Abstract
Background
Pyronaridine-artesunate (PA) is indicated for the treatment of acute uncomplicated Plasmodium falciparum and Plasmodium vivax malaria.
Methods
Individual patient data on safety outcomes were integrated from six randomized clinical trials conducted in Africa and Asia in patients with microscopically confirmed P. falciparum (five studies) or P. vivax (one study) malaria. Efficacy against P. falciparum was evaluated across three Phase III clinical trials.
Results
The safety population included 2,815 patients randomized to PA, 1,254 to comparators: mefloquine + artesunate (MQ + AS), artemether-lumefantrine (AL), or chloroquine. All treatments were generally well tolerated. Adverse events occurred in 57.2% (1,611/2,815) of patients with PA versus 51.5% (646/1,254) for comparators, most commonly (PA; comparators): headache (10.6%; 9.9%), cough (5.9%; 5.6%) and anaemia (4.5%; 2.9%). Serious averse events were uncommon for all treatments (0–0.7%). Transient increases in alanine aminotransferase and aspartate aminotransferase were observed with PA but did not lead to any clinical sequelae. For P. falciparum malaria, day-28 PCR-corrected adequate clinical and parasitological response with PA was 93.6% ([1,921/2,052] 95% CI 92.6, 94.7) in the intent-to-treat population and 98.5% ([1,852/1,880] 95% CI 98.0, 99.1) in the per-protocol population. Median parasite clearance time was 24.1 h with PA, 31.9 h with MQ + AS, and 24.0 h with AL. Median fever clearance time was 15.5 h with PA, 15.8 h with MQ + AS, and 14.0 h with AL. By day 42, P. falciparum gametocytes had declined to near zero for all treatments.
Conclusions
Pyronaridine-artesunate was well tolerated with no safety concerns with the exception of mostly mild transient rises in transaminases. Efficacy was high and met the requirements for use as first-line therapy. Pyronaridine-artesunate should be considered for inclusion in malaria treatment programmes.
Trial registration
Clinicaltrials.gov: NCT00331136; NCT00403260; NCT00422084; NCT00440999; NCT00541385; NCT01594931
Similar content being viewed by others
Background
More than three billion people are at risk of malaria[1]. Despite recent progress in malaria control, there were around 216 million episodes of clinical infection in 2010[1]. Most malaria deaths, around 655,000 each year, occur from Plasmodium falciparum infection in children under five years of age[1, 2]. However, the important contribution of Plasmodium vivax infection to global malaria morbidity is now also being recognized[3–6].
For P. falciparum malaria, artemisinin-based combination therapy (ACT) is generally recommended by the World Heath Organization (WHO)[7]. Parasite burden and fever are rapidly reduced with ACT and efficacy remains high in most regions[7]. Artemisinin tolerance – observed as extended parasite clearance times with ACT treatment – has emerged among P. falciparum from the Cambodia–Thailand border areas[8–15], with some evidence of resistance spreading at the Thailand–Myanmar border[16]. For P. vivax, the WHO recommends ACT in areas where chloroquine resistance has emerged[7]; most notably Indonesia, though there are also reports from further east in the Malay archipelago to Papua New Guinea and Vietnam as well as from South America and Oceania[17, 18]. Using ACT in areas co-endemic for P. falciparum and P. vivax has also been suggested as a strategy to overcome difficulties in differential diagnosis and in cases of mixed infection[17, 19, 20].
Pyronaridine-artesunate (PA) (3:1 ratio) is a novel ACT indicated for the treatment of acute uncomplicated P. falciparum or P. vivax malaria[15, 21–25]. In vitro studies indicate potent activity against recent isolates of multidrug-resistant strains of both P. falciparum and P. vivax from Papua, Indonesia[26], against Kenyan P. falciparum isolates[27], and against around half of chloroquine-resistant P. falciparum strains from the China–Myanmar border area[28]. The PA clinical development programme included two Phase II trials and three Phase III trials in children and adults from Africa and Asia with uncomplicated P. falciparum malaria[15, 22, 24, 25], as well as one comparative Phase III trial in children and adults with uncomplicated P. vivax infection[23]. The programme incorporated parallel development of an adult tablet and a paediatric granule formulation[22], shown in a Phase II study to display similar bioavailability[24]. In all four Phase III studies, PA efficacy was non-inferior to the comparator anti-malarial drugs and PA was generally well tolerated[15, 22, 23, 25].
