Abstract
Background
Malaria the first causes of death from parasitic infection worldwide. Interventions to reduce the burden of malaria have produced a tremendous drop in malaria morbidity and mortality. However, progress is slower in DRC, which shares with Nigeria 39% of deaths related to malaria globally. Inappropriate use of drugs may be one of the factors of this below-average performance. The aim of this study was to describe the use of drugs in the management of uncomplicated malaria in public health facilities in DRC.
Methods
A drug use study was carried out in DRC from January to March 2014. In each of the former 11 provinces of DRC, one Rural Health Centre, one Urban Health Centre and one General Hospital were selected. In each of them, 100 patient’s files containing prescription of anti-malarials from January to December 2013 were randomly selected. Among them, all of the files with diagnosis of uncomplicated malaria were included in this study. Prescribed anti-malarials, co-prescribed drugs and their indications were collected. Descriptive analyses were performed.
Results
A total of 2300 files out of 3300 (69.7%) concerned uncomplicated malaria and were included in analysis. Malaria treatment was initiated after a positive RDT or microscopy in 51.5% of cases, upon suspicion without requesting biological confirmation in 37% and despite negative results in 11%. Twenty-nine (29) different treatment regimens were used. The drugs recommended by the National Malaria Control Programme were used in 54.3% of cases (artesunate–amodiaquine 37.4% or artemether–lumefantrine 16.9%). The second most used anti-malarial was quinine (32.4%). Apart from anti-malarials, an average of 3.1 drugs per patient were prescribed, among which antibiotics (67.9%), analgesics and non-steroidal anti-inflammatory (NSAIDs) (all abbreviations to be explicated on first use) (70.6%), vitamins (29.1%), anaemia drugs, including blood transfusion (9.1%) and corticosteroids (5.7%), In 51.4% of cases there was no indication for the concomitant medication.
Conclusion
Management of uncomplicated malaria in DRC is characterized by a low adherence to treatment policy, numerous treatment regimens, and abundant concomitant medication potentially harmful to the patient. This may contribute to the low performance of DRC in malaria control. Determinant of this irrational use of drugs need to be assessed in order to formulate and implement efficient corrective measures.
Similar content being viewed by others
Background
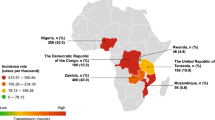
Malaria is the first cause of death from parasitic infection worldwide. Developing tropical countries are the most affected. There were about 212 million cases of malaria in 2015 and an estimated 429,000 deaths among which 90% lived in the African region [1]. In the Democratic Republic of the Congo (DRC), 97% of the population is at risk of endemic malaria and the remaining 3% is exposed to malaria epidemics.
Fighting malaria involves many organizations at international and national level and the disease was included in the Millennium Development Goal (MDG 6c); which was to halt and begin to reverse the incidence of malaria by 2015 [2]. In 2005, the World Health Assembly (WHA) set the targets of reducing malaria case incidence rates by 75% by 2015 [2, 3]. As a result, the average malaria infection prevalence declined by 48% in children aged 2–10 years, mortality decreased by 47% worldwide and by 54% in the World Health Organization (WHO) Africa Region between 2000 and 2015, and 55 countries met the target set by the MDGs [1]. However, DRC is not on track to achieve the MDG or WHA targets; instead, it is among the 13 countries that carry 78% of the burden of malaria and in which the reduction of malaria incidence of 32% since 2000 is below the average of 53% in the other countries globally [2]. With about 1% of the world population [3] and 1.7% of those exposed to malaria, DRC had 9% of malaria cases and 10% of malaria deaths in 2015 and together with Nigeria a share of 36% of deaths related to malaria globally [1]. Inappropriate use of drugs may be among the determinants of this counter performance.
Inappropriate use of anti-malarials [4, 6], poor adherence to treatment guidelines [5, 7], lack of laboratory data supporting diagnosis of malaria before treatment [6, 8] or usage of drugs known to be ineffective [7] have been reported from African countries affected with malaria. In addition to anti-malarials, other drugs e.g., antibiotics, are irrationally used during malaria treatment [8, 10]. In DRC, an unpublished study of Mesia et al. found that the recommended ACT was only used by 6% of healthcare providers three years after implementation of artesunate/amodiaquine as first-line treatment for uncomplicated malaria. The situation had not changed much in 2014: 6% of children under 5 years with fever received an ACT [9].
