years after diagnosis. In this region of low- and middle-income countries, these results reflect the dynamics of cancer epidemiology in HIV positive patients with increasingly available ART and longer life expectancy.
Site was also significantly associated with mortality. This might reflect varying prevalence of the different cancers and differences in access to treatment and care.
We observed an increased hazard of mortality following cancer diagnosis associated with detectable viral load (63% higher than patients with VL < 400 copies/ml); this hazard was particularly higher (83%) for those diagnosed with an ADC. HIV VL has been demonstrated in previous studies to predict mortality in patients diagnosed with ADC, particularly HIV-associated lymphomas [29,30,31]. Virologic suppression has also been associated with improved survival in studies of NADC [31, 32]. In our population, lack of virologic suppression was associated with mortality after cancer diagnosis and was independent of any observed immunologic association with mortality, suggesting that viral control may be a marker of other patient or clinical characteristics associated with improved cancer outcomes rather than the immunologic effect of HIV. In KS, the most frequent ADC in our study, HIV-1 has a direct role in disease pathogenesis, due to pro-oncogenic effects of HIV-1-encoded proteins such as the Tat protein. Tat, a regulatory protein released by HIV-infected cells, protects cells from apoptosis, promotes the growth of spindle cells in synergy with inflammatory cytokines, [33,34,35] and contributes to the intense neoangiogenesis found in KS lesions [36].
Our study did not find that CD4 at the time of cancer diagnosis was predictive of mortality following cancer diagnosis in any of the analyses performed, which differs from studies in high-income settings [32, 37]. Though median CD4 count at cancer diagnosis was significantly lower among patients diagnosed with an ADC versus those diagnosed with a NADC, CD4 count among all patients was very low in our cohort (median 148 cells/μl, IQR: 44–364) and 42% of all the patients were not on cART at cancer diagnosis, suggesting late HIV diagnosis or access to care. The very low CD4 counts among most patients and the fact that the majority had ADC may have limited our ability to detect a meaningful role of immunosuppression and mortality risk. Another possible explanation may be related to the high prevalence of KS, which if diagnosed in early stages and treated, generally has a good prognosis.
Although our study was focused on survival, it also describes cancer epidemiology of HIV-positive adults in the Latin America region. Five percent of patients overall were diagnosed with cancer during the study period; the majority of cases were ADC, and KS was the most frequent. KS incidence is geographically variable, and depends on the prevalence of human herpesvirus-8 infection, the prevalence of HIV, and access to HIV treatment [38, 39]. Our findings are consistent with other studies where ADC were still the most frequent malignancies observed, even in more recent years of the epidemic [20, 21, 40,41,42]. However, many recent reports describe an increasing proportion of cancers due to NADC, and occurring more frequently than ADC, among HIV cohorts [24, 43,44,45,46,47,48]. The most frequent NADC observed in our cohort were anal cancer, Hodgkin disease, and skin cancer, which likely are related to coinfection with oncogenic viruses such as HPV and EBV, and an aging population [24, 49,50,51]. Lung cancer was less frequently observed in our cohort compared to other reports, [24, 52] possibly due to differing patterns of tobacco use, diagnostic capabilities, or case ascertainment, which needs further exploration. Anal cancer was more frequent in FIOCRUZ- Brazil and INNSZ-Mexico; possibly related to more frequent anal cancer screening practices. These trends will probably continue to change as HIV-positive individuals live longer and antiretroviral therapy is started earlier. Of note, a high number of testis cancer was found in FA-Chile. Data from the general population show that Chile has a higher incidence of testis cancer (age- standardized rate 6.8 per 100,000 population) than the other countries participating in the study (ranging from 0.4 in Honduras to 5 per 100,000 population in Argentina) [53]. Further investigation will be needed to determine whether there are particular associated factors in the HIV-positive population.
Across our region, cancer trends and mortality differed, likely reflecting differences in access to cART and HIV care historically. For example, FIOCRUZ-Brazil (which has had cART universally available since 1996) had the highest proportion of incident NADC diagnosed as well as high mortality following cancer diagnosis. Indeed, some studies from high-income settings with broad access to cART have also observed higher mortality for NADC than for ADC [22]. One important risk factor for incidence of and mortality after NADC is increasing age, an observation we also found in our study [32]. Older age alone has been associated with increased mortality in HIV and may be associated with poor response to HIV or cancer treatment or accumulation of other co-morbidities. Taken together, these findings underscore the epidemiologic changes observed in high-income settings of increased NADC incidence and mortality among an aging cohort of HIV patients that is also occurring in Latin America.
