Abstract
Background
Plasmodium vivax is considered to be absent from western Africa, where the prevalence of Duffy-negative red blood cell phenotype proves to be high. Several studies have, however, detected P. vivax infection cases in this part of Africa, raising the question of what is the actual prevalence of P. vivax in local populations.
Methods
The presence of P. vivax was investigated in a large population of healthy blood donors in Benin using microscopy, serology and molecular detection. The seroprevalence was measured with species-specific ELISA using two recombinant P. vivax proteins, namely rPvMSP1 and rPvCSP1. Specific molecular diagnosis of P. vivax infection was carried out using nested-PCR. The performances and cut-off values of both rPvCSP1 and rPvMSP1 ELISA were first assessed using sera from P. vivax-infected patients and from non-exposed subjects.
Results
Among 1234 Beninese blood donors, no parasites were detected when using microscopy, whereas 28.7% (354/1234) of patients exhibited had antibodies against rPvMSP1, 21.6% (266/1234) against rPvCSP1, and 15.2% (187/1234) against both. Eighty-four samples were selected for nested-PCR analyses, of which 13 were positive for P. vivax nested-PCR and all Duffy negative.
Conclusion
The results of the present study highlight an unexpectedly high exposure of Beninese subjects to P. vivax, resulting in sub-microscopic infections. This suggests a probably underestimated and insidious parasite presence in western Africa. While the vaccination campaigns and therapeutic efforts are all focused on Plasmodium falciparum, it is also essential to consider the epidemiological impact of P. vivax.
Similar content being viewed by others
Background
About half of the world population is exposed to malaria parasites, and in 2015, the World Health Organization estimated that there were 214 millions of new cases of malaria worldwide, resulting in 438,000 deaths, essentially involving young African children [1]. While six parasitic species can cause human malaria, namely Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale curtisi, Plasmodium ovale wallikeri, Plasmodium malariae and Plasmodium knowlesi, it must be stressed that P. falciparum and P. vivax are the most prevalent malaria parasite species. Whereas both species display a widespread distribution, P. vivax has a wider distribution than P. falciparum, having recently re-emerged in the south of Europe [2]. In a recent review, Moreira et al., have highlighted the substantial morbidity and mortality associated with P. vivax infection, along with its low parasitaemia in endemic countries, and in particular Southeast Asia, western Pacific, and South America [3]. While the overall P. vivax prevalence in Africa remains low, the parasite is considered to be present in the Horn of Africa, yet almost absent in West Africa. To date, this has been mainly accounted for by the absence of the red blood cell surface Duffy antigen among Africans living in this area [4]. Meanwhile, however, P. vivax infections were documented in Duffy-negative subjects in Brazil [5, 6], Ethiopia [7, 8], Madagascar [9], but also in West African countries, such as Mauritania [10], Cameroon [11, 12], Equatorial Guinea, and Angola [13]. According to these different studies, the prevalence of P. vivax in West-Africa is probably underestimated and large-scale epidemiological studies are thus required to investigate the burden of P. vivax infections [3].
Microscopy diagnostic methods have been shown to be time-consuming, requiring experienced personnel, while possibly leading to misidentification between P. vivax and P. ovale spp., which are highly prevalent in West Africa [14]. For epidemiological studies to assess P. vivax infections, molecular biology has been commonly used and shown to be more sensitive than microscopy [3, 15].
Molecular biology, however, remains expensive for many countries in endemic areas [16]. Serologic assays constitute a good alternative for epidemiological survey and blood donor screening, given that, antibodies reflect exposure to pathogens [17]. ELISA assays were recently developed for the detection of anti-P. falciparum, P. ovale wallikeri/curtisi, and P. malariae antibodies by using species-specific recombinant MSP1 proteins [18]. By this mean, authors of that previous study have been able to highlight an unexpected high seroprevalence of P. ovale spp. and P. malariae in Beninese blood donors.
For the present study, a specific P. vivax ELISA was developed using recombinant P. vivax merozoite surface protein 1 (rPvMSP1) and circumsporozoite protein 1 (rPvCSP1). Performance of this assay was first assessed in both French travellers positive for P. vivax and non-exposed-to-Plasmodium French blood donors. Then, the seroprevalence of P. vivax in an asymptomatic Beninese blood donor population was further explored for the first time.
