Abstract
Purpose
Our aim was to describe non-AIDS-defining cancer (NADC) mortality among people living with HIV (PLWH), to compare it with that of the general population, and to assess potential risk factors.
Methods
We included antiretroviral-naive PLWH from the multicentre CoRIS cohort (2004–2021). We estimated mortality rates and standardised mortality ratios (SMRs). We used cause-specific Cox models to identify risk factors.
Results
Among 17,978 PLWH, NADC caused 21% of all deaths observed during the follow-up. Mortality rate due to NADC was 1.58 (95%CI 1.36, 1.83) × 1000 person-years and lung and liver were the most frequent cancer-related causes of death. PLWH had 79% excess NADC mortality risk compared to the general population with the highest SMR found for Hodgkin lymphoma, anal and liver cancers. The SMRs decreased with age and were the highest in age groups under 50 years. The most important prognostic factor was low CD4 count, followed by smoking, viral hepatitis and HIV transmission through heterosexual contact or injection drug use.
Conclusion
Non-AIDS cancers are an important cause of death among PLWH. The excess mortality related to certain malignancies and the association with immunodeficiency, smoking, and coinfections highlights the need for early detection and treatment of cancer in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancers account for a considerable proportion of morbidity and mortality among people living with HIV (PLWH) (Engels et al. 2017). With the widespread use of effective combination antiretroviral therapy (ART), there was a shift in the predominant types of cancers that affect this population, from AIDS-defining cancers, which include those related to advanced immunodeficiency that characterise AIDS (Kaposi’s sarcoma, non-Hodgkin lymphoma, and invasive cervical cancer) to non-AIDS–defining cancers (NADC) (Shiels and Engels 2017).
During the last decades, mortality rates in PLWH have decreased for many causes of death, including AIDS cancers, while NADC mortality has remained constant (Weber et al. 2013; Smith et al. 2014) becoming one of the leading causes of death in PLWH (Croxford et al. 2017; Yuan et al. 2022). Meanwhile, ART has improved its effectiveness, cancer prevention and control have increased due to the human papillomavirus (HPV) vaccine and hepatitis C virus (HCV) treatment as well as screening and prevention campaigns, and, finally, treatment strategies for cancer have evolved. In this setting, quantifying and monitoring cancer mortality trends in PLWH are essential to understand its evolution and the underlying risk factors with the final aim of highlighting targeted priorities in care and prevention. In Spain, NADC mortality was three times higher among PLWH than the general population during the years 1999–2006 (Aldaz et al. 2011), but data on recent mortality trends over time are lacking or only limited to the regional level (López et al. 2016).
Factors potentially contributing to increasing incidence of NADC among PLWH include traditional cancer risk factors, such as aging and smoking, among others, as well as HIV-dependent risk factors (including length of HIV infection and immunosuppression, (Clifford et al. 2005) co-infections with HPV, hepatitis B virus (HBV) or HCV, (Picard et al. 2016; Hu et al. 2019) immune system activation and chronic inflammation (Tenorio et al. 2014)). However, there is little evidence on specific risk factors for NADC mortality among PLWH, and the few studies that have investigated them (Bonnet et al. 2004; d’Arminio et al. 2008; Leierer et al. 2021) have not considered multiple risk factors including HIV-related and -unrelated. The only study that investigated risk factors for cancer mortality among PLWH that considered both traditional and HIV-related risk factors was limited to the years 1998–2001 (d’Arminio et al. 2008).
The aims of this study were to describe NADC mortality and its temporal trends among PLWH, to compare them with those in the general population, and to assess potential risk factors during the years 2004 to 2021.
Materials and methods
Study population
CoRIS is an open, prospective, multicentre cohort of confirmed HIV-positive individuals. Participants are ART-naive at study entry, recruited in 47 clinical centres from 14 of the 17 autonomous regions in Spain from 2004 onwards. In brief, CoRIS collects a dataset including baseline and follow-up sociodemographic, immunological and clinical data. Data are highly standardized and submitted to periodic quality control procedures. Participants are followed up periodically following routine clinical practice (Sobrino-Vegas et al. 2011).
For this study, we included antiretroviral-naïve individuals aged ≥ 20 years at enrolment and with at least one day of follow-up, recruited from January 1st, 2004 to November 30th, 2021, which was considered as administrative censoring date.