There is an apparent need to improve rational use of anti-malarials, but without a knowledge basis of how drugs are being prescribed and used, it is difficult to initiate a discussion on rational drug use or to suggest measures to improve prescribing habits [10]. Taking this into account, it is of paramount importance to first assess the current practices in the use of anti-malarial drugs. The aim of this study is to describe the prescription of drugs in the management of uncomplicated malaria in Public Health facilities in DRC.
Methods
Study setting
DRC is the second largest and the fourth most populated country of Africa with a population estimated to 81 million inhabitants [11] The health system of DRC is composed of 515 Health Zones, each of them comprising one General Referral Hospital (GRH) and several Health Centres (HC). Most of them are integrated in the national health system and thus connected to the National Malaria Control Programme. Current, treatment policy of malaria in DRC [12] recommends that uncomplicated malaria is to be managed in HC, while severe malaria is managed in Referral Hospitals. HC are rural or urban according to their geographical location: rural areas are characterized by more poverty, less qualified health personnel, difficulties in transportation and all social services. Urban areas are characterized by more qualified health personnel, some better social services, but also more promiscuity. HC are mostly run by nurses especially in rural areas; physicians may sometimes be found in urban health centres but are mostly responsible of patient care in GRH. The study was carried out in all the previous 11 provinces of DRC. In each one of them, one GRH, one rural HC and one urban HC were selected to capture use of drugs in complicated, in uncomplicated malaria, as well as urban and rural conditions. DRC has been through many civil wars and there are still armed groups in many remote areas especially in the eastern regions. Therefore, the study was conducted in the Capital cities and the surrounding rural areas in each province. This is also where the population fleeing the abuses of the armed groups converge. The total catchment area covered by these health facility is approximately 4.5 million inhabitants according to the date provided by the Health Zones. The recommended drugs for uncomplicated malaria are artesunate + amodiaquine (ASAQ) or artemether + lumefantrine (AL).
Study design
This was a cross-sectional drug use study that aimed at assessing the prescription of anti-malarial drugs. Therefore, a retrospective review of patients’ file containing a prescription of an anti-malarial from January to December 2013 was performed. One hundred files were randomly selected in each health facility as recommended by WHO in the investigation about drug use in health facilities [13], yielding a sample size of 3300 files. The data were collected from January to March 2014. Patients’ files were thereafter classified according to the diagnosis of malaria recorded by the prescriber: uncomplicated malaria, treatment failure, severe malaria, and are kept electronically as Excel spreadsheets.
Only the patients’ file in which the indication of anti-malarial prescription was uncomplicated malaria were included in this study. All cases of severe malaria or no malaria diagnosis were excluded from the analysis. For each of them, the following variables were recorded: Province, health facility (GRH, urban HC or Rural HC), age, and medical history; clinical signs and symptoms as well as laboratory results supporting the diagnosis of malaria; and the drug prescribed (anti-malarials and co-prescribed medication with their indication). Data were entered using Epi-info 7, CDC Atlanta, then exported in Microsoft Excel 2013. Descriptive analyses were performed. Calculation of 95% confidence interval was performed using Stata 12.
Statistical analysis
Descriptive analyses were performed. Calculation of 95% confidence interval was performed using Stata 12.0 (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp).
Variables were described by count or frequencies. When necessary, Chi square tests was used to compare them in children less than 5 years old with other patients. A p value < 0.05% was considered for statistical significance.
Results
This drug use study was conducted in the 11 former provinces of DRC and analysed the patterns of the prescription of anti-malarial drugs in Health Centres and General Referral Hospitals. Of the 3300 patients’ files collected 2300 had uncomplicated malaria as the indication for anti-malarial drug prescription Tables 1 and 2.
Patients’ characteristics
About one-third of the patients (37.9% of cases) are children under 5 years of age. Among them, 6.3% (140/2227) were less than 6 months old.
Medical management
Confirmation of diagnosis prior to initiation of treatment
Confirmation of malaria by rapid diagnostic test (RDT) or microscopy was requested by the medical personnel only in 63% (1436/2300) of suspected cases; in 52% (1184/2300), the results were positive and in 11% (252/2300) of cases, malaria treatment was initiated despite negative results. In 2.6% of cases (59/2300), malaria diagnosis was based on both microscopy and RDT. Both were positive in 48 patients; in 11 cases, microscopy was positive but RDT negative. Table 3 shows that prescription of anti-malarial was based more frequently on positive results in children blow 5 years old.