The objective of this paper was to evaluate PA safety outcomes by integrating individual patient data from two Phase II and four Phase III randomized clinical trials[15, 22–25]. Efficacy outcomes for PA in uncomplicated P. falciparum malaria were examined descriptively across the three Phase III trials that included patients with this infection[15, 22, 25].
Methods
Ethics statement
The clinical trials were conducted in accordance with the Declaration of Helsinki (Tokyo 2004), Good Clinical Practice and applicable regulations. Trial protocols were approved by the independent ethics committee of each study centre. All patients or their guardians provided informed written or witnessed oral consent; assent was required from children able to understand the study.
Source data
Individual patient data were integrated from six PA randomized clinical trials, two Phase II studies and four Phase III studies, conducted in sub-Saharan Africa, Southeast Asia and India between 2005 and 2008 (Table 1)[15, 22–25]. Further details of the trial protocols are supplied in the published reports[15, 22–25].
Details of the studies included in this analysis are summarized in Table 1. The two Phase II studies were non-comparative; one was a dose escalation study to examine the safety and pharmacokinetics of the PA tablet and granule formulations in children with P. falciparum (SP-C-003-05)[24], the other was a dose ranging study (SP-C-002-05) of PA tablets in adults with P. falciparum malaria. Of the four Phase III studies, three were conducted in subjects with P. falciparum[15, 22, 25], two studies used PA tablets[15, 25], and one the PA granule formulation[22]. The remaining Phase III study included subjects with P. vivax malaria[23]. All four Phase III studies were non-inferiority studies against comparators recommended as first-line anti-malarial therapy in the relevant countries. The non-inferiority margin was 5% in the two P. falciparum tablet studies that included both children and adults (SP-C-004-06, SP-C-005-06), and 10% in the paediatric granule P. falciparum study (SP-C-007-07) and the P. vivax study (SP-C-006-06).
Treatments
Pyronaridine-artesunate (Shin Poong Pharmaceutical Company Ltd, Ansan, South Korea) was supplied as tablets (180:60 mg per tablet) or as a paediatric granule formulation presented in sachets (60:20 mg per sachet). In the Phase III studies, PA was given once daily for three days (day 0, 1, 2), dosed by body weight as follows, for tablets: 20–25 kg one tablet, 26–44 kg two tablets, 45–64 kg three tablets, 65–90 kg four tablets, i e, 7.2:2.4 to 13.8:4.6 mg/kg/dose; and for granules, ≥5– <9 kg one sachet, 9– <17 kg two sachets, 17– <25 kg three sachets, i e, 6.7:2.2 to 13.3:4.4 mg/kg/dose.
The comparators in the PA Phase III P. falciparum studies were dosed by body weight. Artemether-lumefantrine (AL) was given twice daily for three days, at 0.9:5.3 to 2.4:14.4 mg/kg/dose for tablets in SP-C-005-06 and 1.3:8.0 to 4.0:24.0 mg/kg/dose for crushed tablets in SP-C-007-07. Dosing of AL was with or without food based on local practices. Mefloquine + artesunate (MQ + AS) was given as a loose combination, once daily for three days at 5.6:2.2 to 12.5:5.0 mg/kg/dose in study SP-C-004-06. In the Phase III P. vivax study (SP-C-006-06), the comparator chloroquine (CQ) was given once daily for three days at a daily dose in children of 10 mg/kg on days 0 and 1 and 5 mg/kg on day 2 and for adults of 620 mg on days 0 and 1 and 310 mg on day 2.
