Abstract
Background
Malaria remains a very important public health problem in Ethiopia. Currently, only Plasmodium falciparum and Plasmodium vivax are considered in the malaria diagnostic and treatment policies. However, the existence and prevalence of Plasmodium ovale spp. and Plasmodium malariae in Ethiopia have not been extensively investigated. The objective of this study was to use a multiplex IgG antibody detection assay to evaluate evidence for exposure to any of these four human malaria parasites among asymptomatic individuals.
Methods
Dried blood spots (DBS) were collected from 180 healthy study participants during a 2016 onchocerciasis survey in the Jimma Zone, southwest Ethiopia. IgG antibody reactivity was detected using a multiplex bead assay for seven Plasmodium antigens: P. falciparum circumsporozoite protein (CSP), P. falciparum apical membrane antigen-1 (AMA1), P. falciparum liver stage antigen-1 (LSA1), and homologs of the merozoite surface protein-1 (MSP1)-19kD antigens that are specific for P. falciparum, P. vivax, P. ovale spp. and P. malariae.
Results
One hundred six participants (59%) were IgG seropositive for at least one of the Plasmodium antigens tested. The most frequent responses were against P. falciparum AMA1 (59, 33%) and P. vivax (55, 28%). However, IgG antibodies against P. ovale spp. and P. malariae were detected in 19 (11%) and 13 (7%) of the participants, respectively, providing serological evidence that P. malariae and P. ovale spp., which are rarely reported, may also be endemic in Jimma.
Conclusion
The findings highlight the informative value of multiplex serology and the need to confirm whether P. malariae and P. ovale spp. are aetiologies of malaria in Ethiopia, which is critical for proper diagnosis and treatment.
Similar content being viewed by others
Background
In 2017, an estimated 219 million cases of malaria occurred worldwide, compared with 239 million cases in 2010 and 217 million cases in 2016 [1]. An estimated 435,000 deaths from malaria recorded globally in 2017, compared with 451,000 estimated deaths in 2016, and 607,000 in 2010 [1]. An increasing number of countries are moving towards eliminating malaria. Ethiopia is among the sub-Saharan African countries that have successfully reduced their malaria burden in the last decade [2, 3]. The Government of Ethiopia launched an elimination strategy taking advantage of this progress, in line with the commitment of African leaders to attain malaria elimination by 2030 [4]. The Federal Ministry of Health (FMoH) achieved significant declines in malaria mortality and incidence and has recently declared its objective to eliminate malaria by 2020 in low transmission areas that have an annual parasite incidence (API) of less than one per 1000 total populations. The goal is to achieve nationwide elimination by 2030 [4]. The Plasmodium species causing malaria in Ethiopia are Plasmodium falciparum, accounting for about 60% of cases, and Plasmodium vivax, which accounts for about 40% of cases, with the former being the cause of most severe clinical manifestations and deaths [4, 6]. Current case management protocols target both species [4, 5], but may not be adequate for other Plasmodium species.
Plasmodium ovale spp. [7, 8] and Plasmodium malariae [6] have also been reported from limited areas in Ethiopia. Additionally, the FMoH has historical records that include reports of sizeable number of cases of both P. malariae and P. ovale spp. during the 1980s and 1990s [6,7,8]. However, current information about population-level exposure estimates to these species is limited.
The multiplex bead assay (MBA) can provide accurate and quantitative information about the diversity of exposure to malaria parasites by measuring human antibody levels against several antigens concurrently. In this study, MBA incorporating seven Plasmodium antigen targets used to assess malaria seroprevalence in the Limu Kossa District, Jimma Zone in southwest Ethiopia. Four antigen targets were specific for P. falciparum infection, including indicators of long and short-term infection. Homologs of the P. falciparum merozoite surface protein 1 (MSP-1) for P. vivax, P. ovale spp. and P. malariae were used to characterize species-specific responses [9,10,11,12,13].
Methods
Study area and design
A total of 180 dried blood spot (DBS) samples were collected in October 2016 as part of a community-based onchocerciasis survey in the villages of Arengama 1, Arengama 2 and Konche in Limu Kossa District, Jimma zone, Oromia Region, which is located 400 km in the south west of Addis Ababa. Study participants were selected through convenience sampling among village residents with age 5 years and above who provided consent and assent and participated in an interview and finger prick blood collection.