Medical management of uncomplicated malaria
A total of 29 different treatments were used to manage uncomplicated malaria. The most used drugs were ASAQ, AL and quinine. As shown in Table 4 they were prescribed to 1994 patients (86.7%). They are are followed by the injectable artemisinin derivatives, alpha–beta arteether and artemether, then sulfadoxine-pyrimethamine (SP). The other drugs represented together 3.7%; each of them was used in less than 1% of patients. They include quinine containing treatments (quinine plus ACT, such as ASAQ, AL, dihydroartemisinin–piperaquine (DHA–PQ), quinine plus doxycycline, SP, artemether or artesunate); other ACT medicines, such as DHA–PQ and artesunate-SP and oral monotherapies, including oral artemisinin-based monotherapy (oAMT). Quinine and ASAQ were significantly more used in the subgroup of under 5 years old children the most affected by malaria whereas, artemether–lumefantrine and the injectable artemisinin derivative alpha–beta arteether were more used in the patients aged 5 years old and above.
Concomitant medication
Fifty-six patients (2.4%) received no other drug than anti-malarials. The other patient received an average of 3.1 drugs. Table 5 shows, for every concomitant medication, the number of patients that received it. Analgesics and NSAIDs were the most prescribed, to 70.6% of patients; antibiotics were prescribed to 68% of patients. Vitamins were prescribed to 29% of patients and the other anti-infectious drugs, mostly anti-helminthics were prescribed in 27.5% of cases. Antibiotics were used without a specified diagnosis in 56.2% of cases and for a non-bacterial infectious condition (vomiting, intestinal parasitosis, flu) in 16.6% of cases. Among antalgics, metamizole, a drug with known serious haematologic adverse reactions was prescribed to 12.2% of patients. Drug combinations used in influenza were prescribed to 6.1% of patients.
All age groups received concomitant medication. Table 6 shows that, significantly more children under five were prescribed antibiotics compared to other patients (75% vs. 63%). Antalgics, (74.7% vs. 68.3%), drugs used for anaemia, among which, iron salts, folate and vitamin B12 and blood transfusion (16.2% vs. 4.9%). Ten of the 11 blood transfusions were given to children of this age group. For the one remaining transfusion, age was not specified but the weight of the patient (8.5 kg) strongly suggests he is in this same age group. Corticosteroids and drugs used in the management of influenza were also significantly more prescribed to children under five. Prescription of vitamins was comparable in both groups.
Prescription of antibiotics was found to be comparable (p = 0.137802) in patients with positive biological confirmation, of malaria 69.1% (818/1184) and those with negative tests 74.2 (186/252). Surprisingly however, antibiotics were significantly less prescribed (p = 0.025078) in patients with no biological confirmation of malaria, 64.4% (549/853) than in patients with positive biological confirmation.
Discussion
Despite the use of the same powerful dugs, DRC is still heavily affected by malaria and concentrates 10% of all deaths related to malaria worldwide, most of whom are children under 5 years old. Inappropriate use of drugs in the management of this disease may play a significant role in this counter performance. This study aimed at assessing the use of drugs in the management of uncomplicated malaria in rural and urban health zones and referral hospitals. In each of the 11 provinces of DRC, only those in or near the capital cities were included. This is also where converge the population fleeing the abuses of armed groups. The stratification by province, and health facility, as well as the consideration of rural and urban aspects may contribute to increase the representativeness of our sample. In addition, the preponderance of patient aged less than 5 year could mean a rash between our sample and the population affected by malaria in DRC [9]. It is worth to notice the 6.3% of infants under 6 months. Malaria was thought to be rare in this age group for various reasons [14]. But more and more data suggest that malaria may not be as rare as previously thought and may be masquerading other severe infectious conditions [14] Thus; there is a need to understand more about the characteristic of malaria in this age group as well as their optimal treatment. The WHO has recognized the infants under 12 months [16] as one of the most vulnerable population. Use of long-lasting insecticidal nets (LLINs), intermittent preventive therapy with SP for infants (IPTi) and prompt diagnosis and effective treatment of malaria infections [16] have been recommended. For some of these infants, especially those weighing less than 5 kg, there is a lack of proven treatment options: none of the current ACT is approved for infants under 4.5 kg, and there are concerns about the safety of quinine in this age group [17] and, as shown for AL [18], pharmacokinetics of some drugs recommended for other age group, can be different in this group, leading to increased exposure to these substances. There is still a need for evidence to understand more about the best treatment for this vulnerable population that represents a non-negligible proportion of the malaria patients.