Patients and procedures
Patients and procedures are described in detail elsewhere[15, 22–25]. In brief, patients of either gender were eligible if they had P. falciparum mono-infection, or in SP-C-006-06 P. vivax mono-infection, in all cases microscopically confirmed within defined limits (Table 1), with fever or a history of fever while meeting age/body weight criteria for each study (Table 1). Patients were excluded if they had significant co-morbid illness, recent anti-malarial therapy, known hypersensitivity to study drugs, evidence of severe malnutrition, if they were pregnant (test required) or breastfeeding, or had participated previously in a PA clinical trial.
At screening, a medical history was taken and a physical examination performed. All enrolled patients were hospitalized from day 0 to 3. Follow-up assessments were at days 7, 14, 21, 28, 35 and 42. Vital signs and malaria signs/symptoms were monitored throughout the study. Temperature was taken at screening, every 8 h over ≥72 h following the first dose or until two normal readings between 7 and 25 h apart, then at each visit or as clinically indicated. Venous blood samples were taken for clinical biochemistry, haematology and urinalysis testing and 12-lead electrocardiographs were performed at screening and then at intervals as specified in the protocol.
Parasitological assessments were performed according to WHO guidelines[29]. Giemsa-stained thick blood slides were prepared before each dose, every 8 h (±1 h) following first dose administration for ≥72 h or until parasite clearance (two consecutive negative readings 7 to 25 h apart), and at subsequent visits. For P. falciparum, asexual and gametocyte parasite counts were performed separately; for P. vivax asexual and gametocyte parasite counts were recorded separately at screening and total parasite counts recorded at all other assessments. Thin blood slides were prepared for parasite identification at screening and from day 7 at all follow-up visits. In the P. falciparum Phase III studies, recrudescence was determined by PCR genotyping using P. falciparum genes msp 1, msp 2, and glurp; defined as at least one matching allelic band in all markers between baseline and post-day-7 samples[30, 31].
Outcomes
Safety outcomes were adverse event incidence and severity (categorized using MedDRA version 10.1), laboratory abnormalities (graded according to the Division of Microbiology and Infectious Diseases Toxicity Scale), and electrocardiograph abnormalities.
Efficacy outcomes were integrated for the Phase III P. falciparum studies only and were defined according to WHO methods[29]. The primary efficacy outcome was day-28 PCR-corrected adequate clinical and parasitological response (ACPR), defined as clearance of asexual parasitaemia without recrudescence or previous treatment failure. Day-28 uncorrected ACPR was a secondary endpoint.
Secondary efficacy endpoints were parasite clearance time (time from first dose to asexual aparasitaemia for two consecutive negative readings 7–25 h apart); fever clearance time (time from first dose to apyrexia for two consecutive normal temperature readings 7–25 h apart); and the proportion of subjects aparasitic and proportion apyretic at day 1 (24 h after the first dose), day 2 (48 h after the first dose), and day 3 (72 h after the first dose). The proportion of patients with gametocytes at each assessment was an exploratory endpoint.
Statistical methods
The safety analysis included data from all Phase II and Phase III studies and was conducted on the safety population, i e, all patients who had received any amount of study drug. Descriptive statistics were provided for safety outcomes.
The efficacy analysis included data from the Phase III P. falciparum trials and in the integrated analysis was conducted primarily on the intent-to-treat (ITT) population, i e, all randomized patients with P. falciparum malaria who received any amount of study medication. This definition was consistent across all the Phase III P. falciparum studies. Descriptive statistics were provided for efficacy outcomes.
Descriptive sub-group analyses were performed for day-28 PCR-corrected ACPR for the ITT population as follows: region (Asia, Africa); age (<5, 5–12, >12– <18, ≥18 years); gender (male, female); weight (<17, ≥17– <25, ≥25 kg); previous malaria episode (yes, no); number of previous malaria episodes in the last 12 months (0, 1, >1); baseline parasitaemia (≤5,000, >5,000–10,000, >10,000 μL-1); PA formulation (granule, tablet); and PA actual dose (≤8.5:2.8, >8.5:2.8–9.5:3.2, >9.5:3.2–11.0:3.7, >11.0:3.7 mg/kg/day).