Methods
Samples from Plasmodium vivax infected patients
Sera from 41 P. vivax-infected patients from French Guyana and Venezuela were used for the initial study. Diagnosis and species identification were carried out by means of the microscopical observation of blood smears and then confirmed by PCR, as previously described [19]. This population was employed in order to determine the sensitivity and positive predictive value of ELISA.
Negative controls
Blood donor samples were collected at the Etablissement Français du Sang d’Alsace (EFS Alsace). Donors were classified as unexposed-to-malaria (280 samples) if their questionnaire responses indicated that they had never travelled to a malaria-endemic area. These samples were used to assess ELISA’s specificity and negative predictive value.
Samples from Beninese blood donors
Plasma and total blood samples from blood donors without apparent malaria symptoms (n = 1234) were collected over 10 months (May 2009 to February 2010) in six Beninese departmental blood centres [20]. Each donor signed a consent form, and both the Direction of Benin National Blood Transfusion Agency and Research Ethics Committee of the Republic of Benin validated the protocol. This population had been previously studied in order to determine the specific seroprevalence of P. falciparum, P. ovale spp. and P. malariae in Benin using species-specific ELISA [18]. Quantification of circulating pLDH was also performed.
Recombinant proteins
Nucleotide sequences encoding 203 AA (amino acids) of P. vivax merozoite surface protein 1 (rPvMSP1; Accession number AAA63427.1) and 259 AA of P.vivax circumsporozoite protein 1 (rPvCSP1; P08677.2) were cloned into expression vector pMAL-c2X (New England BioLabs, Ipswich, MA, USA). Both recombinant proteins were produced by Escherichia coli expression hosts and purified on amylose resin and DEAE Sepharose ® (GE healthcare, Uppsala, Sweden).
ELISA assays
Recombinant protein antibody screening was carried out using an in-house ELISA test derived from a commercial assay (DiaMed) [21]. rPvMSP1 and rPvCSP1 were immobilized overnight on 96-well plates at 4 °C in coating buffer and blocked for 1 h with phosphate buffered saline (PBST) with Tween 0.05% containing 1% bovine serum albumin (BSA) (Merck, Darmstadt, Germany). After washing with PBST, 200μL of diluent buffer (PBST with BSA 0.1%) were dispensed into each well and 10μL of serum incubated for 1 h at 37 °C. Using the same plate, 10 μL of positive and negative controls in triplicate were added. After three washes with PBST, 100 μL of horseradish peroxidase-labelled, monoclonal rabbit anti-human IgG (Sigma-Aldrich, St Quentin, France) were incubated for 30 min at 37 °C. After three washes with PBST, 100 μL of tetramethylbenzidine (TMB) plus substrate solution (Kem-en-tec, Denmark) were incubated for 15 min at 37 °C and the reaction was stopped with 50 μL of 0.5 M sulfuric acid. The absorbance was read within 30 min at 450 nm against 620 nm. Test validation required the positive OD to be >0.500 and the negative OD < 0.200. Average OD values for the 280 malaria-unexposed controls were 0.109 ± 0.095 and 0.112 ± 0.120 for rPvMSP1 and rPvCSP1, respectively. The cut-off value was set at three-fold the negative control wells’ average OD. The antibody (Ab) index of each sample was defined as ratio of its OD value and the cut-off value. The sample was considered positive if the Ab index was ≥1, and negative if the Ab index was <1. All assays were fully automated and performed on an EVOLIS Microplate System (Bio-Rad) at the Microbiology Department of the Hôpitaux Universitaires de Strasbourg.
Blood DNA extraction
Total DNA from 1 mL of whole blood sample was extracted using the QIAmp Blood DNA mini kit® (Qiagen, Hilden, Germany) according to the manufacturer’s recommendations and eluted in a final volume of 200 µL.
Nested-PCR for the diagnosis and species identification of Plasmodium infection
Search for Plasmodium sp. using nested-PCR was conducted, as previously described [22]. Briefly, the reaction mix contained 1× GoTaq Green mix (Promega), 2 mM of MgCl2, 0.2 mM of dNTPs, 0.5 µM of primers, and 5 µL of DNA template (or PCR product) in a 50 µL final volume. First round of PCR was carried out using rPLU5 and rPLU6 and nested using rViv1 and rViv2 primers for detecting P. vivax, rFAL1 and rFAL2 for P. falciparum, rMAL1 and rMAL2 for P. malariae, rOVA1 and rOVA2 for P. ovale curtisi [22], and rOVA1v and rOVA2v for P. ovale wallikeri [23]. Amplification consisted in an initial denaturation step of 3 min at 95 °C, which was followed by 40 cycles of 30 s at 95 °C, and then 30 s at 58 °C, and thereafter of 1 min at 72 °C (30 s for the nested).