All patients agree to participate in CoRIS by signing an informed consent form. The CoRIS cohort was approved by the Clinical Research Ethics Committee of the Gregorio Marañón General University Hospital. This study was approved by the Carlos III Institute Research Ethics Committee (PI 05_2019) and was performed in accordance with the Declaration of Helsinki.
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Outcomes
The main outcome was death due to NADC. We also considered the following endpoints: viral and nonviral NADC mortality, mortality due to lung cancer and mortality due to liver cancer. Deaths were ascertained through cohort reporting, classified using revised CoDe, which is a simplified version of CoDe coding system that has been proposed by the Antiretroviral Therapy Cohort Collaboration (Zwahlen et al. 2009), which has been previously applied to CoRIS (Hernando et al. 2012).
According to different pathogenesis and risk factors, we further categorized NADC deaths as viral, nonviral, and other (Hernández-Ramírez et al. 2017). Viral NADC deaths included those due to cancers of the anus and penis which are related to HPV; liver cancer, which is associated with HBV and HCV; Hodgkin’s lymphoma, which is related to Epstein–Barr virus; and Merkel cell carcinoma, which is associated with Merkel cell polyomavirus. Cancers of vagina/vulva and oral cavity/pharynx, which are caused by HPV, were categorized together with other nonviral cancers (such as gynaecological or head and neck cancers) in the database. Since they could not be classified as viral or nonviral NADC, gynaecological, head and neck as well as cancers of unknown primary site were classified as ‘other’.
Statistical analyses
We estimated 5-years age group- and sex-specific annual mortality rates as the number of deaths due to NADC by 1000 person-years of follow-up with 95% confidence intervals (CIs) based on the normal approximation of the logarithm of the rates. Follow-up of individuals began on the date of enrolment to the date of death, last visit or administrative censoring date, whichever came first.
To compare the cohort mortality to that of the general population, we estimated age-and sex-specific annual Standardized Mortality Ratios (SMR), defined as the ratio of observed to expected deaths according to mortality among the general population. Expected deaths were obtained by applying calendar year, sex- and age-specific (in 5-years bands) mortality rates for the general population to the person-years of follow-up of the CoRIS cohort. We obtained the annual cause-specific mortality rates for the general population from the National Statistics Institute (www.ine.es) during 2004–2021. We performed a test for trend by including age or period as a continuous variable and a test for interaction by including sex as an interaction term, both in a Poisson regression model. We finally obtained age-, sex- and period-(2004–2006, 2007–2010, 2011–2013, 2014–2017, 2018–2021) specific rates and SMR. We chose the year 2014 as one of the cut-off points because it was in that year when the Spanish antiretroviral treatment guidelines changed to recommend initiation of ART regardless of the CD4 cell count.
We estimated mortality rate ratios (MRR) for mortality due to all NADC, viral, nonviral NADC, lung and liver cancers, using cause-specific Cox proportional hazard models (to account for competing risk events), with age as timescale. We estimated robust standard errors to account for clustering of participants within centres. In each model we included a set of baseline and time-updated variables as potential prognostic factors. Baseline variables were sex at birth (male, female), transmission route (males having sex with other males [MSM], injecting drug use [IDU], heterosexual contact, other/unknown), educational level (no/primary education, secondary education, university, other/unknown), region of origin (Europe, Sub-Saharan Africa, Latin America, other/unknown) and AIDS diagnosis at enrolment. Time-updated variables were CD4 T-cell count (< 200, 201–349, 350–499, ≥ 500 cells/µL, unknown), presence of HCV antibodies (no, yes or unknown) or hepatitis B surface antigen (no, yes or unknown), CD4/CD8 ratio (≤ 0.4, > 0.4, unknown), viral load (< 50, 51–10,000, 10,000–100,000, ≥ 100,000 copies/mL, unknown) and smoking status (never, ex-, current smoker, unknown).
Statistical analyses were performed using R version 4.2 (R Core Team 2020).