Lastly, our study is novel in its reporting of long term survival following cancer diagnosis in HIV patients in Latin America and showed important differences from what has been reported in high-income settings. Overall survival following cancer diagnosis in our study at one, three, and five years was 80%, 73%, and 68% respectively. In contrast, the five-year survival after cancer diagnosis was 54.5% following ADC diagnosis and approximately 65% following NADC diagnosis in the HIV Outpatient Study in the US [31]. Worm et al. reported five-year survival of 52.7% following NADC diagnosis in the D:A:D study [24]. These differences may be due to differences in specific types of cancers diagnosed (for instance, low rates of lung cancer observed in our cohort), patient characteristics (such as CD4 nadir or presence of co-infections, not included in our analysis), cancer treatment availability, or death ascertainment. Our study importantly adds to the understanding of cancer outcomes in HIV patients globally, including those from settings of limited resources and high prevalence of ADC.
There are limitations to our study to consider. First, though misclassification is a concern for any observational study, CCASAnet has gone to great lengths to maintain a high level of data quality including on-site audits of observational data collected [54]. It is possible that some cancer cases may be undiagnosed and therefore not included in this study due to differential rates of cancer screening or diagnosis. Second, our analysis was limited by high rates of missing laboratory data. This was addressed by multiple imputation in our analyses but is a common challenge for observational data in resource-limited settings. Third, other factors known to predict cancer outcomes were not included in this study, including cancer stage at diagnosis, cancer treatment, and smoking. Some studies from the US have suggested that HIV patients with cancer are less likely to receive appropriate cancer treatments compared to uninfected patients [55]. We did not have complete information available regarding cancer treatment received by patients and how this may differ by clinical site or patient characteristics such as cART use or immune status. Fourth, due to relatively low numbers of individual NADC diagnoses, we grouped the cancer diagnoses into ADC and NADC categories. Cancers are a heterogeneous mix of diseases and this approach, and the moderate numbers of events, may have limited our ability to detect clinical predictors of outcomes related to specific cancer diagnoses. Fifth, cancers diagnosed up to one year before the HIV diagnosis were included. It is probable that patients with ADC were more likely to be tested for HIV than patients with NADC, so there might be an under- representation of HIV patients with NADC in our cohort. Lastly, some studies have shown worse outcomes of NADC in HIV-positive people compared to the general population [1]. Our analysis lacks an HIV-uninfected population with which to compare survival outcomes following cancer diagnosis to evaluate the question of whether HIV patients in our region have comparably different outcomes than uninfected cancer patients.
Conclusions
As one of the first studies to describe survival after cancer diagnosis in HIV-positive individuals from Latin America, this study provides valuable information to be used at the local level and shows the need of continuing investigation of cancer epidemiology to establish effective prevention and screening policies in this region. Future work will be strengthened by increasing observation time as patients with HIV and cancer live longer, incorporating additional information about specific cancer therapies in the region, and utilizing regional national cancer registries that may improve ascertainment and allow for comparisons with the general populations.
References
Coghill AE, Engels EA. Are cancer outcomes worse in the presence of HIV infection? Cancer Epidemiol Biomark Prev. 2015;24(8):1165–6.
Patel P, Hanson DL, Sullivan PS, et al. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Ann Intern Med. 2008;148(10):728–36.
Silverberg MJ, Chao C, Leyden WA, et al. HIV infection and the risk of cancers with and without a known infectious cause. AIDS. 2009;23(17):2337–45.
Bonnet F, Burty C, Lewden C, et al. Changes in cancer mortality among HIV-infected patients: the Mortalite 2005 survey. Clin Infect Dis. 2009;48(5):633–9.
Franceschi S, Lise M, Clifford GM, et al. Changing patterns of cancer incidence in the early- and late-HAART periods: the Swiss HIV cohort study. Br J Cancer. 2010;103(3):416–22.
Powles T, Robinson D, Stebbing J, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol. 2009;27(6):884–90.
Raffetti E, Albini L, Gotti D, et al. Cancer incidence and mortality for all causes in HIV-infected patients over a quarter century: a multicentre cohort study. BMC Public Health. 2015;15:235.
Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst. 2011;103(9):753–62.
Vandenhende MA, Roussillon C, Henard S, et al. Cancer-related causes of death among HIV-infected patients in France in 2010: evolution since 2000. PLoS One. 2015;10(6):e0129550.
Brickman C, Palefsky J. Cancer in the HIV-Infected Host: Epidemiology and Pathogenesis in the Antiretroviral Era. Curr HIV/AIDS Rep. 2015;12:388–96.
Lewden C, Salmon D, Morlat P, et al. Causes of death among human immunodeficiency virus (HIV)-infected adults in the era of potent antiretroviral therapy: emerging role of hepatitis and cancers, persistent role of AIDS. Int J Epidemiol. 2005;34(1):121–30.
Simard EP, Engels EA. Cancer as a cause of death among people with AIDS in the United States. Clin Infect Dis. 2010;51(8):957–62.
Sigel K, Crothers K, Dubrow R, et al. Prognosis in HIV-infected patients with non-small cell lung cancer. Br J Cancer. 2013;109(7):1974–80.
Spano JP, Massiani MA, Bentata M, et al. Lung cancer in patients with HIV infection and review of the literature. Med Oncol. 2004;21(2):109–15.
Pacheco AG, Tuboi SH, Faulhaber JC, et al. Increase in non-AIDS related conditions as causes of death among HIV-infected individuals in the HAART era in Brazil. PLoS One. 2008;3(1):e1531.
Grinsztejn B, Luz PM, Pacheco AG, et al. Changing mortality profile among HIV-infected patients in Rio de Janeiro, Brazil: shifting from AIDS to non-AIDS related conditions in the HAART era. PLoS One. 2013;8(4):e59768.
Luz PM, Bruyand M, Ribeiro S, et al. AIDS and non-AIDS severe morbidity associated with hospitalizations among HIV-infected patients in two regions with universal access to care and antiretroviral therapy, France and Brazil, 2000-2008: hospital-based cohort studies. BMC Infect Dis. 2014;14:278.
Cobucci RN, Lima PH, de Souza PC, et al. Assessing the impact of HAART on the incidence of defining and non-defining AIDS cancers among patients with HIV/AIDS: a systematic review. J Infect Public Health. 2015;8(1):1–10.
Fazito E, Vasconcelos AM, Pereira MG, et al. Trends in non-AIDS-related causes of death among adults with HIV/AIDS, Brazil, 1999 to 2010. Cad Saude Publica. 2013;29(8):1644–53.
Castilho JL, Luz PM, Shepherd BE, et al. HIV and cancer: a comparative retrospective study of Brazilian and U.S. clinical cohorts. Infect Agent Cancer. 2015;10:4.
Fink VI, Shepherd BE, Cesar C, et al. Cancer in HIV-infected persons from the Caribbean, central and South America. J Acquir Immune Defic Syndr. 2011;56(5):467–73.
Gotti D, Raffetti E, Albini L, et al. Survival in HIV-infected patients after a cancer diagnosis in the cART era: results of an italian multicenter study. PLoS One. 2014;9(4):e94768.
Hleyhel M, Belot A, Bouvier AM, et al. Trends in survival after cancer diagnosis among HIV-infected individuals between 1992 and 2009. Results from the FHDH-ANRS CO4 cohort. Int J Cancer. 2015;137(10):2443–53.
Worm SW, Bower M, Reiss P, et al. Non-AIDS defining cancers in the D:a:D study--time trends and predictors of survival: a cohort study. BMC Infect Dis. 2013;13:471.
Narayan KM, Miotti PG, Anand NP, et al. HIV and noncommunicable disease comorbidities in the era of antiretroviral therapy: a vital agenda for research in low- and middle-income country settings. J Acquir Immune Defic Syndr. 2014;67(Suppl 1):S2–7.
McGowan CC, Cahn P, Gotuzzo E, et al. Cohort profile: Caribbean, central and South America network for HIV research (CCASAnet) collaboration within the international epidemiologic databases to evaluate AIDS (IeDEA) programme. Int J Epidemiol. 2007;36(5):969–76.
Selik RM, Mokotoff ED, Branson B, et al. Revised Surveillance Case Definition for HIV Infection — United States, 2014. Morb Mortal Wkly Rep. 2014;63(RR 03):1–10.