Duffy genotype determination
Duffy genotype was assessed by sequencing the ~516 bp region of the gene encoding Duffy antigen as previously described [12, 24]. PCR products were sequenced by MWG Eurofins (Germany). Analysis of this sequence allows the T-33C mutation in the Duffy gene promoter to be detected. Single-nucleotide polymorphism (SNP) abolishes the expression of Duffy antigen in erythroid cells.
Statistical analysis
Epidemiological data analyses were performed using the Chi squared test. Correlation coefficients were calculated using Pearson’s coefficients. Comparison between r 2 values was carried out using Williams’ t test for dependent data. A p value below 0.05 was considered statistically significant. Statistical analyses were conducted using GraphPad Prism® software.
Results
Assessment of rPvMSP1 and rPvCSP1 ELISA
The assay sensitivity was first evaluated on 41 sera from P. vivax-positive febrile patients diagnosed using microscopy and then confirmed by species-specific PCR. Specificity was subsequently evaluated on 280 sera from non-exposed-to-malaria French blood donors. The rPvMSP1 and rPvCSP1 ELISA sensitivity values were 68.3 and 70.7%, respectively (Table 1). Specificity values were 99.3 and 96.8%, respectively, providing a better predictive positive value for rPvMSP1 ELISA (93.3%) as compared to rPvCSP1 (76.3%). Negative predictive values were similar between both assays, namely 95.5 and 95.8%, respectively. The test performance when combining the two ELISA (positive results for both rPvMSP1 and rPvCSP1, and negative if one of the two was negative) was also evaluated. When using this combination, sensitivity in P. vivax patients decreased to 53.7%, whereas both specificity and positive predictive values reached 100%, along with a 93.6% negative predictive value.
Plasmodium vivax seroprevalence study in Beninese blood donors
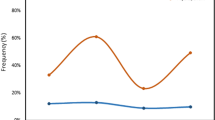
The recombinant antigens were used in order to evaluate P. vivax seroprevalence in a panel of 1234 Beninese blood donors. This cohort had previously been studied in order to assess the presence of antibodies directed against P. malariae, P. ovale spp. and P. falciparum species [18]. Anti-rPvMSP1 antibodies were detected in 28.7% (354/1234) of the Beninese population, and anti-rPvCSP1 in 21.6% (266/1234), with concomitant detection of both anti-rPvMSP1 and anti-rPvCSP1 in 15.2% of the cohort (187/1234). Data from a previous study were employed in order to determine the percentage of subjects also presenting with specific antibodies against other Plasmodium species [18, 21]. As shown in Table 2, many Beninese blood donors displayed antibodies against at least one other Plasmodium species. To evaluate possible cross-reactions between these malarial recombinant proteins, the correlation coefficient was calculated as previously described, and linear regressions were performed (Fig. 1) for the antigen pair indexes (rPvMSP1/rPvCSP1, rPoMSP1/rPvMSP1, rPoMSP1/rPvCSP1, rPmMSP1/rPvMSP1, rPmMSP1/rPvCSP1, rPfMS1-rPfAMA1/rPvMSP1, rPfMS1-rPfAMA1/rPvCSP1) [25]. There was a highly significant correlation between rPvMSP1 and rPvCSP1 indexes (r 2 = 0.3033; p < 0.05; see Additional file 1: Table S1). While the correlation coefficients between other pairs were also significant, the rPvMSP1/rPvCSP1 p value proved to be the lowest (Additional file 1: Table S1). Thereafter, the r 2 value of the rPvMSP1/rPvCSP1 pair was compared to other pairs (Additional file 1: Table S1). Statistical analyses confirmed that rPvMSP1/rPvCSP1 r 2 value was significantly higher than that of all other pairs. Analyses of epidemiological data did not reveal any correlation between P. vivax infection and age. However, males were significantly more frequently seropositive for rPvMSP1 than for rPvCSP1 (Table 3), this difference between males versus females remaining significant even after combining both antigens.