Results
Among the 18,573 participants included in CoRIS by November 2021, 17,978 met inclusion criteria: 85.5% of them were men, the majority was from Spain (55.2%) and the most frequent mode of HIV acquisition was MSM (62.6%) (Table 1). At enrolment, median age was 35 years, 33.4% subjects had CD4 T-cell count ≥ 500 cells/µL, and 12.4% had an AIDS diagnosis. Among subjects with known smoking status, 5,357 (44.0%) were active smokers.
Mortality rates due to NADC
We observed that 176 of the 851 (20.7%) deaths registered during the study period were due to NADC: of these, 31 were due to a viral (17.6%), 125 (71.0%) were due to a nonviral cancer and 20 (11.4%) were due to other cancers. Mortality rates and SMR due to all and specific NADC are shown in Table 2.
NADC mortality rate was 1.58 (95% 1.36, 1.83): the highest mortality rates were found for lung and liver cancer.
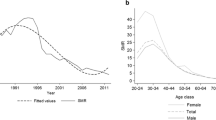
Mortality rates due to both viral and nonviral cancers were similar by sex (P-value for interaction, [Pint] = 0.061) and increased with age (P-value for trend, [Ptrend] < 0.0001). The mortality rates for nonviral cancers were stable over the follow-up period, whereas those for viral cancers showed a decrease from the years 2004–2006 to the years after 2007. We also observed a slight increase during 2018–2021, which was mainly due to an increase in liver cancer mortality rates which varied from 0.15 × 1,000 person-years (95%CI 0.06–0.40) in 2014–2017 to 0.34 × 1,000 person-years (95%CI 0.20–0.59) during 2018–2021 (see online resource Fig. 1).
NADC mortality was higher among PLWH than that of the general population, matched by age, sex and period (SMR: 1.79 (95%CI 1.54, 2.07)), especially for viral NADC and for most specific cancers (Table 2). SMRs were highest for Hodgkin lymphoma, anal and liver cancer. The risk of death due to oesophageal, kidney or lung cancer among PLWH was at least twice that of the general population. Whenever mortality was lower in PLWH than that of the general population, the estimates were imprecise.
SMRs for viral cancers were higher in females (17.35 (95%CI 7.79, 38.61)) than in males (4.11 (95%CI 2.77, 6.08), Pint = 0.007). For nonviral cancers, there was some evidence that the SMRs were also higher in females than males (2.23 (95%CI 1.45, 3.42) vs 1.45 (95%CI 1.19, 1.75), Pint = 0.086) (See online resource Table 1).
The SMRs decreased with age: NADC mortality in PLWH was three times higher than that of the general population in age groups under 50 years and gradually decreased to a similar rate than that of the general population in age groups over 70 years (Ptrend < 0.001). This decrease was particularly evident for viral cancers (Ptrend = 0.054). (Fig. 1). Like the mortality rates, SMRs for viral cancers were the highest during the years 2004–2006 and decreased thereafter while SMRs for nonviral and all NADC showed minor variation over time (Ptrend = 0.077 and 0.083, respectively) (Online resource Fig. 1).
Participants’ characteristics in association with NADC mortality
Table 3 shows the multivariable analysis of participants’ characteristics associated with mortality due to all, viral and nonviral NADC, and lung and liver cancers. Subjects who acquired HIV through heterosexual contact or use of injected drugs had a higher mortality risk due to NADC than men who acquired HIV through sex with men. The factor that was most strongly associated with mortality in all categories analysed (all NADC, and viral, nonviral and lung cancers), was the time-updated CD4 T-cell count. Compared to subjects with CD4 counts ≥ 500/µL, the mortality risk steeply increased with more profound immunodeficiency. Active smoking was strongly associated with mortality due to all, nonviral, and lung cancers, and hepatitis B or C infection were associated with NADC mortality in all categories. For all categories analysed, there was some evidence that subjects from non-European origin had a lower risk of mortality. After adjusting for other risk factors, mortality in all categories analysed was similar for sex, viral load, CD4/CD8 ratio, or AIDS diagnosis at enrolment. Lung cancer mortality risk increased with active or past smoking, heterosexual contact as transmission route, and CD4 counts < 500/µL; liver cancer mortality was associated with injected drugs or heterosexual contact as transmission route.