Malaria treatment was initiated without biological confirmation in almost half of the cases. This may results in wastage of drugs that should be given to true malaria cases [19], unnecessary and avoidable adverse drug reactions (ADR) and delay in the detection of the true illness of the patient which can be lethal [20]. Indeed the WHO and the Congolese NMCP have recommended biological confirmation of malaria by either RDT or microscopy before initiation of treatment. However, the performance of diagnostic tests prior to treatment is not a guarantee of optimal use of anti-malarials. Malaria treatment initiated despite negative results in 11% of cases which is in line with other studies [21, 22] with a rate of malaria treatment despite negative laboratory testing diagnosis of as high as 58% in Nigeria [21]. This inappropriate prescription of anti-malarials despite negative results may be caused by the assumption of undetectable malaria, lack of tools for alternative diagnosis, provider know-how and time, the patients demand for drugs [23], lack of trust in laboratory results, constancy of anti-malarial supply and resistance to change from pre-existing patterns [24]. Another issue is the drug prescribed: The recommended ACT formulations, ASAQ and AL, were prescribed in only half of the cases. Patients below 5 years old were more likely to be prescribed ASAQ or quinine whereas the older patient received more AL and alpha–beta arteether. Currently, ACT is the best choice for management of uncomplicated malaria. The demonstrated efficacy and safety of ASAQ [25, 26] and AL [27, 28] have led the NMCP of DRC to recommend them [12] for management of uncomplicated malaria. On the other hand quinine use in malaria treatment was established before the methods for modern clinical trials were developed [29]; this drug has a low therapeutic index [17], which means an increased risk of dose-related adverse reactions. In addition, head to head studies have shown superiority of ACT over quinine in the management of uncomplicated malaria [30, 31]. Despite these evidences, quinine continue to be used (up to 40% in children under 5 years old). One of the reasons would be that this drug has been used against malaria for a long time. The drug is so popular that in many areas of DRC that the word quinine has been included in local languages as a word for any tablet. Yet, the widespread usage of quinine may probably be playing a role in the low performance of DRC in malaria mortality and morbidity. The injectable artemether and alpha beta arteether were also used despite they are not recommended for uncomplicated malaria and there is no WHO prequalified product available [32]. The use of these injectable monotherapies in uncomplicated malaria may also fuel drug resistance like the oral artemisinin-based monotherapies (oAMT). Oral monotherapy of artesunate, dihydroartemisinin (DHA) and amodiaquine were used in 3, 4 and 1 patients, respectively. This seems very low, but there is still a concern: the WHO has identified use of oAMT as one of the major driver of resistance to artemisinin and its derivatives [33]. The regulatory authority of DRC has responded by withdrawing marketing authorization to oAMT [34], but these drugs are still prescribed and this raises also the question of the origin of these oAMT, their presence in pharmacies and unauthorized drug sellers and why they are still prescribed by health professionals. Compliance to treatment guidelines is a major factor of treatment success [35]. However, prescribers adhered to treatment policy in only half of the cases which is in line with findings from other countries in Sub-Saharan Africa [6,7,8]. This may be related to many factors like stock-outs, ignorance, the attempt to save money, difficulties to change habits or misleading incentives. Better organisation of health facilities and training of personnel may significantly increase adherence to national policy as shown in Uganda [36]. Nevertheless, adherence to treatment guidelines by health workers is not the end of the story; it is important to take in account adherence of the patient to the prescription. Onyango et al. have shown that adherence to prescription was very low especially in the poorest, less educated and younger patients [37]. So when assessing factors related to low adherence of prescribers to treatment policy, it is important to take in account the adherence of patients to treatment and related factors in order to put in place more adapted corrective measures. In addition to anti-malarials, the patients received other concomitant medication.
Uncomplicated malaria presents in the form of numerous unspecific signs and symptoms including most of the time headaches, fever, and pain which drive the prescription of antipyretic drugs, analgesics or NSAIDs. Paracetamol was the most prescribed, however, metamizole a drug known to induce rare but irreversible agranulocytosis [38, 39] was given to 12.3% of patients. Given this risk and considering the multiple alternatives the use of metamizole seems inappropriate.