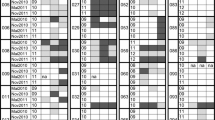
Plasmodium vivax detection by nested-PCR in Beninese blood donors
Direct research of P. vivax was performed using nested-PCR, targeting a small region (~120 bp) of the ssrRNA gene [22, 23]. To enhance the probability to found P. vivax-positive subjects, blood samples (see flow diagram, Fig. 2) that were positive for circulating pan-pLDH antigen, with positivity for either rPvMSP1 or rPvCSP1 ELISA or for both, were selected. A total of 84 samples fulfilled these criteria, of which 25 were positive for Plasmodium sp. using nested PCR with 20/25 P. falciparum, 1/25 P. ovale spp., 2/25 P. malariae, and 13/25 P. vivax. Nine subjects were simultaneously infected by both P. vivax and P. falciparum, and one by P. falciparum, P. malariae, and P. vivax. To confirm P. vivax detection, the 13 nested-PCR products were sequenced. Chromatograms were interpretable for seven of them, thereby confirming the presence of P. vivax (Additional file 2: Fig. S1. Accession numbers KY014285-KY014291).
Duffy determination
Duffy statute of the 13 subjects with a positive P. vivax-nested-PCR was established by sequencing. Homozygous T-33C mutation was detected in all 13 subjects, thereby indicating that these subjects were Duffy-negative.
Discussion
Over the last decade, a new vision of the transmission of P. vivax in Africa has emerged, with evidence of its presence in West Africa [26]. Likewise, the dogma of Duffy-negativity protecting effect against P. vivax infection has being challenged [26]. New P. vivax mapping has been recently proposed, highlighting numerous grey areas in the knowledge [26]. As a result, the real burden of P. vivax in Africa is still unknown. Different hypotheses may account for the partial view of P. vivax epidemiology in Africa, including the dogma of Duffy’s protectivity, low parasitaemia of P. vivax compared to P. falciparum and inappropriate diagnostic tools for accurate large-scale screenings [27]. Difficulties with microscopy diagnosis were encountered in the first studies using PCR, revealing the presence of P. vivax in western Africa, where it was supposed to be absent [26]. Moreover, microscopy was shown to require experienced operators in order to avoid misidentification between P. ovale spp. and P. vivax [14].
Regarding the epidemiology of P. vivax in Africa, symptomatic subjects probably represent only the tip of the iceberg. Given this background, studies including large cohorts of asymptomatic subjects, such as in the present work, will be likely prove in this research field. It should be acknowledged, however, that parasitaemia in asymptomatic carriers was shown to be very low, making the use of direct diagnosis tools for the detection of these cryptic infections very challenging [8]. Furthermore, both PCR and microscopy are not able to exclude previously-cured P. vivax infections. For these reasons, a species-specific ELISA assay was developed in the present study in order to determine the P. vivax seroprevalence in large-scale cohorts of Beninese healthy people.
Benin is located in the intertropical region of West Africa, its climate considered warm with four seasons, two dry and two rainy [20]. Given that major Anopheles species vectors of P. vivax are present, Benin meets all the required conditions for a potential constant parasite transmission [28, 29]. However, the prevalence of P. vivax in Benin has never been studied before. Recombinant proteins were produced using regions of PvMSP1 and PvCSP1. Both proteins have been previously studied for their immunogenicity properties, while representing potential vaccine targets [30].
Given that the present study sought to explore P. vivax presence in Beninese blood donors, ELISA’s cut-off values were adjusted to favour the test’s specificity and positive predictive values. Sensitivities of this assays were approximately 70%, which may be accounted for by using the sera from travellers suffering from acute infection while having not yet produced antibodies against P. vivax, as previously reported for P. falciparum [21]. Plasmodium vivax seroprevalence in Beninese blood donors ranged from 28.7 to 15.2% when considering only either rPvMSP1 results or the combination with rPvCSP1. The present study was the first to investigate P. vivax presence in Benin, and only two prior studies investigated P. vivax seroprevalence in West Africa. Based on these study results, 13 and 5.2% of subjects from the Republic of the Congo and the Cameroon, respectively, exhibited antibodies specifically directed against specific P. vivax antigens [11, 25]. Results from the present study confirmed that the P. vivax seroprevalence in peoples living in West Africa amounts to at least 10%, if not more. In the present work, seroprevalence in males was significantly higher than in females, with the opposite being previously reported from the Republic of Congo [25], thereby pointing towards differences between the different areas as to the epidemiology and likely risk factors.
