Abstract
The spread of artemisinin and partner drug resistance through Asia requires changes in first-line therapy. The traditional modus has been the replacement of one first-line anti-malarial regimen with another. The number of anti-malarial drug candidates currently in development may have given false confidence in the expectation that resistance to artemisinin-based combination therapy (ACT) can be solved with a switch to the next anti-malarial drug regimen. A number of promising anti-malarial drug regimens did not succeed in becoming first-line drugs due to safety concerns or rapid development of resistance. Currently promising candidates for inclusion in first-line regimens, such as KAE 609, KAF 156, OZ 439, and OZ 277, have already triggered safety concerns or fears that point mutations could render the drugs inefficacious. An additional challenge for a new first-line drug is finding an appropriate partner drug. There is hope that none of the above-mentioned concerns will be substantiated in larger, upcoming trials. Meanwhile, combining already licensed anti-malarials may be a promising stop-gap measure. Practitioners in Vietnam have empirically started to add mefloquine to the current dihydroartemisinin-piperaquine. Practitioners in Africa could do worse than empirically combine already licensed co-artemether and amodiaquine when treatment with ACT no longer clears Plasmodium falciparum. Both combinations are currently undergoing trials.
Similar content being viewed by others
Background
The spread of artemisinin and partner drug resistance through Asia requires changes in first-line therapy. In Binh Phuoc Province, Vietnam, the proportion of malaria patients with detectable falciparum parasitaemia after three days of treatment with the current first-line treatment, dihydroartemisinin piperaquine, has reached 57% and the parasite clearance half-life doubled from 3.75 h in 2011 to 6.60 h in 2015 [1]. The now dominant artemisinin-resistant Plasmodium falciparum C580Y lineage in the Greater Mekong Sub-region (GMS) probably arose in western Cambodia and spread through Vietnam, Laos and Thailand, outcompeting other parasites and acquiring piperaquine resistance [2]. West of the GMS, P. falciparum strains with two non-synonymous mutations in the k13 propeller region have been detected in Changlang district, Arunachal Pradesh, India. While treatment outcome has not yet been affected in India, the appearance of phenotypic resistance is probably only a question of time. In the past, chloroquine (CQ) and later sulfadoxine/pyrimethamine (SP)-resistant P. falciparum strains spread from India to East Africa and then through the African continent. The recent emergence and spread of multidrug-resistant P. falciparum strains, which are no longer cured by artemisinin-based combination therapy (ACT), has resulted in considerable research, with support from large funders (e.g., Global Fund, Bill and Melinda Gates Foundation, and Wellcome Trust) without any notable impact. When CQ was compromised by resistance, the attributable mortality in sub-Saharan Africa in the 1980–1990s was millions [3]. Yet the spread of ACT resistance has not resulted in the declaration of a Public Health Emergency of International Concern (PHEIC). This omission could be explained by an overreliance on novel anti-malarial drug candidates, which could potentially replace ACT as first-line treatment. This paper discusses potential flaws of such candidate drugs.
Replacement for ACT?
The previous modus of replacing one first-line anti-malarial regimen with another may not be possible now. There is a range of reasons why promising, efficacious anti-malarials in the pipeline did not become first-line treatments. Halofantrine induces consistent dose-related lengthening of the PR and QT intervals, which made it unsuitable for further use in public health [4]. Pyronaridine, in the combination with artemisinin, was considered a highly promising combination therapy until a data monitoring committee found evidence of elevated transaminases in a pivotal trial consistent with low-level toxicity [5]. Further studies suggested that the risk of a hepatotoxicity event was no greater after pyronaridine–artesunate retreatment than after first treatment (0.19 vs 0.54%) yet an aspartate transaminase (AST) increase (3% in first and retreatments) as well as an increased alanine transaminase (ALT; 3% in first and 2% retreatments) with this combination is still higher than in artemether-lumefantrine treatment [6].
The European Medicines Agency has since granted a revised label for the pyronaridine-artesunate combination, removing all restrictions on repeat-dosing, on use only in areas of high resistance and low transmission, and on requirements for liver function monitoring. However the drug’s disappointing efficacy, <90% in Western Cambodia [7], has cast doubt about the usefulness of the pyronaridine–artesunate combination as an universal first-line treatment. Atovaquone was introduced in 1990 and did not become a first-line treatment probably due to its high cost. In addition, atovaquone is particularly susceptible to resistance as single nucleotide polymorphisms can confer high-level resistance. Atovaquone resistance was reported within a year of introduction [8].