More than 2/3 of patients were prescribed antibiotics. Children blow 5 years old were significantly more likely to be prescribed antibiotics, as shown in other studies [8, 40]. The lack of confirmation of malaria or negative results are among the drivers of antibiotic co-prescription with anti-malarials [41] But, surprisingly, prescription of antibiotics was comparable in patient with positive and negative parasitological exams. Patient for which confirmation of malaria was not sought were prescribed rather less antibiotics. Some Congolese prescribers assume inexplicably that better management of malaria requires addition of antibiotics to anti-malarials. Whether this is a misunderstanding of the recommendation to combine quinine with clindamycin or doxycycline, or no is not known. Nevertheless, this remains an issue that needs an assessment of extent and determinants in Congolese settings because it may be part of the irrational use of antibiotics which is common especially in developing countries and a major contributor to bacterial resistance [8, 42]. Considering the high prevalence of malaria in DRC and the high prescription of antibiotics for malaria, management of malaria may be threatening treatment of bacterial infection and this can cause significant problems to patients and health systems.
Vitamins, mostly multivitamins were prescribed to 29.1% of patients, without an indication mentioned in the files. There was no significant difference in prescription to children under-five compared to other patients. Neither the WHO guidelines nor the national guidelines recommend usage of vitamins in the management of malaria. Some studies have speculated that the antioxidant effect of vitamins, especially vitamin C and E, may reduce efficacy of artemisinin derivatives [43]. The same concern may be evoked regarding the use of iron whose supplementation in children has been shown to increase susceptibility to malaria [44, 45]. The effect of iron supplementation on the efficacy of ACT has not been assessed; however, a study in Malawi [46] showed reduction in efficacy of sulfadoxine-pyrimethamine in children receiving concomitantly SP and iron supplementation. Other studies [47, 48] has shown no beneficial effect iron supplementation during malaria treatment. In DRC where, 60% of children aged 6–59 months are affected by anaemia [9], these interactions need to be more assessed in order to propose more efficient strategies.
Blood transfusion in the context of management of malaria is used to improve oxygen delivery to tissue, due to severe anaemia. Eleven children under five received blood transfusion and the recorded indication was just anaemia. In severe malaria, blood transfusion may be necessary, but benefits of this procedure need to be weighed against risks of transmission of serious infectious diseases (HIV, hepatitis B) severe immunologic reactions, volume overload, hyperkalaemia [49]. Transfusions are necessary when the level of haemoglobin is so low that it is not tolerated and that may define severe malaria [29]. These 11 transfusions may be related to misclassification of complicated malaria cases as uncomplicated, or to the numerous unnecessary transfusions given to ambulatory patients.
Conclusion
DRC is still heavily affected by malaria despite the effectiveness of available tools to control this potentially lethal disease. Inappropriate use of those tools, namely medicines still hampers better control of the disease. Half of the patients receive malaria treatment with no diagnostic confirmation and adherence to treatment guidelines is low. Quinine, which is no more recommended for uncomplicated malaria is still widely used. In addition, the management of uncomplicated malaria is characterized by polypharmacy, mostly in children below 5 years old. Dangerous analgesics like metamisole are used. Antibiotics and other drugs, like vitamins, anaemia drugs and corticosteroids are prescribed, most of the time without an indication. The massive use of antibiotics raises the concerning question that management of uncomplicated malaria in DRC may be one of the drivers of selection of resistant bacteria which is a serious threat to public health. All these practices may be threatening the success of the control of malaria in DRC. There is a need to train all stakeholders in the proper management of uncomplicated malaria and make available all diagnostic tools, especially RDTs and the recommended drugs. The withdrawal of the non-recommended drug from the marked will also improve the management of uncomplicated malaria. The determinants of all these situations need to be assessed in order to formulate more accurate recommendations.
Abbreviations
- ACT:
-
Artemisinin-based combination therapy
- ADR:
-
adverse drug reaction
- AL:
-
artemether plus lumefantrine
- ASAQ:
-
artesunate plus amodiaquine
- DHA:
-
dihydroartemisinin
- DRC:
-
Democratic Republic of the Congo
- GRH:
-
General Reference Hospital
- HC:
-
Health Centre
- IV:
-
intravenous
- MDG:
-
millennium development goals
- NMCP:
-
National Malaria Control Programme
- NSAID:
-
non-steroidal anti inflammatory
- oAMT:
-
oral artemisinin based monotherapy
- PQ:
-
piperaquine
- RTD:
-
rapid diagnostic test
- SDG:
-
sustained development goals
- WHO:
-
World Health Organisation
References
WHO. World malaria report 2016. Geneva: World Health Organization; 2016.