Post-hoc analyses of time to recrudescence and time to re-infection conducted using Kaplan-Meier estimates (log-rank test) were conducted for the integrated analysis; subjects without the event were censored at the last available parasite assessment date.
Kaplan-Meier estimates were used to evaluate parasite clearance time and fever clearance time. Subjects without parasite or fever clearance within 72 h after the first treatment dose were censored at that time point. An additional analysis of parasite clearance time in Cambodia (Pailin at the Cambodia–Thailand border) versus Thailand (Mae Sot and Mae Ramat) was performed without censoring at 72 h. The proportion of subjects with parasite clearance and the proportion of subjects with fever clearance on days 1, 2 and 3 were calculated using Kaplan-Meier estimates. Log10 area under the curve (AUC) for gametocyte density was calculated in count · day/μL based on a log10 transformation. Statistical analysis was performed using SAS (Version 9.1).
Results
Patients
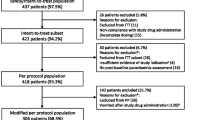
Overall, 2,817 patients were randomized to PA and 1,254 to comparators (MQ + AS, AL and CQ). Two subjects did not receive PA and were excluded from the safety population (n = 2,815) (Table 2). A similar proportion of patients in the PA group (14.4% [405/2,815]) discontinued treatment as for comparators (17.6% [221/1,254]). In the efficacy (ITT) population, 2,052 subjects with P. falciparum malaria were treated with PA and 1,026 with comparators (MQ + AS or AL) (Table 2). Subject disposition for the efficacy ITT population was similar to that of the safety population (Table 2).
In the PA group (safety population), 91.9% (2,587/2,815) of patients were treated for P. falciparum and 8.1% (228/2,815) for P. vivax malaria, 49.3% (1,389/2,815) of subjects were from Asia, 50.7% (1,426/2,815) from Africa and mean patient age was 20.6 years (Table 3). Overall in the safety population, the PA group and the combined comparators group were well balanced for baseline demographic and clinical characteristics (Table 3). However, for individual comparators, integration of the data led to imbalances in patient age and the regions from which patients were recruited because of the different study entry criteria (Table 3).
Safety
In the safety population, medication was taken as planned for 98.9% (2,785/2,815) of patients receiving PA and 98.6% (1,236/1,254) of those receiving comparators. All drug treatments were generally well tolerated. The number of patients with at least one treatment-emergent adverse event was similar for PA (57.2% [1,611/2,815]) and comparators (51.5% [646/1,254]), as was the number of patients thought to have adverse events related to drug therapy: 25.2% (708/2,815) and 25.5% (320/1,254), respectively. The nature and incidence of adverse events due to any cause was similar for PA versus combined comparators (Table 4). The most common adverse events were headache (10.6% PA; 9.9% comparators), cough (5.9% PA; 5.6% comparators) and anaemia (4.5% PA; 2.9% comparators) (Table 4).
Serious adverse events occurred in 0.6% (18/2,815) of patients in the PA group and in 0.4% (5/1,254) in the combined comparators. There were no deaths. One patient in the PA group had two serious adverse events that were considered treatment-related (hepatic enzyme increased and abortion incomplete) and one patient receiving MQ + AS had two treatment-related serious adverse events (convulsion and grand mal convulsion). All other serious adverse events were considered not to be related to treatment: in the PA group there were two cases each of pyrexia, malaria, typhoid fever and urinary tract infection, and one case each of anaemia, cardiac failure, abdominal pain, limb abscess, cholera, paronychia, parotitis, pneumonia, acute pyelonephritis, wound infection, abortion complete and depression; for comparators there were two cases of cerebral malaria and one of immunosuppression.