In a previous study, the same Beninese blood donor population was employed in order to assess species-specific ELISA for the diagnosis of P. falciparum, P. ovale wallikeri/curtisi and P. malariae [18]. While integrating these previous results into the present study, it was observed that most of the subjects with P. vivax antibodies were also reactive to one or more other Plasmodium species. Whereas significant correlation factors were observed between rPvCSP1 or rPvMSP1 indexes and other species-specific antigens, it was not consider this to correspond to cross-reactivity between epitopes. As a matter of fact, all Beninese blood donors were shown to live in co-endemic areas with active transmission of P. falciparum, P. ovale spp. and P. malariae. The same observation was made by Culleton et al., who concluded that this correlation was predictive of that exposure to infection by one malaria species would also be predictive of the risk as to exposure to another malaria species [25]. Moreover, statistical analyses confirmed that the correlation coefficient factor value of rPvCSP1/rPvMSP1 index was significantly higher than that of others. In order to definitively assess results from the present study, molecular diagnosis using nested-PCR was performed. As discussed above, antibody detection does not mean the parasite to be present in Beninese blood donors at the time of sampling. Subjects with a higher risk of having circulating P. vivax in their blood where therefore selected. Selection criteria were based on both rPvCSP1 and rPvMSP1 positive results, in association with the detection of pLDH circulating antigen. Among the 1234 Beninese blood donors, 84 fulfilled these criteria, of which 13 were positive for the P. vivax-nested-PCR. Plasmodium falciparum DNA was also detected in nine of them, with one subject being positive for P. vivax, P. falciparum and P. malariae. These results thus reinforce the hypothesis of multiple anti-Plasmodium sp. antibody detection among Beninese blood donors as DNAs from three different Plasmodium species may be present in the same individual. It has to be assumed that multiple plasmodial infections may be detected in the same subject/patient via serology screening and, therefore, that microscopy remains the gold standard diagnostic tool, which should be followed by species-specific PCR, and this especially for submicroscopic cases. However, present results also explain the difficulties associated with microscopy diagnosis of P. vivax in regions of high multiple endemic Plasmodium species. Plasmodium vivax-nested-PCR products sequencing confirmed the presence of P. vivax. While it has to be acknowledged that these short sequences did not enable further strain comparison, it must be stressed that it was impossible to amplify longer sequences, thereby reflecting the very-low parasitaemia in these samples.
Based on both serology and PCR results, the present study highlights an unexpected high prevalence of P. vivax in the Beninese population, whereas the Duffy-negative phenotype is expected to reach 98–100% [31]. Duffy phenotype was assessed in the 13 subjects with positive P. vivax-nested-PCR. All were Duffy-negative, confirming that the Duffy-negative status does not constitute a barrier for P. vivax infection, as previously reported [9]. This finding strongly suggests that P. vivax may be able to use alternative pathways so as to invade red blood cells [32].
Results from the present study, combined to previous ones, suggest that serological assays are probably the most powerful tools aimed to investigate the burden of P. vivax in western Africa. After the first studies providing irrevocable proof of the presence of P. vivax presence while using molecular tools on small targeted populations, large-scale investigations using serology are now required. Moreover, the present study demonstrates that molecular approaches do only detect a small number of carriers while widely underestimating the prevalence of P. vivax, especially in low endemic settings.
Conclusion
Plasmodium vivax is now well-recognized to be involved in severe attacks and is able to develop treatment-resistance. While prophylactic and therapeutic efforts are rightly focused on P. falciparum, the epidemiological impact of P. vivax must thus also be taken into account. For P. vivax, given that transmission is generally lower, measuring transmission while using routine diagnosis tools may prove difficult. Molecular and serological methods are thus necessary in order to assess the real disease burden. The present results demonstrate that seroprevalence can be used as an additional tool to identify new areas of vivax malaria transmission. This information as well as the prevalence of all malaria species will likely prove essential for the successful implementation of malaria control and elimination programmes [27, 33].
References
WHO. World Malaria report. Geneva, World Health Organization, 2015. http://www.who.int/mediacentre/factsheets/fs094/en/.
Danis K, Lenglet A, Tseroni M, Baka A, Tsiodras S, Bonovas S. Malaria in Greece: historical and current reflections on a re-emerging vector borne disease. Travel Med Infect Dis. 2013;11:8–14.
Moreira CM, Abo-Shehada M, Price RN, Drakeley CJ. A systematic review of sub-microscopic Plasmodium vivax infection. Malar J. 2015;14:360.