WHO. World malaria report 2015. Geneva: World Health Organization; 2015.
République Démocratique du Congo. 2018. http://www.banquemondiale.org/fr/country/drc. Accessed 21 Apr 2018.
Oshikoya KA, Chukwura HA, Ojo OI. Evaluation of outpatient paediatric drug prescriptions in a teaching hospital in Nigeria for rational prescribing. Paediatr Perinat Drug Ther. 2006;7:183–8.
Mannan AA, Malik EM, Ali KM. Antimalarial prescribing and dispensing practices in health centres of Khartoum state, 2003–2004. East Mediterr Health J. 2009;15:122–8.
Okoro R, Nwambu J. Evaluation of physicians’ prescribing patterns of antimalarial drugs during pregnancy at the obstetrics and gynaecology department of a teaching hospital in Maiduguri, Borno state, Nigeria. Int J Pharm Biomed Sci. 2012;3:39–46.
Gardella F, Assi S, Simon F, Bogreau H, Eggelte T, Ba F, et al. Antimalarial drug use in general populations of tropical Africa. Malar J. 2008;7:124.
Means AR, Weaver MR, Burnett SM, Mbonye MK, Naikoba S, McClelland RS. Correlates of inappropriate prescribing of antibiotics to patients with malaria in Uganda. PLoS ONE. 2014;9:e90179.
Ministère du Plan et Suivi de la Mise en oeuvre de la Révolution de la Modernité (MPSMRM), Ministère de la Santé Publique (MSP) et ICF International. Enquête Démographique et de Santé en République Démocratique du Congo 2013–2014. Rockville, Maryland, USA: MPSMRM, MSP et ICF International; 2014.
WHO. Introduction to drug utilization research. Geneva: World Health Organization; 2003.
World Population Prospects—Population Division—United Nations. https://esa.un.org/unpd/wpp/. Accessed 21 April 2018.
Programme National de Lutte contre le Paludisme. Guide national de prise en charge du paludisme. Kinshasa: PNLP; 2012.
WHO. How to investigate drug use in health facilities. Geneva: World Health Organization; 1993. pp. 1–92. http://apps.who.int/medicinedocs/pdf/s2289e/s2289e.pdf.
D’Alessandro U, Ubben D, Hamed K, Ceesay SJ, Okebe J, Taal M, et al. Malaria in infants aged less than six months—is it an area of unmet medical need? Malar J. 2012;11:400.
Ojukwu J, Ezeonu C, Ogbu C. Severe malaria in neonates masquerading as septicaemia. Nigerian J Paediatr. 2004;31:48–55.
WHO. Malaria in infants. Geneva: World Health Organization; 2018.
Achan J, Talisuna AO, Erhart A, Yeka A, Tibenderana JK, Baliraine FN, et al. Quinine, an old anti-malarial drug in a modern world: role in the treatment of malaria. Malar J. 2011;10:144.
Tiono AB, Tinto H, Alao MJ, Meremikwu M, Tshefu A, Ogutu B, et al. Increased systemic exposures of artemether and dihydroartemisinin in infants under 5 kg with uncomplicated Plasmodium falciparum malaria treated with artemether-lumefantrine (Coartem®). Malar J. 2015;14:15.
Mwangi TW, Mohammed M, Dayo H, Snow RW, Marsh K. Europe PMC Funders Group Clinical algorithms for malaria diagnosis lack utility among people of different age groups. Trop Med Int Health. 2012;10:530–6.
Harchut K, Standley C, Dobson A, Klaassen B, Rambaud-Althaus C, Althaus F, et al. Over-diagnosis of malaria by microscopy in the Kilombero Valley, Southern Tanzania: an evaluation of the utility and cost-effectiveness of rapid diagnostic tests. Malar J. 2013;12:159.
Ezenduka CC, Okonta MJ, Esimone CO. Adherence to treatment guidelines for uncomplicated malaria at two public health facilities in Nigeria; Implications for the “test and treat” policy of malaria case management. J Pharm Policy Pract. 2014;7:15.
Mangham LJ, Cundill B, Ezeoke O, Nwala E, Uzochukwu BSC, Wiseman V, et al. Treatment of uncomplicated malaria at public health facilities and medicine retailers in south- eastern Nigeria. Malar J. 2011;10:155.