Overall, adverse events leading to study withdrawal occurred in 1.6% (44/2,815) of patients in the PA group and 1.0% (13/1,254) in the comparator group; vomiting was the reason in 1.1% (32/2,815) and 0.9% (11/1,254) of cases, respectively. In the PA group, other reasons for study withdrawal were P. falciparum infection (0.3%; 9/2,815), malaria (0.1%; 3/2,815) and one case each of nausea and fatigue. In the comparator group there were two cases of cerebral malaria (0.2%) leading to study withdrawal. Of the patients who were withdrawn from the study because of an adverse event, drug treatment was discontinued in 2.2% (27/1,254) of patients in the PA group (26 instances of vomiting, one of nausea, one of malaria) and in 1.0% (12/1,254) of patients receiving comparators (10 vomiting, two cerebral malaria).
There were no major differences between PA and comparators in haematology parameters over the course of the study (Figure 1). For all treatment groups, there was a small decrease in haemoglobin concentration on day 3 (mean <1 g/dL) with recovery to baseline levels by day 28, and corresponding changes in haematocrit and red blood cells. Proportional decreases in neutrophils from baseline were associated with mean proportional increases in lymphocytes and eosinophils. Platelet counts were low at baseline and had increased by day 7 in all treatment groups. There were no clinically meaningful changes from baseline for white blood cells, monocytes or basophils in any treatment group.
Changes from baseline in haematology parameters in patients receiving pyronaridine-artesunate or combined comparators (safety population). NB: Day-28 values are available for the Plasmodium vivax study only[23].
No clinically important changes from baseline were observed in total bilirubin, alkaline phosphatase, creatinine, albumin, creatine kinase, urea, sodium, potassium, glucose or blood urea nitrogen in any treatment group. In the PA group, both alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were increased on day 3 and day 7 versus baseline, and normalized by day 28 (Figure 2). In the PA group, treatment-emergent Grade 3/4 toxicities for ALT were recorded for 0.4% (11/2,750) of patients on day 3 and 0.9% (24/2,709) on day 7; for AST the incidence was 0.5% (13/2,757) and 0.3% (9/2,711), respectively. For comparators, in the MQ + AS group 0.2% (1/404) of patients had an ALT Grade 3 toxicity on day 7. In the AL group, 0.2% (1/582) of patients had an ALT Grade 4 toxicity on day 3, and for AST 0.5% (3/583) had Grade 3 toxicity on day 3 and 0.2% (1/581) on day 7. Only one patient in the PA group had a serious adverse event related to a Grade 3/4 biochemistry value, hepatic enzyme increased: Grade 3 AST and ALT values on day 7 (295 U/L and 272 U/L, respectively), decreasing to near normal levels by day 28 (54 U/L, 25 U/L, respectively); total bilirubin was normal at all assessments; ALP was normal except for a Grade 1 toxicity on day 7 (168 U/L). The proportion of patients with ALT and/or AST >3x the upper limit of normal (ULN) plus peak total bilirubin >2xULN in the PA group was 0.2% (7/2,815) versus 0.3% (2/603) for AL; one of these patients receiving PA also had a clinically important increase in ALP. There were no cases in the MQ + AS or CQ groups. No clinically important changes were recorded for urine glucose, protein and blood screening.
Changes from baseline in liver enzymes and total bilirubin in patients receiving pyronaridine-artesunate or combined comparators (safety population). NB: Day-28 values are available for the Plasmodium vivax study only[23].
The incidence of treatment-emergent clinically important abnormal electrocardiograph results was 1.1% (30/2,752) for PA, 0.7% (3/417) for MQ + AS, 0.3% (2/588) for AL and 2.7% (6/222) for CQ. An adverse event of QT interval prolongation was recorded for 0.2% (6/2,815) of patients receiving PA, 1.2% (5/423) receiving MQ + AS, 0.2% (1/603) receiving AL and 2.6% (6/228) receiving CQ. The proportion of patients with an adverse event of bradycardia was 1.1% (31/2,815) for PA and 0.8% (5/603) for AL with no cases in the MQ + AS or CQ groups. No electrocardiograph abnormality required drug discontinuation or withdrawal from the study.