Laboratory analysis by multiplex bead assay (MBA)
Seven malaria antigens were coupled to polystyrene beads using 1-ethyl-3-(3-dimethylaminopropyl) (Calbiochem, Woburn, MA) carbodiimide to convert carboxyl groups on the surface of the magnetic microspheres (MagPlex Beads; Luminex Corporation, Austin, TX) to reactive esters. The esters readily react with available primary amino groups on the antigens to form covalent amide bonds between antigen and microspheres. The seven recombinant antigens were expressed as Glutathione S-transferases (GST) fusion proteins and were coupled to activated beads in separate reaction tubes (12.5 million beads each) using 30 µg P. falciparum CSP, 60 µg P. falciparum LSA1, 20 µg P. falciparum AMA-1, and 20 µg of each of the four species-specific MSP-1-19kD antigen in 50 mM 2-(N-morpholino) ethanesulfonic acid (MES), 0.85% NaCl, pH 5.0. As a control, for non-specific binding of human IgG, 15 µg GST was coupled to beads a using the same conditions.
The MBA was conducted using serum eluted from DBS to a final dilution of 1:400 in buffer B (PBS with 0.5% BSA, 0.3% Tween 20, 0.1% sodium azide, 0.5% polyvinyl alcohol, 0.8% polyvinylpyrrolidone, 0.1% casein, and 4 µg/ml crude Escherichia coli extract), incubated for 1 h at 37 °C, and then stored at 4 °C overnight. The next day, the assay plate (Sigma Millipore, MAHVN4550, Burlington, MA) was pre-wetted with 200 µl phosphate buffered saline pH 7.2 plus 0.05% Tween20 (PBS-T) and evacuated with vacuum. To prepare a bead mix, beads coupled with each of the 7 different malaria antigens were re-suspended by vortexing, and 15 µl of each (~ 250,000 beads) of the antigen-coupled beads were transferred to conical tubes containing 5 ml Buffer A (PBS-T, 0.5% bovine serum albumin, 0.02% NaN3). Of this bead mix, 50 µl were transferred to each well (~ 2500 each bead classification per well) of the assay plate using multichannel pipette and washed twice with 100 µl of PBS-T. To detect IgG reactivity, 50 µl of the prepared samples were added in duplicate wells, incubated for 90 min at room temperature on a shaker and then washed three times. After washing, 50 µl of biotinylated mouse anti-human IgG (Southern Biotech, 9042-08, Birmingham, USA) diluted at 50 ng/well in buffer A was added to each well and incubated for 45 min at room temperature on a shaker. After three washes to remove the excess biotinylated antibodies, 50 µl 1:200 streptavidin-phycoerythrin (Invitrogen S866, Waltham, USA) solution in buffer A was added per well and incubated at room temperature for 1 h on a shaker. The plate was washed once, 50 µl of buffer A were added to each well and incubated for 30 min at room temperature on a shaker. In the last step, the plate was washed and 125 µl of PBS added to each well, incubated for 2 min with shaking, and followed by immediate reading on the Bio-Rad Bio-Plex 200 System, (Bio-Rad, Hercules, CA, USA). Data were acquired with Bio-Plex manager 6.1 Software (Bio-Rad) with a protocol to read plates at High RPI and 100 beads/well per region. The means of the median fluorescence intensity (MFI) minus background from blank wells (MFI-bg) were calculated as the final MFI-bg reading for duplicate wells for each sample. Positivity to the seven antigens for the four Plasmodium species was evaluated using previously determined cut-off values (Table 1). The cut-off was calculated using a panel of 92 samples from United States residents without history of travel outside the US. From the results, the log normal mean was calculated and added three standards deviations to get the MFI-Bg cut off.
Statistical analysis
Data were imported into an Excel database and analysed using SPSS V 20. Descriptive statistics were used to describe the demographic characteristics and prevalence of antibodies to each antigen individually and in combination.