Altaras R, Nuwa A, Agaba B, Streat E, Tibenderana JK, Strachan CE. Why do health workers give anti-malarials to patients with negative rapid test results ? A qualitative study at rural health facilities in western Uganda. Malar J. 2016;15:23.
Burchett HED, Leurent B, Baiden F, Baltzell K, Björkman A, Bruxvoort K, et al. Improving prescribing practices with rapid diagnostic tests (RDTs): synthesis of 10 studies to explore reasons for variation in malaria RDT uptake and adherence. BMJ Open. 2017;7:e012973.
Schramm B, Valeh P, Baudin E, Mazinda CS, Smith R, Pinoges L, et al. Efficacy of artesunate-amodiaquine and artemether-lumefantrine fixed-dose combinations for the treatment of uncomplicated Plasmodium falciparum malaria among children aged six to 59 months in Nimba County, Liberia: an open-label randomized non-inferiority. Malar J. 2013;12:251.
Ndeba PM, Alessandro UD, Hennart P, Donnen P, Porignon D, Balaluka GB, et al. Efficacy of artesunate plus amodiaquine for treatment of uncomplicated clinical falciparum malaria in severely malnourished children aged 6–59 months, Democratic Republic of Congo. J Clin Exp Pathol. 2012;S3:005.
Ngasala BE, Malmberg M, Carlsson AM, Ferreira PE, Petzold MG, Blessborn D, et al. Efficacy and effectiveness of artemether-lumefantrine after initial and repeated treatment in children < 5 years of age with acute uncomplicated Plasmodium falciparum malaria in rural Tanzania: a randomized trial. Clin Infect Dis. 2011;52:873–82.
Getnet G, Fola AA, Alemu A, Getie S, Fuehrer H-P, Noedl H. Therapeutic efficacy of artemether-lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Enfranze, north-west Ethiopia. Malar J. 2015;14:258.
WHO. Treatment of severe malaria. Guidelines for the treatment of malaria. Geneva: World Health Organization; 2015. p. 71–88.
Alecrim MG, Lacerda MV, Mourãdieo MP, Alecrim WD, Padilha A, Cardoso BS, et al. Successful treatment of Plasmodium falciparum malaria with a six-dose regimen of artemether–lumefantrine versus quinine-doxycycline in the western Amazon region of Brazil. Am J Trop Med Hyg. 2006;74:20–5.
Achan J, Tibenderana JK, Kyabayinze D, Wabwire Mangen F, Kamya MR, Dorsey G, et al. Effectiveness of quinine versus artemether–lumefantrine for treating uncomplicated falciparum malaria in Ugandan children: randomised trial. BMJ. 2009;339:b2763.
Medicines/Finished Pharmaceutical Products, WHO—Prequalification of Medicines Programme; 2018. https://extranet.who.int/prequal/content/prequalified-lists/medicines?label = alpha + beta + arteether&field_medicine_applicant = &field_medicine_fpp_site_value = &search_api_aggregation_1 = &field_medicine_pq_date%5Bdate%5D = &field_medicine_pq_date_1%5Bdate%5D = &field. Accessed 21 April 2018.
Global Malaria Programme. Emergence and spread of artemisinin resistance calls for intensified efforts to withdraw oral artemisinin-based monotherapy from the market. Geneva: World Health Organization; 2014. p. 1–15.
WHO. Marketing of oral artemisinin-based monotherapy medicines at country level. Geneva: World Health Organization; 2014.
Zurovac D, Githinji S, Memusi D, Kigen S, Machini B, Muturi A, Otieno G, Snow R, Nyandigisi A. Major improvements in the quality of malaria case-management under the “test and treat” policy in Kenya. PLoS One. 2014;9(3):e92782.
Sears D, Kigozi R, Mpimbaza A, Kakeeto S, Sserwanga A, Staedke SG, et al. Anti-malarial prescription practices among outpatients with laboratory-confirmed malaria in the setting of a health facility-based sentinel site surveillance system in Uganda. Malar J. 2013;12:252.
Onyango EO, Ayodo G, Watsierah CA, Were T, Okumu W, Anyona SB, et al. Factors associated with non-adherence to artemisinin-based combination therapy (ACT) to malaria in a rural population from holoendemic region of western Kenya. BMC Infect Dis. 2012;12:143.