Discussion
In this large Spanish cohort of PLWH followed up between 2004 and 2021, we observed that NADC accounted for 21% of all deaths and that NADC mortality rate was 1.58 per 1,000 person-years. We observed that PLWH had a 79% higher risk of NADC mortality than the general population, especially among women and at younger ages. Sustained immunodeficiency, smoking and viral hepatitis were independently associated with an increased risk of NADC mortality. These findings underline that PLWH have an increased risk of death due to NADC than people from the general population of the same sex, age and period and that NADC mortality risk is related to a combination of traditional life-style factors, such as smoking and coinfection, and HIV-related risk factors, such as immunodeficiency. This is, to our knowledge, the first study assessing risk factors for NADC mortality that considers both traditional and HIV-related factors in recent years.
Although mortality in PLWH has been decreasing during the last decade in most European countries including Spain (Gueler et al. 2017; Fontela et al. 2020), we observed that NADC mortality rates remained constant over time. Similar results were observed in a multi-cohort study including PLWH from Europe, USA, and Australia during 1999–2011 (Smith et al. 2014) and more recently in the Navarra region in Spain (Fontela et al. 2020). Earlier European studies have shown a stable incidence of NADC among PLWH (Franceschi et al. 2010; García-Abellán et al. 2019; Poizot-Martin et al. 2021) and the fact that NADC mortality rates did not decrease in PLWH, while they did in the general population (Sociedad Española de Oncología Médica 2023), suggests that cancer-reducing interventions implemented so far might not be adequately reaching PLWH.
NADC mortality was 80% higher than that of the general Spanish population: this is similar to that reported in other studies (Croxford et al. 2017; Hessol et al. 2018). SMRs were the highest for cancers related to oncogenic viruses, but also for smoking-related cancers including lung, oesophagus and kidney, as previously observed (Yuan et al. 2022). Results from this same cohort during the years 2004–2014 have shown that the NADC excess mortality with respect to the general population was mainly due to increasing age, low CD4 count and HCV coinfection (Alejos et al. 2016). The same factors that are associated with cancer incidence may explain this increased mortality risk, such as smoking, alcohol use, chronic viral hepatitis, and other pro-oncogenic viruses such as HPV (Parka et al. 2016; Leierer et al. 2021). Also, PLWH have shown poorer outcomes compared with HIV-negative oncological patients (Suneja et al. 2013), which could be related to more advanced cancer stage at diagnosis (Shiels et al. 2015) or disparities in cancer treatment (Suneja et al. 2016) and screening (Corrigan et al. 2019). Most of these studies have been conducted in the United States, and whether the same drivers apply also in Europe is largely unknown.
We observed higher SMRs for women than for men, mainly for viral cancer mortality, in contrast with a study in the United Kingdom (Croxford et al. 2017) that reported slightly higher SMRs in males, but only during the first year of diagnosis.
Previous studies observed higher SMR for all-cause mortality in women than in men (Lewden et al. 2012). This result may reflect differences in the distribution of factors associated with NADM mortality (such as education, socioeconomic status and access to health care, prevalence of smoking, alcohol consumption, use of injected drugs or coinfections) between women living with HIV and those of the general population. In Spain, women living with HIV have been infected through use of injected drugs more frequently than men, and therefore have a higher prevalence of hepatitis C coinfection, as we have previously seen in our cohort (Muñoz Hornero et al. 2021). The excess mortality due to viral cancers in women is likely due to hepatocellular carcinoma and is probably due to the higher prevalence of chronic hepatitis B and C infection observed in women living with HIV with respect to those HIV-seronegative as observed in Collins et al. (Collins et al. 2021).
There is a lack of research investigating specific risk factors for NADC mortality in women with HIV.
The greatest difference in mortality risk between PLWH and the general population occurred before 50 years of age. Previous studies have shown younger ages at diagnosis in PLWH for certain cancers, such as lung and anal (Shiels et al. 2017), which could be related to the earlier and/or greater exposure to risk factors such as cigarette smoking and HPV (Parka et al. 2016). Also, PLWH with HCV or HBV coinfection experience faster progression to cirrhosis (Osborn et al. 2007; de Lédinghen et al. 2008) which is the main risk factor for hepatocellular carcinomas.