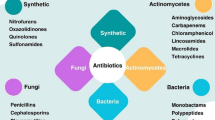
The recent publication of promising trials with several new anti-malarial drug classes has given a reassuring impression that the “anti-malarial drug development pipeline has probably never looked healthier” [9] (see Table 1). Based on the flaws that derailed progress of earlier, promising anti-malarial drugs, there are reasons to be sceptical about the promise of the following candidates in the pipeline:
-
KAE 609, Cipargamin™, (a phase-2 compound), is the most advanced candidate targeting ATPase4. It has the shortest parasite clearance time (PCt ½ < 1 h) observed in any anti-malarial drug [10]. A major concern is single nucleotide polymorphisms (SNP) at the PfATP4 gene which can be selected in vitro after 3–4 months exposure to incrementally increasing sub-lethal concentrations of KAE 609 [11]. If this finding is substantiated, the loss of KAE 609, like atovaquone earlier, seems likely. A second concern about KAE 609 is that administration resulted in abnormal liver function in 3 of 21 [12], alkaline phosphatase increase in 10 of 25, ALT increase in 1 of 25 and hyper-bilirubinaemia in 5 of 25 [13] study participants.
-
KAF 156, an imidazolopiperazine (a phase-2 compound), has a slower PCt rate than KAE 609 but presents similar concerns [12, 14, 15]. Single nucleotide polymorphisms (SNP) in PfCARL, the likely drug target of KAF 156, can be selected in vitro after 4 months exposure to incrementally increasing concentrations of KAF [16]. In addition, 30% of study participants had elevated transaminases.
-
OZ 439, Artefenomel™, (a phase-2 compound), belongs to the ozonides class of drugs, which share peroxide pharmacophore with artemisinins [17, 18]. Like artemisinins, the PCt 1/2 of OZ439 is slower in parasites with k13 mutation suggesting cross-resistance between ozonides and artemisinins [18]. There are safety concerns, as trial participants receiving the drug candidate had elevated creatine phosphokinase (CPK), transaminases and a QTc interval prolongation [18]. A study of 60 volunteers, given a single dose regimen combining 800 mg OZ439 with 960 or 1440 mg piperaquine, is expected to result in lower peak piperaquine plasma concentrations compared with available 3-day piperaquine-artemisinin combinations and can therefore be expected to cause less QTc prolongation [19].
-
OZ 277, Arterolane™, (a phase-4 compound); another synthetic peroxide is the most advanced of the new anti-malarials. Combined with piperaquine, this new drug is already registered and marketed by Ranbaxy in India [20,21,22]. There is a concern that OZ277 shares cross-resistance with the artemisinin derivatives. High resistance levels against the partner drug piperaquine have already been documented in Cambodia and Vietnam. A further concern is the QTc prolongation observed in 6.9% of study participants [23].
It is critical to find and appropriate partner drug for candidate drugs. Ideally the partner drug should facilitate a single dose treatment as SP did in the last century. None of the potential partner drugs can be given as single dose regimen.
Conclusions
There is hope that none of the above-mentioned concerns will be substantiated in larger, upcoming trials. What can be done besides hoping? Attempts to regain efficacy of artemisinins by increasing dose were disappointing [24] and since only fixed-dose combinations are licensed, increased partner drug dosing could be associated with increased toxicity and adherence issues. Extending the course of routine 3-day treatment to 5 or 7 days was successful, associated with a cure rate of 98% in western Cambodia, the epicentre of drug resistance [25]. The cost of such compromised regimens will increase, while adherence could decrease. Practitioners in Vietnam have instead empirically started to add mefloquine to the current DHA-piperaquine first-line treatment. There appears to be an inverse susceptibility between piperaquine and mefloquine. A similar inverse susceptibility between co-artemether (artemether/lumefantrine) and amodiaquine could be exploited as stopgap measure in Africa [26]. Mefloquine did not gain wide acceptance in Africa where co-artemether is the most popular ACT and there has been extensive experience in the use of amodiaquine. Practitioners could do worse than empirically combine co-artemether and amodiaquine until a replacement for the current first-line treatment becomes available. The safety and efficacy of triple therapy is under evaluation in a series of trials in Asia and Africa [27].