Results
Sero-diagnosis of Plasmodium species
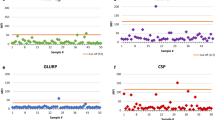
Of the 180 enrolled study participants, 121 (67.2%) were male and 59 (32.8%) females with a mean age of 49 years (standard deviation = 14). Of all samples analysed, 106 (59%) were seropositive for IgG antibodies against at least one of the malaria antigens tested. Antibodies reactive with P. falciparum were detected most frequently, with 59 (33%) seropositive persons to P. falciparum AMA1, 52 (29%), to P. falciparum MSP 1-19kD, 16 (9%) to, P. falciparum CSP and 4 (2%) to P. falciparum LSA1 (Table 2 and Fig. 1). The IgG positivity for P. falciparum MSP 1-19kD and/or P. falciparum AMA1 antigens was 39% (n = 71) and 11% (20) had evidence of exposure to either P. falciparum CSP and/or P. falciparum LSA1 antigens.
Malaria exposure history
Fifteen percent (27 of 180) of the study participants had evidence for a lifetime exposure history to both P. falciparum and P. vivax. Additionally 6.7% had evidence for P. falciparum and P. malariae exposure. The serologic evidence of exposure to different Plasmodium species is indicated in Table 3.
Discussion
Malaria elimination is the interruption of local transmission. This is achieved by detecting every infection and managing each case properly [4]. Identifying the Plasmodium species type and intensive implementation of malaria diagnosis and treatment accordingly is important for the elimination programmes. Malaria in Ethiopia has traditionally considered to be caused primarily by P. falciparum and P. vivax hence these species are targeted in the national malaria diagnosis and treatment strategy; there has been limited information on the importance of P. ovale spp. and P. malariae in Ethiopia. Here, a novel MBA, a bead-based technology that allows multi-analyte profiling, where microsphere beads with unique light spectra are coupled to specific antigens [12], to determine the diversity of exposure to malaria parasites.
Human infections with Plasmodium species elicit antibody responses to multiple parasite stages and the presence of these antibodies can be used as indicators of parasite exposure [15]. MBA using seven informative malaria antigens provided information on the Plasmodium species exposure types in Jimma area. The information will inform national malaria diagnosis and treatment strategies, for example, by including guidance for supporting diagnosis of all malaria species found in Ethiopia.
Antibodies to Plasmodium antigens such as AMA1 [14], CSP [15], MSP1 [16], and LSA-1 have all been used as biomarkers of malaria transmission in various endemic settings [11], and were included in this multiplex serology assay. The observed low seroprevalence to the non-erythrocytic antigens, CSP and LSA-1 could suggest that the study area has low transmission rates of P. falciparum, as antibody responses to these antigens decay faster than responses to blood-stage antigens. The MSP-1 antigen, a predominant merozoite surface antigen that is present in all examined Plasmodium species, and the species-specific 19kD fragments (MSP 1-19kD) were useful in this study to determine that all four species were being transmitted. P. falciparum and P. vivax MSP-1 are used extensively as serological biomarkers, and often used for population studies [17, 18] and according to a previous study, there is no evidence of cross reactivity between the species-specific MSP-1 antigens [19].
Currently, P. falciparum and P. vivax are considered the main aetiologies of malaria in Ethiopia and the national diagnostic and treatment strategies only cover these two species. However, in this survey antibody evidence in 10.6% and 7.2% of the study participants had IgG responses that were specific for P. malariae and P. ovale spp., respectively. The samples tested came from a convenience sample of the population, and thus may not be representative of the local or national population. Furthermore, because these are antibody responses, these rates may not be accurate estimates of current incidence or prevalence even in the tested population, the results clearly indicates that at some time point, P. malariae and P. ovale spp. have been present in Ethiopia. Additional studies are needed to demonstrate the distribution and prevalence for P. malariae and P. ovale spp. Even though the findings are novel for Ethiopia, both P. ovale spp. and P. malariae were similarly reported in some countries in Africa [16, 20, 21].
The study also showed the value of MBA serology, as it allows analysing multiple antibodies at one time and indicated antibody exposure to more than one human malaria species in 27% of the study participants. The seroprevalence of P. falciparum and P. vivax MSP 1-19kD antigens was almost equal, with 29 and 28% of the population in Limu Kossa having IgG antibodies to these two antigens, respectively. Fifteen percent of the population had IgG to both of these antigens, confirming that exposure to both species has occurred in Ethiopia.