Carriquiry G, Fink V, Koethe JR, et al. Mortality and loss to follow-up among HIV-infected persons on long-term antiretroviral therapy in Latin America and the Caribbean. J Int AIDS Soc. 2015;18:20016.
Gopal S, Patel MR, Yanik EL, et al. Temporal trends in presentation and survival for HIV-associated lymphoma in the antiretroviral therapy era. J Natl Cancer Inst. 2013;105(16):1221–9.
Gopal S, Patel MR, Yanik EL, et al. Association of early HIV viremia with mortality after HIV-associated lymphoma. AIDS. 2013;27(15):2365–73.
Patel P, Armon C, Chmiel JS, et al. Factors associated with cancer incidence and with all-cause mortality after cancer diagnosis among human immunodeficiency virus-infected persons during the combination antiretroviral therapy era. Open Forum Infect Dis. 2014;1(1):ofu012.
Achenbach CJ, Cole SR, Kitahata MM, et al. Mortality after cancer diagnosis in HIV-infected individuals treated with antiretroviral therapy. AIDS. 2011;25(5):691–700.
Barillari G, Sgadari C, Fiorelli V, et al. The tat protein of human immunodeficiency virus type-1 promotes vascular cell growth and locomotion by engaging the alpha5beta1 and alphavbeta3 integrins and by mobilizing sequestered basic fibroblast growth factor. Blood. 1999;94(2):663–72.
Cheung MC, Pantanowitz L, Dezube BJ. AIDS-related malignancies: emerging challenges in the era of highly active antiretroviral therapy. Oncologist. 2005;10(6):412–26.
Ensoli B, Sturzl M, Monini P. Cytokine-mediated growth promotion of Kaposi's sarcoma and primary effusion lymphoma. Semin Cancer Biol. 2000;10(5):367–81.
Impola U, Cuccuru MA, Masala MV, et al. Preliminary communication: matrix metalloproteinases in Kaposi's sarcoma. Br J Dermatol. 2003;149(4):905–7.
Collaboration of Observational HIV Epidemiological Research Europe (COHERE) study group, Bohlius J, Schmidlin K, et al. Prognosis of HIV-associated non-Hodgkin lymphoma in patients starting combination antiretroviral therapy. AIDS. 2009;23(15):2029–37.
Bohlius J. AIDS-defining Cancer project working group for IeDEA and COHERE in EuroCoord; AIDS-defining Cancer project working group for IeDEA and COHERE in EuroCoord, Comparison of Kaposi sarcoma risk in HIV-positive adults across five continents: a multiregional multicohort study. Clin Infect Dis. 2017;65(8):1316-26.
Rohner E, Wyss N, Heg Z, et al. HIV and human herpesvirus 8 co-infection across the globe: systematic review and meta-analysis. Int J Cancer. 2016;138(1):45–54.
Laurido M, Uruena A, Vizzotti C, et al. Incidence variation in malignancies associated or not with AIDS at an outpatient care center, 1997-2005. Medicina (B Aires). 2007;67(3):243–6.
Zohar M, Micha B. Cancer incidence in people living with HIV/AIDS in Israel, 1981-2010. AIDS Res Hum Retrovir. 2015;31(9):873–81.
Sachdeva RK, Sharma A, Singh S, et al. Spectrum of AIDS defining & non-AIDS defining malignancies in North India. Indian J Med Res. 2016;143(Supplement):S129–35.
Dryden-Peterson S, Medhin H, Kebabonye-Pusoentsi M, et al. Cancer incidence following expansion of HIV treatment in Botswana. PLoS One. 2015;10(8):e0135602.
Chen M, Jen I, Chen YH, et al. Cancer incidence in a Nationwide HIV/AIDS patient cohort in Taiwan in 1998-2009. J Acquir Immune Defic Syndr. 2014;65(4):463–72.
Chiu CG, Smith D, Salters KA, et al. Overview of cancer incidence and mortality among people living with HIV/AIDS in British Columbia, Canada: implications for HAART use and NADM development. BMC Cancer. 2017;17(1):270.
Riedel DJ, Stafford KA, Vadlamani A, et al. Virologic and immunologic outcomes in HIV-infected patients with Cancer. AIDS Res Hum Retrovir. 2017;33(5):482–9.