Miller LH, Mason SJ, Clyde DF, McGinniss MH. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N Engl J Med. 1976;295:302–4.
Carvalho TA, Queiroz MG, Cardoso GL, Diniz IG, Silva AN, Pinto AY, et al. Plasmodium vivax infection in Anajas, State of Para: no differential resistance profile among Duffy-negative and Duffy-positive individuals. Malar J. 2012;11:430.
Cavasini CE, de Mattos LC, Couto AA, Couto VS, Gollino Y, Moretti LJ, et al. Duffy blood group gene polymorphisms among malaria vivax patients in four areas of the Brazilian Amazon region. Malar J. 2007;6:167.
Woldearegai TG, Kremsner PG, Kun JF, Mordmüller B. Plasmodium vivax malaria in Duffy-negative individuals from Ethiopia. Trans R Soc Trop Med Hyg. 2013;107:328–31.
Lo E, Yewhalaw D, Zhong D, Zemene E, Degefa T, Tushune K, et al. Molecular epidemiology of Plasmodium vivax and Plasmodium falciparum malaria among Duffy-positive and Duffy-negative populations in Ethiopia. Malar J. 2015;14:84.
Menard D, Barnadas C, Bouchier C, Henry-Halldin C, Gray LR, Ratsimbasoa A, et al. Plasmodium vivax clinical malaria is commonly observed in Duffy-negative Malagasy people. Proc Natl Acad Sci USA. 2010;107:5967–71.
Wurtz N, Mint Lekweiry K, Bogreau H, Pradines B, Rogier C, Ould Mohamed Salem Boukhary A, et al. Vivax malaria in Mauritania includes infection of a Duffy-negative individual. Malar J. 2011;10:336.
Fru-Cho J, Bumah VV, Safeukui I, Nkuo-Akenji T, Titanji VP, Haldar K. Molecular typing reveals substantial Plasmodium vivax infection in asymptomatic adults in a rural area of Cameroon. Malar J. 2014;13:170.
Ngassa Mbenda HG, Das A. Molecular evidence of Plasmodium vivax mono and mixed malaria parasite infections in Duffy-negative native Cameroonians. PLoS ONE. 2014;9:e103262.
Mendes C, Dias F, Figueiredo J, Mora VG, Cano J, de Sousa B, et al. Duffy negative antigen is no longer a barrier to Plasmodium vivax-molecular evidences from the African West Coast (Angola and Equatorial Guinea). PLoS Negl Trop Dis. 2011;5:e1192.
Mukadi P, Lejon V, Barbe B, Gillet P, Nyembo C, Lukuka A, et al. Performance of microscopy for the diagnosis of malaria and human African trypanosomiasis by diagnostic laboratories in the Democratic Republic of the Congo: results of a nation-wide external quality assessment. PLoS ONE. 2016;11:e0146450.
Goncalves BP, Drakeley C, Bousema T. Infectivity of microscopic and submicroscopic malaria parasite infections in areas of low malaria endemicity. J Infect Dis. 2016;213:1516–7.
Visser T, Daily J, Hotte N, Dolkart C, Cunningham J, Yadav P. Rapid diagnostic tests for malaria. Bull World Health Organ. 2015;93:862–6.
Nankabirwa JI, Yeka A, Arinaitwe E, Kigozi R, Drakeley C, Kamya MR, et al. Estimating malaria parasite prevalence from community surveys in Uganda: a comparison of microscopy, rapid diagnostic tests and polymerase chain reaction. Malar J. 2015;14:528.
Doderer-Lang C, Atchade PS, Meckert L, Haar E, Perrotey S, Filisetti D, et al. The ears of the African elephant: unexpected high seroprevalence of Plasmodium ovale and Plasmodium malariae in healthy populations in Western Africa. Malar J. 2014;13:240.
Filisetti D, Bombard S, N’Guiri C, Dahan R, Molet B, Abou-Bacar A, et al. Prospective assessment of a new polymerase chain reaction target (STEVOR) for imported Plasmodium falciparum malaria. Eur J Clin Microbiol Infect Dis. 2002;21:679–81.
Atchade PS, Doderer-Lang C, Chabi N, Perrotey S, Abdelrahman T, Akpovi CD, et al. Is a Plasmodium lactate dehydrogenase (pLDH) enzyme-linked immunosorbent (ELISA)-based assay a valid tool for detecting risky malaria blood donations in Africa? Malar J. 2013;12:279.