Huber M, Andersohn F, Sarganas G, Bronder E, Klimpel A, Thomae M, et al. Metamizole-induced agranulocytosis revisited: results from the prospective Berlin Case-Control Surveillance Study. Eur J Clin Pharmacol. 2015;71:219–27.
Stammschulte T, Ludwig WD, Mühlbauer B, Bronder E, Gundert-Remy U. Metamizole (dipyrone)-associated agranulocytosis. An analysis of German spontaneous reports 1990–2012. Eur J Clin Pharmacol. 2015;71:1129–38.
Ndhlovu M, Nkhama E, Miller JM, Hamer DH. Antibiotic prescribing practices for patients with fever in the transition from presumptive treatment of malaria to “confirm and treat” in Zambia: a cross-sectional study. Trop Med Int Health. 2015;20:1696–706.
Njozi M, Amuri M, Selemani M, Masanja I, Kigahe B, Khatib R, et al. Predictors of antibiotics co-prescription with antimalarials for patients presenting with fever in rural Tanzania. BMC Public Health. 2013;13:1097.
Akinyandenu O, Akinyandenu A. Irrational use and non-prescription sale of antibiotics in Nigeria: a need for change. J Sci Innov Res JSIR. 2014;3:251–7.
Oguntola S. Iron tablets, vitamin C affect efficacy of malaria drugs; 2015. http://www.eyesonmalaria.org/content/iron-tablets-vitamin-c-affect-efficacy-malaria-drugs.
Veenemans J, Milligan P, Prentice AM, Schouten LRA, Inja N, van der Heijden AC, et al. Effect of supplementation with zinc and other micronutrients on malaria in Tanzanian children: a randomised trial. PLoS Med. 2011;8:87–8.
Spottiswoode N, Duffy PE, Drakesmith H. Iron, anemia and hepcidin in malaria. Front Pharmacol. 2014;5:1–11.
Nwanyanwu OC, Ziba C, Kazembe PN, Gamadzi G, Gandwe J, Redd SC. The effect of oral iron therapy during treatment for Plasmodium falciparum malaria with sulphadoxine-pyrimethamine on Malawian children under 5 years of age. Ann Trop Med Parasitol. 1996;90(6):589–95.
van den Hombergh J, Dalderop E, Smit Y. Does iron therapy benefit children with severe malaria-associated anaemia? A clinical trial with 12 weeks supplementation of oral iron in young children from the Turiani Division, Tanzania. J Trop Pediatr. 1996;42:220–7.
Cusick SE, Opoka RO, Abrams SA, John CC, Georgieff MK, Mupere E. Delaying iron therapy until 28 days after antimalarial treatment is associated with greater iron incorporation and equivalent hematologic recovery after 56 days in children: a randomized controlled trial. J Nutr. 2016;146:1769–74.
Sharma S, Sharma P, Tyler LN. Transfusion of blood and blood products: indications and complications. Am Fam Physician. 2011;83:719–24.
Authors’ contributions
PNN and GLT designed the protocol and supervised study and; CNN, SMM, GKM, DBN, JLL, LMK and YNL supervised data analysis; DBN and YNL provided statistical support, PNN drafted the manuscript; CHB, ABE, LNY and DBN reviewed the manuscript; All authors read and approved the final manuscript.
Acknowledgements
Funding of this study was provided by the Global fund to fight AIDS, Tuberculosis and Malaria through SANRU. We thank National Malaria Control Programme of DRC (Programme National de Lutte contre le Paludisme) for support and assistance and all the staff of the clinical Pharmacology Unit, especially, Lusakibanza Manzo Mariano, Liwono Yana Jerry, Nanga Mfwawunu Tom, Mbo Modiri Clarisse, the University of Kinshasa and all the Health facilities involved.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was based on the retrospective review of patients’ files. Approval was obtained from the Kinshasa School of Public Health Ethics Committee under the number ESP/CE/100/2013 dated 18 December 2013 before commencement of the study. Authorization was obtained at provincial level and at facility level before data collection. Confidentiality of patients’ information was kept, and the current analysis did not include individual identifiers.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ntamabyaliro, N.Y., Burri, C., Nzolo, D.B. et al. Drug use in the management of uncomplicated malaria in public health facilities in the Democratic Republic of the Congo. Malar J 17, 189 (2018). https://doi.org/10.1186/s12936-018-2332-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-018-2332-3