Results from the multivariable analysis showed that, compared to MSM, mortality risk was higher in subjects who acquired HIV through heterosexual contact and especially through IDU. This could be related to earlier diagnosis due to active HIV testing and a good adherence to HIV management that are more frequent in MSM (Rava et al. 2021; Izquierdo Miguel et al. 2023). The higher mortality due to NADC in IDU has been previously described (Trickey et al. 2016).
There was some evidence of lower NADC mortality among subjects of non-European origin. A previous meta-analysis showed lower mortality in migrants with respect to general population for all-cause mortality as well as for cancer mortality (Aldridge et al. 2018). These results can be explained with the healthy migrant hypothesis (people that decide to migrate are usually young and healthy) and the salmon bias (migrants frequently return to their country of origin when they are in poor health or before death) (Borhade and Dey 2018).
Two potentially modifiable factors were most strongly associated with mortality: low CD4 count and smoking. CD4 count was the most important prognostic factor for mortality due to all, viral, and nonviral NADC, including lung cancer. This has been observed in previous studies (d’Arminio et al. 2008; Leierer et al. 2021) and underlines the need for prompt HIV diagnosis and early treatment initiation, as well as good treatment adherence. Besides, these associations support the implementation of tailored cancer surveillance approach in PLWH with higher risk of NADC incidence and mortality. Regarding smoking, 44% of our patients were active smokers, which is a higher proportion than that of the Spanish general population, which ranged between 29.6% and 34.0% during the years 2005–2019 (Observatorio Español de las Drogas y las Adicciones 2021). Given that active smoking was associated with a two-fold risk of NADC mortality and more than ten-fold risk of lung cancer mortality, and that more than a third of the NADC deaths were due to lung cancer, this stresses the need to reinforce the interventions for smoking cessation among PLWH.
After adjusting for other risk factors, other markers of advanced HIV infection as HIV viral load, AIDS diagnosis at enrolment, and CD4/CD8 ratio were not associated with mortality. A study in the D:A:D cohort (Monforte et al. 2008a) also found that HIV viral load was not significantly associated with mortality after adjusting for CD4 count.
Hepatitis B and C coinfections were associated with an increased risk of death due to NADC, and specifically hepatitis C was associated with increased mortality due to viral cancers. However, although the risk estimates for liver cancer mortality were high for patients with hepatitis B or C, the estimates were uncertain probably due to the low number of cases. Our results are also limited by the lack of information on direct acting antivirals for the treatment of hepatitis C, which have been shown to decrease the incidence of liver cancer (Morgan et al. 2013).
Our study has several limitations. We were not able to ascertain the cause of death in 11.4% of the subjects. Also, we could not include in the viral cancer group several cancers of known viral origin such as vagina/vulva and oral cavity/pharynx, which are caused by HPV. Another limitation was the lack of information on HPV infection as well as the high proportion of missing data for important cancer-associated factors such as BMI, alcohol consumption, smoking status and HCV/HBV coinfections.
In conclusion, NADC mortality accounted for a large proportion of deaths among PLWH and was associated mainly to immunodeficiency, smoking, and coinfection with hepatitis B and C, which are all preventable risk factors. Besides, NADC mortality was higher in PLWH than in the general population, especially for viral cancers and among women and at younger ages. These findings highlight the importance of prompt HIV diagnosis and linkage to care, along with tailored strategies to enhance early detection of cancer as well as the need of prevention and modification of traditional cancer risk factors among PLWH, with a special attention to women and younger people.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HPV:
-
Human papillomavirus
- IDU:
-
Injecting drug use
- MRR:
-
Mortality rate ratio
- MSM:
-
Men having sex with men
- NADC:
-
Non-AIDS-defining cancers
- PLWH:
-
People living with HIV
- SMR:
-
Standardized mortality ratio
References
Aldaz P, Moreno-Iribas C, Egüés N et al (2011) Mortality by causes in HIV-infected adults: comparison with the general population. BMC Public Health 11:300. https://doi.org/10.1186/1471-2458-11-300
Aldridge RW, Nellums LB, Bartlett S et al (2018) Global patterns of mortality in international migrants: a systematic review and meta-analysis. Lancet 392:2553–2566. https://doi.org/10.1016/S0140-6736(18)32781-8
Alejos B, Hernando V, Iribarren J et al (2016) Overall and cause-specific excess mortality in HIV-positive persons compared with the general population: role of HCV coinfection. Medicine (Baltimore) 95:e4727. https://doi.org/10.1097/MD.0000000000004727
Bonnet F, Lewden C, May T et al (2004) Malignancy-related causes of death in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. Cancer 101:317–324. https://doi.org/10.1002/cncr.20354
Borhade A, Dey S (2018) Do migrants have a mortality advantage? Lancet 392:2517–2518. https://doi.org/10.1016/S0140-6736(18)33052-6
Clifford GM, Polesel J, Rickenbach M et al (2005) Cancer risk in the Swiss HIV cohort study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst 97:425–432. https://doi.org/10.1093/jnci/dji072
Collins LF, Sheth AN, Mehta CC et al (2021) The prevalence and burden of non-AIDS comorbidities among women living with or at risk for human immunodeficiency virus infection in the United States. Clin Infect Dis 72:1301–1311. https://doi.org/10.1093/cid/ciaa204
Corrigan KL, Wall KC, Bartlett JA, Suneja G (2019) Cancer disparities in people with HIV: a systematic review of screening for non-AIDS–defining malignancies. Cancer 125:843–853. https://doi.org/10.1002/cncr.31838
Croxford S, Kitching A, Desai S et al (2017) Mortality and causes of death in people diagnosed with HIV in the era of highly active antiretroviral therapy compared with the general population: an analysis of a national observational cohort. Lancet Public Heal 2:e35–e46. https://doi.org/10.1016/S2468-2667(16)30020-2
d’Arminio MA, Abrams D, Pradier C et al (2008) HIV-induced immunodeficiency and mortality from AIDS-defining and non-AIDS-defining malignancies. AIDS 22:2143–2153. https://doi.org/10.1097/QAD.0b013e3283112b77
de Lédinghen V, Barreiro P, Foucher J et al (2008) Liver fibrosis on account of chronic hepatitis C is more severe in HIV-positive than HIV-negative patients despite antiretroviral therapy. J Viral Hepat 15:427–433. https://doi.org/10.1111/j.1365-2893.2007.00962.x
Engels EA, Yanik EL, Wheeler W et al (2017) Cancer-attributable mortality among people with treated human immunodeficiency virus infection in North America. Clin Infect Dis 65:636–643. https://doi.org/10.1093/cid/cix392
Observatorio Español de las Drogas y las Adicciones (2021) Alcohol, tabaco y drogas ilegales en España. Madrid
Fontela C, Aguinaga A, Moreno-Iribas C et al (2020) Trends and causes of mortality in a population-based cohort of HIV-infected adults in Spain: comparison with the general population. Sci Rep 10:8922. https://doi.org/10.1038/s41598-020-65841-0
Franceschi S, Lise M, Clifford GM et al (2010) Changing patterns of cancer incidence in the early-and late-HAART periods: The Swiss HIV Cohort Study. Br J Cancer 103:416–422. https://doi.org/10.1038/sj.bjc.6605756
García-Abellán J, del Río L, García JA et al (2019) Risk of cancer in HIV-infected patients in Spain, 2004–2015. The CoRIS cohort study. Enferm Infecc Microbiol Clin. https://doi.org/10.1016/j.eimc.2018.11.011
Gueler A, Moser A, Calmy A et al (2017) Life expectancy in HIV-positive persons in Switzerland. AIDS 31:427–436. https://doi.org/10.1097/QAD.0000000000001335
Hernández-Ramírez RU, Shiels MS, Dubrow R, Engels EA (2017) Cancer risk in HIV-infected people in the USA from 1996 to 2012: a population-based, registry-linkage study. Lancet HIV 4:e495–e504. https://doi.org/10.1016/S2352-3018(17)30125-X
Hernando V, Sobrino-Vegas P, Burriel MC et al (2012) Differences in the causes of death of HIV-positive patients in a cohort study by data sources and coding algorithms. AIDS 26:1829–1834. https://doi.org/10.1097/QAD.0b013e328352ada4