Efficacy
Efficacy was evaluated in an integrated analysis of the Phase III P. falciparum studies SP-C-004-06[15] SP-C-005-06[25] and SP-C-007-07[22]. Day-28 PCR-corrected ACPR for PA was 93.6% ([1,921/2,052] 95% CI 92.6, 94.7) in the ITT population and 98.5% ([1,852/1,880] 95% CI 98.0, 99.1) in the PP population; similar to comparators (Figure 3A). For day-28 uncorrected ACPR, there was no difference between PA and comparators in the ITT or PP populations (Figure 3B).
Sub-group analysis provided similar day-28 PCR-corrected ACPR rates (ITT population) regardless of region, age group, gender, weight, previous malaria, number of episodes of malaria in the last 12 months, or baseline parasitaemia (Table 5). There was no difference in day-28 PCR-corrected ACPR (ITT population) between the PA granule and tablet formulations: 93.8% ([333/355] 95% CI 91.3, 96.3) and 93.6% ([1,588/1,697] 95% CI 92.4, 94.7), respectively. Efficacy was similar across the actual PA dose groups: 92.2% ([365/396] 95% CI 89.5, 94.8) for ≤8.5:2.8 mg/kg/day; 93.9% ([512/545] 95% CI 91.9, 96.0) for >8.5:2.8–9.5:3.2 mg/kg/day; 94.0% ([616/655] 95% CI 92.2, 95.9) for >9.5:3.2–11.0:3.7 mg/kg/day; and 93.9% ([428/456] 95% CI 91.6, 96.1) for >11.0:3.7 mg/kg/day.
Kaplan-Meier estimates of P. falciparum recrudescence rate and re-infection rate are shown in Figure 4. Both the recrudescence rate (Figure 4A) and the re-infection rate (Figure 4B) with PA were intermediate between MQ + AS and AL.
The majority of patients in all treatment groups had P. falciparum clearance by day 2 (Table 6). Median parasite clearance time for P. falciparum (ITT population) was 24.1 h with PA, 31.9 h with MQ + AS, and 24.0 h with AL (Table 6; Figure 5A). Median parasite clearance time was extended for all treatments in Asian versus African centres (Table 6). In particular, median parasite clearance time was extended in Cambodia for both treatment groups at 64.1 h for PA and 64.2 h for MQ + AS (Figure 5B). In comparison, median parasite clearance time in Thailand was 31.7 h for PA and 38.7 h for MQ + AS (Figure 5B). Day-28 PCR-corrected ACPR (ITT population) in the PA group in Cambodia was 89.3% (125/140) 95% CI 82.9, 93.9 and in Thailand was 93.3% (375/402) 95% CI 90.4, 95.5. For MQ + AS group, day-28 PCR-corrected ACPR (ITT population) was 93.0% (66/71) 95% CI 84.3, 97.7 in Cambodia and 88.9% (176/198) 95% CI 83.7, 92.9 in Thailand.
The majority of patients with P. falciparum had fever clearance by day 1 (Table 6). Median fever clearance time for P. falciparum in the ITT population was 15.5 h for PA, 15.8 h for MQ + AS and 14.0 h with AL (Table 6, Figure 6). Fever clearance times were extended in Asia versus Africa for all treatments (Table 6).
Plasmodium falciparum gametocytes were present in 8.9% (276/3,078) of patients at baseline, and gradually decreased to 0% or near 0% in all treatment groups by the end of the study (Figure 7).