How long stop-gap measures can hold back and prevent increasing morbidity and mortality attributable to ACT resistance is unknown. Meanwhile, ACT resistance is spreading across international borders. Large populations in sub-Saharan Africa whose immunity to malaria is declining with decreasing malaria incidence will be severely affected by the spread of ACT resistance. There are no tried and tested approaches to stop the spread of ACT resistance, but recognizing that the spread of ACT resistance is a public health emergency and of international concern is a necessary step to coordinate an international response.
Abbreviations
- ACPR:
-
adequate clinical and parasitological response
- ACT:
-
artemisinin combination therapy
- ALT:
-
alanine transaminase
- AST:
-
aspartate transaminase
- Conc.:
-
concentration
- CPK:
-
creatine phosphokinase
- CQ:
-
chloroquine
- DHA:
-
dihydroartemisinin
- GMS:
-
Greater Mekong Subregion
- K13:
-
PF3D7_1343700 kelch propeller domain
- MIC:
-
minimal inhibitory concentration
- ml:
-
millilitre
- ms:
-
millisecond
- ng:
-
nanogram
- PCR:
-
polymerase chain reaction
- PCt:
-
parasite clearance time
- Pf:
-
Plasmodium falciparum
- PHEIC:
-
Public Health Emergency of International Concern
- RSA:
-
ring-stage survival assay
- SNP:
-
single nucleotide polymorphisms
- SP:
-
sulfadoxine/pyrimethamine
- WT:
-
wild type
References
Thanh NV, Thuy-Nhien N, Tuyen NT, Tong NT, Nha-Ca NT, Dong LT, et al. Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin-piperaquine in the south of Vietnam. Malar J. 2017;16:27.
Imwong M, Suwannasin K, Kunasol C, Sutawong K, Mayxay M, Rekol H, et al. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong Subregion: a molecular epidemiology observational study. Lancet Infect Dis. 2017;17:491–7.
Trape JF. The public health impact of chloroquine resistance in Africa. Am J Trop Med Hyg. 2001;64:12–7.
Nosten F, ter Kuile FO, Luxemburger C, Woodrow C, Kyle DE, Chongsuphajaisiddhi T, et al. Cardiac effects of antimalarial treatment with halofantrine. Lancet. 1993;341:1054–6.
Duparc S, Borghini-Fuhrer I, Craft CJ, Arbe-Barnes S, Miller RM, Shin CS, et al. Safety and efficacy of pyronaridine-artesunate in uncomplicated acute malaria: an integrated analysis of individual patient data from six randomized clinical trials. Malar J. 2013;12:70.
Sagara I, Beavogui AH, Zongo I, Soulama I, Borghini-Fuhrer I, Fofana B, et al. Safety and efficacy of re-treatments with pyronaridine-artesunate in African patients with malaria: a substudy of the WANECAM randomised trial. Lancet Infect Dis. 2016;16:189–98.
Leang R, Canavati SE, Khim N, Vestergaard LS, Fuhrer IB, Kim S, et al. Efficacy and safety of pyronaridine-artesunate for treatment of uncomplicated Plasmodium falciparum malaria in western Cambodia. Antimicrob Agents Chemother. 2016;60:3884–90.
Looareesuwan S, Viravan C, Webster HK, Kyle DE, Hutchinson DB, Canfield CJ. Clinical studies of atovaquone, alone or in combination with other antimalarial drugs, for treatment of acute uncomplicated malaria in Thailand. Am J Trop Med Hyg. 1996;54:62–6.
White NJ. Can new treatment developments combat resistance in malaria? Expert Opin Pharmacother. 2016;17:1303–7.
White NJ, Pukrittayakamee S, Phyo AP, Rueangweerayut R, Nosten F, Jittamala P, et al. Spiroindolone KAE609 for falciparum and vivax malaria. N Engl J Med. 2014;371:403–10.
Rottmann M, McNamara C, Yeung BKS, Lee MCS, Zou B, Russell B, et al. Spiroindolones, a potent compound class for the treatment of malaria. Science. 2010;329:1175–80.