Hessol NA, Ma D, Scheer S et al (2018) Changing temporal trends in non-AIDS cancer mortality among people diagnosed with AIDS: San Francisco, California, 1996–2013. Cancer Epidemiol 52:20–27. https://doi.org/10.1016/j.canep.2017.11.004
Hu J, Liu K, Luo J (2019) HIV–HBV and HIV–HCV Coinfection and Liver Cancer Development. pp 231–250
Izquierdo Miguel R, Rava M, Moreno-García E, et al (2023) HIV medical care interruption among people living with HIV in Spain, 2004–2020. AIDS Publish Ah:2004–2020. https://doi.org/10.1097/QAD.0000000000003552
Leierer G, Rieger A, Schmied B et al (2021) A lower CD4 count predicts most causes of death except cardiovascular deaths. The Austrian HIV Cohort Study. Int J Environ Res Public Health 18:12532. https://doi.org/10.3390/ijerph182312532
Lewden C, Bouteloup V, De Wit S et al (2012) All-cause mortality in treated HIV-infected adults with CD4 >=500/mm3 compared with the general population: evidence from a large European observational cohort collaboration. Int J Epidemiol 41:433–445. https://doi.org/10.1093/ije/dyr164
López C, Masiá M, Padilla S et al (2016) Muertes por enfermedades no asociadas directamente con el sida en pacientes con infección por el VIH: Un estudio de 14 años (1998–2011). Enferm Infecc Microbiol Clin 34:222–227. https://doi.org/10.1016/j.eimc.2015.04.010
Morgan RL, Baack B, Smith BD et al (2013) Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma. Ann Intern Med 158:329. https://doi.org/10.7326/0003-4819-158-5-201303050-00005
Muñoz Hornero C, Muriel A, Montero M et al (2021) Diferencias epidemiológicas y de mortalidad entre hombres y mujeres con infección por VIH en la cohorte CoRIS entre los años 2004 y 2014. Enferm Infecc Microbiol Clin 39:372–382. https://doi.org/10.1016/j.eimc.2020.05.021
Osborn M, Guest J, Rimland D (2007) Hepatitis B virus and HIV coinfection: relationship of different serological patterns to survival and liver disease. HIV Med 8:271–279. https://doi.org/10.1111/j.1468-1293.2007.00469.x
Parka LS, Hernandez-Ramirez RU, Silverberg MJ et al (2016) Prevalence of non-HIV cancer risk factors in persons living with HIV/AIDS: A meta-analysis. AIDS 30:273–291. https://doi.org/10.1097/QAD.0000000000000922
Picard A, Badoual C, Hourseau M et al (2016) Human papilloma virus prevalence in HIV patients with head and neck squamous cell carcinoma. AIDS 30:1257–1266. https://doi.org/10.1097/QAD.0000000000001030
Poizot-Martin I, Lions C, Allavena C et al (2021) Spectrum and incidence trends of AIDS- and Non–AIDS-defining cancers between 2010 and 2015 in the French Dat’AIDS Cohort. Cancer Epidemiol Biomarkers Prev 30:554–563. https://doi.org/10.1158/1055-9965.EPI-20-1045
R Core Team (2020) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
Rava M, Domínguez-Domínguez L, Bisbal O et al (2021) Late presentation for HIV remains a major health issue in Spain: Results from a multicenter cohort study, 2004–2018. PLoS ONE 16:e0249864. https://doi.org/10.1371/journal.pone.0249864
Shiels MS, Engels EA (2017) Evolving epidemiology of HIV-associated malignancies. Curr Opin HIV AIDS 12:6–11. https://doi.org/10.1097/COH.0000000000000327
Shiels MS, Copeland G, Goodman MT et al (2015) Cancer stage at diagnosis in patients infected with the human immunodeficiency virus and transplant recipients. Cancer 121:2063–2071. https://doi.org/10.1002/cncr.29324
Shiels MS, Althoff KN, Pfeiffer RM et al (2017) HIV infection, immunosuppression, and age at diagnosis of non-AIDS-defining cancers. Clin Infect Dis 64:468–475. https://doi.org/10.1093/cid/ciw764
Smith CJ, Ryom L, Weber R et al (2014) Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet 384:241–248. https://doi.org/10.1016/S0140-6736(14)60604-8
Sobrino-Vegas P, Gutiérrez F, Berenguer J et al (2011) La cohorte de la red española de investigación en sida y su biobanco: organización, principales resultados y pérdidas al seguimiento. Enferm Infecc Microbiol Clin 29:645–653. https://doi.org/10.1016/j.eimc.2011.06.002
Sociedad Española de Oncología Médica (2023) Las cifras del cáncer en España 2023. Soc Española Oncol Médica