While P. falciparum and P. vivax infections remain as a primary concern in Ethiopia, the detection of antibodies specific against P. malariae and P. ovale spp. is important [18] because both can cause chronic nephritic syndrome, leading to adverse reactions during treatment and high mortality rates [13]. It is challenging to diagnose P. malariae and P. ovale by microscopy due to low parasitaemia and resemblance to P. vivax particularly in cases of mixed infection. Furthermore, RDTs have limited ability to detect these species [22], which also leads to misdiagnosis. Inability to accurately diagnose and promptly treat P. malariae and P. ovale cases can affect patient medical outcomes in particular and the elimination programme in general. The choice of treatment for confirmed P. ovale spp. and P. malariae infection is chloroquine at 25 mg/kg for 3 days [23]. P. ovale spp. and P. malariae are also susceptible to artemisinin-based combination therapy (ACT). Mixed infection of P. falciparum with P. ovale spp. or P. malariae can successfully be treated with ACT drugs [23]. However, the efficacy of these drugs to P. ovale spp. and to P. malariae is not studied in Ethiopia.
Multiple serological data sets generated using MBA, which might not have otherwise been collected as part of surveillance, is helpful for program decision-making. It is important for the national treatment guidelines to explicitly include P. malariae and P. ovale spp. in the treatment algorithm; for example, microscopy might be recommended in cases where RDTs are negative but symptoms persist. Future studies with larger populations that include microscopy or DNA based methods are needed to unequivocally demonstrate the presence of active P. malariae and P. ovale infections. These findings are important for the Ethiopian programme in their quest to eliminate human malaria.
Limitation of the study
The study participants are residents of Konche, Arengama 1 and Arengama 2 villages of Limu Kossa Districts selected based on convenient sampling. Therefore, the result may not be generalizable to the entire district population.
Conclusion
The study showed well-defined evidence of malaria infections among the study participants, with P. falciparum and P. vivax having the highest exposure rates. It also revealed that P. malariae and P. ovale spp. were endemic at low levels in the Limu Kossa district of Ethiopia. Therefore, there is a need for robust studies to identify the distribution of Plasmodium species present in Ethiopia. Those findings may impact the national strategies for elimination, including clinical diagnosis and treatment, as well as the priorities for programmatic research.
Availability of data and materials
The database analysed in this study are available from the corresponding author.
References
WHO. World malaria report. Geneva: World Health Organization; 2018.
WHO. Regional profiles—world malaria report. Geneva: World Health Organization; 2015. p. 122.
WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization; 2015. p. 1–35.
Ethiopian Federal Ministry of Health. National malaria elimination roadmap. Addis Ababa: Ethiopian Federal Ministry of Health; 2016.
Vajda ÉA, Webb CE. Assessing the risk factors associated with malaria in the Highlands of Ethiopia: what do we need to know? Trop Med Infect Dis. 2017;2:E4.
Taffese HS, Jima D, Worku B, Ejigu HK. An epidemiological profile of malaria in Ethiopia. National Malaria Control Tean: Ethiopian Public Health Institute, WHO, INFORM Project, Addis Ababa; 2014.
Alelign A, Tadesse D. Current status of malaria in Ethiopia: evaluation of the burden, factors for transmission and prevention methods. Acta Parasitol Glob. 2016;7:1–6.
Alemu A, Fuehrer HP, Getnet G, Tessema B, Noedl H. Plasmodium ovale curtisi and Plasmodium ovale wallikeri in North-West Ethiopia. Malar J. 2013;12:346.
Díaz PB, Lozano PM, Rincón JM, García L, Reyes F, Llanes AB. Quality of malaria diagnosis and molecular confirmation of Plasmodium ovale curtisi in a rural area of the southeastern region of Ethiopia. Malar J. 2015;14:357.
Koffi D, Varela ML, Loucoubar C, Beourou S, Vigan-Womas I, Touré A, et al. Longitudinal analysis of antibody responses in symptomatic malaria cases do not mirror parasite transmission in peri-urban area of Côte d’Ivoire between 2010 and 2013. PLoS One. 2017;12:e0172899.