Doderer C, Heschung A, Guntz P, Cazenave JP, Hansmann Y, Senegas A, et al. A new ELISA kit which uses a combination of Plasmodium falciparum extract and recombinant Plasmodium vivax antigens as an alternative to IFAT for detection of malaria antibodies. Malar J. 2007;6:19.
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–20.
Calderaro A, Piccolo G, Perandin F, Gorrini C, Peruzzi S, Zuelli C, et al. Genetic polymorphisms influence Plasmodium ovale PCR detection accuracy. J Clin Microbiol. 2007;45:1624–7.
Chittoria A, Mohanty S, Jaiswal YK, Das A. Natural selection mediated association of the Duffy (FY) gene polymorphisms with Plasmodium vivax malaria in India. PLoS ONE. 2012;7:e45219.
Culleton R, Ndounga M, Zeyrek FY, Coban C, Casimiro PN, Takeo S, et al. Evidence for the transmission of Plasmodium vivax in the Republic of the Congo, West Central Africa. J Infect Dis. 2009;200:1465–9.
Howes RE, Reiner RC Jr, Battle KE, Longbottom J, Mappin B, Ordanovich D, et al. Plasmodium vivax transmission in Africa. PLoS Negl Trop Dis. 2015;9:e0004222.
Stevenson JC, Stresman GH, Baidjoe A, Okoth A, Oriango R, Owaga C, et al. Use of different transmission metrics to describe malaria epidemiology in the highlands of western Kenya. Malar J. 2015;14:418.
Malaria Atlas Project. http://www.map.ox.ac.uk/.
Gething PW, Van Boeckel TP, Smith DL, Guerra CA, Patil AP, Snow RW, et al. Modelling the global constraints of temperature on transmission of Plasmodium falciparum and P. vivax. Parasit Vectors. 2011;4:92.
Chenet SM, Tapia LL, Escalante AA, Durand S, Lucas C, Bacon DJ. Genetic diversity and population structure of genes encoding vaccine candidate antigens of Plasmodium vivax. Malar J. 2012;11:68.
Howes RE, Patil AP, Piel FB, Nyangiri OA, Kabaria CW, Gething PW, et al. The global distribution of the Duffy blood group. Nat Commun. 2011;2:266.
Gruszczyk J, Lim NT, Arnott A, He WQ, Nguitragool W, Roobsoong W, et al. Structurally conserved erythrocyte-binding domain in Plasmodium provides a versatile scaffold for alternate receptor engagement. Proc Natl Acad Sci USA. 2015;113:191–200.
Lynch C, Cook J, Nanyunja S, Bruce J, Bhasin A, Drakeley C, et al. Application of serological tools and spatial analysis to investigate malaria transmission dynamics in highland areas of Southwest Uganda. Am J Trop Med Hyg. 2016;94:1251–8.
Authors’ contributions
EC and AS designed the study. CDL produced recombinant proteins and performed molecular assays. JPL, LM, EH, and MLC performed ELISA assays on BBD sera. PSA, NWC, CDA, LA, and AB recruited Beninese blood donors and collected epidemiological data in Benin. AAB, AWP, JB, SP, and DF processed the samples and collected the data in France. PP, CDL and EC analysed data and prepared the report. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank the technicians Rachel Huber and Sylvie Mattern from the Microbiology Department at the Hôpitaux Universitaires de Strasbourg for technical expertise.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets pertaining to the current study may be made available by the corresponding author, on reasonable request.
Ethics approval and consent to participate
Each donor signed a consent form, and both the Direction of Benin National Blood Transfusion Agency and Research Ethics Committee of the Republic of Benin validated the protocol.
Funding
This work was supported by the Project CONECTUS Project on transfusion malaria diagnosis. PSA was supported by a grant from the Benin Government.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Philippe Poirier, Cécile Doderer-Lang, Ambaliou Sanni and Ermanno Candolfi contributed equally to this work
Additional files
12936_2016_1620_MOESM2_ESM.docx
Additional file 2: Fig. S1. Sequence alignment of the seven Plasmodium vivax sequence from nested-PCR. Sequence variations are highlighted by black boxes.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Poirier, P., Doderer-Lang, C., Atchade, P.S. et al. The hide and seek of Plasmodium vivax in West Africa: report from a large-scale study in Beninese asymptomatic subjects. Malar J 15, 570 (2016). https://doi.org/10.1186/s12936-016-1620-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1620-z