Suneja G, Shiels MS, Melville SK et al (2013) Disparities in the treatment and outcomes of lung cancer among HIV-infected individuals. AIDS 27:459–468. https://doi.org/10.1097/QAD.0b013e32835ad56e
Suneja G, Lin CC, Simard EP et al (2016) Disparities in cancer treatment among patients infected with the human immunodeficiency virus. Cancer 122:2399–2407. https://doi.org/10.1002/cncr.30052
Tenorio AR, Zheng Y, Bosch RJ et al (2014) Soluble markers of inflammation and coagulation but not T-cell activation predict non-AIDS-defining morbid events during suppressive antiretroviral treatment. J Infect Dis 210:1248–1259. https://doi.org/10.1093/infdis/jiu254
Trickey A, May MT, Vehreschild J et al (2016) Cause-specific mortality in HIV-positive patients who survived ten years after starting antiretroviral therapy. PLoS One 11:e0160460. https://doi.org/10.1371/journal.pone.0160460
Weber R, Ruppik M, Rickenbach M et al (2013) Decreasing mortality and changing patterns of causes of death in the Swiss HIV Cohort Study. HIV Med 14:195–207. https://doi.org/10.1111/j.1468-1293.2012.01051.x
Yuan T, Hu Y, Zhou X, et al (2022) Incidence and mortality of non-AIDS-defining cancers among people living with HIV: a systematic review and meta-analysis. eClinicalMedicine 52:101613. https://doi.org/10.1016/j.eclinm.2022.101613
Zwahlen M, Harris R, May M et al (2009) Mortality of HIV-infected patients starting potent antiretroviral therapy: comparison with the general population in nine industrialized countries. Int J Epidemiol 38:1624–1633. https://doi.org/10.1093/ije/dyp306
Acknowledgements
The list of CoRIS members is provided as Supplementary Information. This study would not have been possible without the collaboration of all patients, medical and nursing staff and data mangers who have taken part in the project.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research was supported by CIBER -Consorcio Centro de Investigación Biomédica en Red- (CB21/13/00091), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación and Unión Europea – NextGenerationEU, the Gilead Scholarship Program for Biomedical Research (GLD19_00106) and the ISCIII- Miguel Servet CP19CIII—00002 contract.
Author information
Authors and Affiliations
Consortia
Contributions
MR conceived, designed the study and conducted all statistical analyses. IS, and MR drafted the manuscript; IS, FG, JMP, IJ played an important role in interpreting the results. All authors revised and approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved and critical revisions of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interests
MR received funds from Gilead Science; IS-G and AC have received conference grants or speaker fees from ViiV Healthcare, Merck Sharp & Dohme, Janssen and Gilead. EVO has received conference grants or counselling fees from Janssen, MSD, Gilead y ViiV. All other authors declare no conflict of interest.
Ethics approval
The CoRIS cohort was approved by the Clinical Research Ethics Committee of the Gregorio Marañón General University Hospital. This study was approved by the Carlos III Institute Research Ethics Committee (PI 05_2019) and was performed in accordance with the Declaration of Helsinki.
Consent to participate
All patients agree to participate in CoRIS by signing an informed consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The list of CoRIS members is provided as Supplementary Information.
Novelty and Impact: Mortality due to non-AIDS defining cancers (NADC) has become one of the leading causes of death in people living with HIV (PLWH). We provided updated estimates of NADC mortality and explored potential risk factors. PLWH had an increased risk of death due to NADC than people from the general population. NADC mortality risk was related to a combination of traditional life-style factors, such as smoking and coinfection, and HIV-related risk factors, such as immunodeficiency.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Suárez-García, I., Gutierrez, F., Pérez-Molina, J.A. et al. Mortality due to non-AIDS-defining cancers among people living with HIV in Spain over 18 years of follow-up. J Cancer Res Clin Oncol 149, 18161–18171 (2023). https://doi.org/10.1007/s00432-023-05500-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05500-9