Kusi KA, Bosomprah S, Kyei-Baafour E, Dickson EK, Tornyigah B, Angov E, et al. Seroprevalence of antibodies against Plasmodium falciparum sporozoite antigens as predictive disease transmission markers in an area of Ghana with seasonal malaria transmission. PLoS One. 2016;11:e0167175.
Luminex. Six challenges in malaria research and ways to overcome them. Austin: Luminex; 2012.
Perraut R, Richard V, Varela ML, Trape JF, Guillotte M, Tall A, et al. Comparative analysis of IgG responses to Plasmodium falciparum MSP1p19 and PF13-DBL1α1 using ELISA and a magnetic bead-based duplex assay (MAGPIX®-Luminex) in a Senegalese meso-endemic community. Malar J. 2014;13:410.
Requena P, Arévalo-Herrera M, Menegon M, Martínez-Espinosa FE, Padilla N, Bôtto-Menezes C, et al. Naturally acquired binding-inhibitory antibodies to Plasmodium vivax Duffy Binding Protein in pregnant women are associated with higher birth weight in a multicenter study. Front Immunol. 2017;8:163.
Elliott SR, Fowkes FJ, Richards JS, Reiling L, Drew DR, Beeson JG. Research priorities for the development and implementation of serological tools for malaria surveillance. F1000Prime Rep. 2014;6:100.
Amanfo SA, Mduluza T, Midzi N, Cavanagh DR, Mutapi F. Seroepidemiology of Plasmodium species infections in Zimbabwean population. Malar J. 2016;15:267.
Sonaimuthu P, Cheong FW, Chin LC, Mahmud R, Fong MY, Lau YL. Detection of human malaria using recombinant Plasmodium knowlesi merozoite surface protein-1 (MSP-119) expressed in Escherichia coli. Exp Parasitol. 2015;153:118–22.
Li P, Zhao Z, Xing H, Li W, Zhu X, Cao Y, et al. Plasmodium malariae and Plasmodium ovale infections in the China–Myanmar border area. Malar J. 2016;15:557.
Priest JW, Plucinski MM, Huber CS, Rogier E, Mao B, Gregory CJ, et al. Specificity of the IgG antibody response to Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, and Plasmodium ovale MSP119 subunit proteins in multiplexed serologic assays. Malar J. 2018;17:417.
Poirier P, Doderer-Lang C, Atchade PS, de Lemoine JP, l’Isle MC, Abou-Bacar A, et al. The hide and seek of Plasmodium vivax in West Africa: report from a large-scale study in Beninese asymptomatic subjects. Malar J. 2016;15:570.
Mueller I, Zimmerman PA, Reeder JC. Plasmodium malariae and Plasmodium ovale—the ‘bashful’ malaria parasites. Trends Parasitol. 2007;23:278–83.
Betson M, Sousa-Figueiredo JC, Atuhaire A, Arinaitwe M, Adriko M, Mwesigwa G, et al. Detection of persistent Plasmodium spp. infections in Ugandan children after artemether–lumefantrine treatment. Parasitology. 2014;141:1880–90.
WHO. Guidelines for the treatment of malaria. 3rd ed. Geneva: World Health Organization; 2015.
Acknowledgements
We duly acknowledge the CDC Atlanta laboratory team for laboratory work support and the study participants for volunteering to be part of the study. We acknowledge Dr. Eric Rogier for his technical assistance with the multiplex assay and support in manuscript preparation.
Funding
This study was funded in part by a Grant from the Bill and Melinda Gates Foundation (Grant Number OPP1017858) and by the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
SF, VC, and GO designed the study, performed the experiments and drafted the manuscript. BB collected the samples and drafted the manuscript. AA, AW, HM drafted and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the scientific and ethical review board of Ethiopian Public Health Institute (EPHI) and CDC (protocol number: 6653). All study participants had previously provided signed consent to be part of the study and for long term storage and future use of the samples for other diseases of public health importance (excluding HIV).
Consent for publication
All authors have given their consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Feleke, S.M., Brhane, B.G., Mamo, H. et al. Sero-identification of the aetiologies of human malaria exposure (Plasmodium spp.) in the Limu Kossa District of Jimma Zone, South western Ethiopia. Malar J 18, 292 (2019). https://doi.org/10.1186/s12936-019-2927-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-019-2927-3