White N, Thanh DT, Uthaisil C, Nosten F, Phyo AP, Hanboonkunupakarn B, et al. Antimalarial activity of KAF156 in falciparum and vivax malaria. N Engl J Med. 2016;375:1152–60.
Tran HT, White NJ, Nguyen T-NT, Nhu HT, Phung TD, Tarning J, et al. Estimation of the in vivo minimum inhibitory concentration of cipargamin in uncomplicated Plasmodium falciparum malaria. Antimicrob Agents Chemother. 2016:AAC. Abstract 01940-16.
Kuhen KL, Chatterjee AK, Rottmann M, Gagaring K, Borboa R, Buenviaje J, et al. KAF156 is an antimalarial clinical candidate with potential for use in prophylaxis, treatment, and prevention of disease transmission. Antimicrob Agents Chemother. 2014;58:5060–7.
Leong FJ, Zhao R, Zeng S, Magnusson B, Diagana TT, Pertel P. A first-in-human randomized, double-blind, placebo-controlled, single- and multiple-ascending oral dose study of novel Imidazolopiperazine KAF156 to assess its safety, tolerability, and pharmacokinetics in healthy adult volunteers. Antimicrob Agents Chemother. 2014;58:6437–43.
Magistrado PA, Corey VC, Lukens AK, LaMonte G, Sasaki E, Meister S, et al. Plasmodium falciparum cyclic amine resistance locus (PfCARL), a resistance mechanism for two distinct compound classes. ACS Infect Dis. 2016;2:816–26.
McCarthy JS, Baker M, O’Rourke P, Marquart L, Griffin P, Hooft van Huijsduijnen R, et al. Efficacy of OZ439 (artefenomel) against early Plasmodium falciparum blood-stage malaria infection in healthy volunteers. J Antimicrob Chemother. 2016;71:2620–7.
Phyo AP, Jittamala P, Nosten FH, Pukrittayakamee S, Imwong M, White NJ, et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. Lancet Infect Dis. 2016;16:61–9.
Darpo B, Ferber G, Siegl P, Laurijssens B, Macintyre F, Toovey S, et al. Evaluation of the QT effect of a combination of piperaquine and a novel anti-malarial drug candidate OZ439, for the treatment of uncomplicated malaria. Br J Clin Pharmacol. 2015;80:706–15.
Uhlemann AC, Wittlin S, Matile H, Bustamante LY, Krishna S. Mechanism of antimalarial action of the synthetic trioxolane RBX11160 (OZ277). Antimicrob Agents Chemother. 2007;51:667–72.
Patil C, Katare S, Baig M, Doifode S. Fixed dose combination of arterolane and piperaquine: a newer prospect in antimalarial therapy. Ann Med Health Sci Res. 2014;4:466–71.
Saha N, Moehrle JJ, Zutshi A, Sharma P, Kaur P, Iyer SS. Safety, tolerability and pharmacokinetic profile of single and multiple oral doses of arterolane (RBx11160) maleate in healthy subjects. J Clin Pharmacol. 2014;54:386–93.
Valecha N, Krudsood S, Tangpukdee N, Mohanty S, Sharma SK, Tyagi PK, et al. Arterolane maleate plus piperaquine phosphate for treatment of uncomplicated Plasmodium falciparum malaria: a comparative, multicenter, randomized clinical trial. Clin Infect Dis. 2012;55:663–71.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Taylor AR, Flegg JA, Holmes CC, Guerin PJ, Sibley CH, Conrad MD, et al. Artemether-lumefantrine and dihydroartemisinin-piperaquine exert inverse selective pressure on Plasmodium falciparum drug sensitivity-associated haplotypes in Uganda. Open Forum Infect Dis. 2017;4:229.
ClinicalTrials.gov. A study by the tracking resistance to artemisinin collaboration (TRAC) (TRACII). ClinicalTrialsgov Identifier: NCT02453308 2015.
Authors’ contributions
Both authors read and approved the final manuscript.
Acknowledgements
We thank our colleagues at the Shoklo Malaria Research Unit and the Mahidol Oxford Research Unit for inspritation and support.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Phyo, A.P., von Seidlein, L. Challenges to replace ACT as first-line drug. Malar J 16, 296 (2017). https://doi.org/10.1186/s12936-017-1942-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-017-1942-5