To further investigate P. falciparum gametocyte carriage, data for the two studies that recruited both adults and children (SP-C-004-06 and SP-C-005-06) were reanalysed to calculate the log10 AUC for gametocyte density (Figure 8). In study SP-C-004-06, in patients who had gametocytes at baseline, median log10 [AUC gametocyte density] was 3.1 (range 0.1 to 4.4) in the PA group (n = 81) and 2.5 (range −0.2 to 4.2) in the MQ + AS group (n = 49) (Figure 8A). In study SP-C-005-06, in patients who had gametocytes at baseline, median log10 [AUC gametocyte density] was 2.5 (range −0.8 to 4.8) in the PA group (n = 66) and 2.1 (−0.3 to 3.6) in the AL group (n = 22) (Figure 8C). In patients with no gametocytes at baseline, but who had post-baseline gametocytes, in study SP-C-004-06, median log10 [AUC gametocyte density] was 2.1 (range 0.43 to 3.65) in the PA group (n = 64) and 1.4 (range 0.22 to 3.4) in the MQ + AS group (n = 17) (Figure 8B). In study SP-C-005-06, median log10 [AUC gametocyte density] was 0.9 (range −0.5 to 3.0) in the PA group (n = 67) and 0.5 (−0.5 to 3.2) in the AL group (n = 25) (Figure 8D).
Plasmodium falciparum gametocyte density over time. A) Study SP-C-004-06 comparing pyronaridine-artesunate to mefloquine + artesunate gametocyte density over time in patients with baseline gametocytes and B) no gametocytes at baseline and post-baseline gametocytes. C) Study SP-C-005-06 comparing pyronaridine-artesunate to artemether-lumefantrine gametocyte density over time in patients with baseline gametocytes and D) no gametocytes at baseline and post-baseline gametocytes. All data are for the intent-to-treat population.
Discussion
The integrated safety analysis included 2,815 adults and children treated with PA for uncomplicated P. falciparum or P. vivax infection. The PA group was well balanced for baseline clinical and demographic characteristics with respect to the combined comparator group. The safety profile for PA in this analysis was similar to that reported for pyronaridine and artemisinin monotherapy[21, 32–35]. Comparator safety profiles were also consistent with previous reports for MQ + AS[36–42], AL[25, 43–46] and CQ[23, 47, 48].
Overall, PA and comparators were generally well tolerated. Although the nature and incidence of adverse events were generally similar between PA and comparators overall, dizziness was more common with MQ + AS (6.6%) and myalgia with CQ (9.2%) than with PA (1.4% and 3.8%, respectively) (Table 4). Serious adverse events were uncommon in all treatment groups (0–0.7%). For PA, only one patient had serious adverse events thought to be related to drug treatment; hepatic enzymes increased and incomplete abortion.
The only significant laboratory finding in the PA group was a mean increase in ALT and AST on days 3 and 7, compared with decreases in these enzymes for comparators (Figure 2). As a result of this signal, an Independent Data Monitoring Committee (IDMC) comprising six members, including three experts in hepatotoxicity, examined the data from all of the studies. Increased transaminases have been observed consistently across all the Phase II/III PA clinical studies and two (of four) of the completed Phase I studies. When they occurred, rises in transaminases peaked by day 7 and levels had normalized or were decreasing by day 28 with no instances of Grade 3 or 4 toxicity at this time point. Increased transaminases were associated rarely with rises in total bilirubin, which was often high at baseline and subsequently fell during treatment. Overall, 0.2% (7/2,815) of patients in the PA group and 0.3% (2/603) in the AL group had ALT and/or AST >3x the upper limit of normal (ULN) plus peak total bilirubin >2xULN; one of these patients in the PA group had elevated ALP which precluded them as a Hy’s law case. Importantly, no patients had any clinical sequelae related to these liver function changes and as a result the IDMC concluded that whilst PA treatment is associated with transient elevated transaminases, the early onset (day 3–7) and rapid resolution are consistent with a direct low-level toxicity. Therefore, as PA is dosed for only three days, the risk of progressive liver injury is small. Additional studies are ongoing in healthy volunteers and in patients to assess the hepatic safety profile of PA when the treatment is administered more than once.
Electrocardiograph results did not suggest any cardiac safety concerns with PA. As would be expected, prolonged QT interval was uncommon with PA (0.07%) but occurred more frequently with the quinoline derivatives MQ (0.7%) and particularly CQ (2.7%)[49]. Bradycardia was observed as an adverse event in 1.1% of patients receiving PA and 0.8% with AL. However, the finding of bradycardia in a young and otherwise fit population is likely to be associated with the resolution of the tachycardia associated with fever as decreases in mean heart rate were noted across all treatment groups and have been observed in other studies of anti-malarial therapy as patients become afebrile and they return to their normal baseline heart rate[33, 50–52].