Tanaka LF, Latorre MR, Gutierrez EB, et al. Risk for cancer among people living with AIDS, 1997-2012: the Sao Paulo AIDS-cancer linkage study. Eur J Cancer Prev.2017; 00:000–000.
Yang J, Su S, Zhao H, et al. Prevalence and mortality of cancer among HIV-infected inpatients in Beijing, China. BMC Infect Dis. 2016;16:82.
Clifford GM, Polesel J, Rickenbach M, et al. Cancer risk in the Swiss HIV cohort study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst. 2005;97(6):425–32.
Crum-Cianflone N, Hullsiek KH, Marconi V, et al. Trends in the incidence of cancers among HIV-infected persons and the impact of antiretroviral therapy: a 20-year cohort study. AIDS. 2009;23(1):41–50.
Engels EA, Biggar RJ, Hall HI, et al. Cancer risk in people infected with human immunodeficiency virus in the United States. Int J Cancer. 2008;123(1):187–94.
Silverberg MJ, Lau B, Achenbach CJ, et al. Cumulative incidence of Cancer among persons with HIV in North America: a cohort study. Ann Intern Med. 2015;163(7):507–18.
International Agency for Research in Cancer. Globocan 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. 2012 [Accessed 2018 06 Apr 2018]; Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
Duda SN, Shepherd BE, Gadd CS, et al. Measuring the quality of observational study data in an international HIV research network. PLoS One. 2012;7(4):e33908.
Suneja G, Boyer M, Yehia BR, et al. Cancer treatment in patients with HIV infection and non-AIDS-defining cancers: a survey of US oncologists. J Oncol Pract. 2015;11(3):e380–7.
Acknowledgements
We gratefully acknowledge all patients, caregivers, and data managers involved in the CCASAnet cohort. We also thank the Infectious Diseases Unit, Hospital Fernández, Buenos Aires, Argentina.
Fundings
This work was funded by the NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (leDEA) (U01AI069923). This award is funded by the following institutes: Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), Office Of The Director, National Institutes Of Health (OD), National Institute Of Allergy And Infectious Diseases (NIAID), National Cancer Institute (NCI), and the National Institute Of Mental Health (NIMH).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Complete data for this study cannot be posted in a supplemental file or a public repository because of legal and ethical restrictions. The Principles of Collaboration under which the CCASAnet multi-national collaboration was founded and the regulatory requirements of the different countries’ IRBs require the submission and approval of a project concept sheet by the CCASAnet executive committee and the principal investigators at participating sites. All datasets provided are de-identified according to HIPAA Safe Harbor guidelines. Disclosure of a person’s HIV status can be highly stigmatizing, and since re-identification of de-identified datasets may be possible when they are combined with publicly available datasets, we promote the signing of a Data Use Agreement before HIV clinical data can be released. To request data, readers may contact Dr. Catherine McGowan (c.mcgowan@vanderbilt.edu) for consideration and instructions. We confirm that the anomyzed dataset will be made available to researchers upon request.
Author information
Authors and Affiliations
Consortia
Contributions
VIF, CAJ, JC, BES, CMG and PC made substantial contributions to the conception and design of the study, VIF, AKP, BG, JN, BC, CC, DP, and PC acquired the data; VIF, CKJ, BES and KJ made substantial contribution to the interpretation of the data. CKJ and BES analyzed it. VIF, CKJ, JC, BES, CMG and PC drafted the article; all authors revised it critically for important intellectual content approved the final version for publishing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Ethics Review Boards from all sites (IRB00002014- Comité de Bioética Fundación Huésped IRB -Argentina-; IRB00004170- Comite - CEP IPEC -Brazil-; IRB00011115- Comité Ético Científico Servicio de Salud Metropolitano Central IRB–Chile-, IRB00003070- Unidad de Investigacion Cientifica IRB – Biomedical–Honduras-, IRB00001910- Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran IRB -Mexico) and IRB00000475- Vanderbilt University Health Science Committee IRB - approved the project, waiving the requirement for individual patient informed consent.
Competing interests
The authors declare that they have no conflicts of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fink, V.I., Jenkins, C.A., Castilho, J.L. et al. Survival after cancer diagnosis in a cohort of HIV-positive individuals in Latin America. Infect Agents Cancer 13, 16 (2018). https://doi.org/10.1186/s13027-018-0188-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-018-0188-3