For the treatment of uncomplicated P. falciparum in children and adults, there was no difference between PA and comparators for day-28 PCR-corrected ACPR for the ITT or PP analyses (Figure 3). This reflects results from the three P. falciparum Phase III studies in which non-inferiority of PA day 28 PCR-corrected ACPR (PP population) was demonstrated versus MQ + AS or AL[15, 22, 25]. Sub-group analysis showed similar day-28 PCR-corrected ACPR (ITT population) for PA by region, age group, gender, weight, previous malaria, malaria in the last 12 months, and baseline parasitemia versus efficacy with PA overall (Table 5).
Kaplan-Meier analysis of the integrated efficacy analysis indicated a P. falciparum recrudescence rate for PA intermediate between the comparators (Figure 4A). For individual studies, recrudescence rate over the 42-day study period was marginally higher with PA versus MQ + AS (P = .049) in SP-C-004-06 and similar versus AL (P = .90) in SP-C-005-06 and in the paediatric study SP-C-007-07 (P = .53)[15, 22, 25]. Similarly, Kaplan-Meier analysis of the integrated efficacy analysis indicated a P. falciparum re-infection rate for PA intermediate between the comparators (AL highest, MQ + AS lowest) (Figure 4B). However, in the individual Phase III studies, re-infection rate was higher with MQ + AS than PA at day 28 (P = .04), and similar at day 42 (P = .17)[15]. One difference in the integrated analysis was that there were more patients in the PA group who where under 18 years of age than in the MQ + AS group and this may have increased the re-infection rate for PA relative to MQ + AS. In support of this, in the Phase III study of PA versus AL that comprised mostly adults (SP-C-005-06), PA had a lower re-infection rate than AL (day 28 P = .004, day 42 P = .007)[25], but this difference was not evident in the paediatric PA versus AL study (SP-C-007-07) (P = .77)[22]. In the integrated analysis, re-infection rate was lower with PA than AL and the patients in the AL group tended to be younger. An alternative explanation is that there were differences in transmission rates between the treatment groups given the imbalance in Asian versus African centres in the integrated analysis.
In the integrated analysis, the P. falciparum parasite clearance rate was 24.1 h with PA and 32.9 h with MQ + AS (Figure 5A, Table 6). However, this was not seen in the comparative Phase III trial of these treatments in which median parasite clearance time was approximately 32 h in both arms (P = .08)[15]. This is probably because of the greater proportion of patients from Africa in the PA group versus the MQ + AS group in the integrated analysis; median parasite clearance rates were longer in Asia than Africa for all comparators (Table 6). In particular, in Cambodia parasite clearance times were extended for PA and MQ + AS to around 64 h (Figure 5B). However, this did not seem to affect the day-28 PCR-corrected ACPR (ITT population) between Cambodia and Thailand for either PA or MQ + AS. Extended parasite clearance times indicate the presence of artemisinin resistance and the results presented here are consistent with other reports from the Cambodia–Thailand border area[8–14, 53]. For example, mean parasite clearance times of around 65 h have been reported for artemisinin-piperaquine, dihydroartemisinin-piperaquine and AL in this region[13].
Parasite clearance times were similar between PA and AL in the integrated analysis (Figure 5A). However, in the individual studies of PA versus AL, parasite clearance was faster with PA (P = .02) in study SP-C-007-07 conducted in children, and in study SP-C-005-06 including mostly adults (P < .001)[22, 25]. As above, these differences are probably explained by the longer parasite clearance times in Asian versus African centres, there being a relative lack of patients recruited from Asian centres in the AL group compared with the PA group in the integrated analysis.
Fever clearance time for PA in the integrated analysis was approximately intermediate between AL (fastest) MQ + AS (slowest) (Figure 6). However, in the individual Phase III studies, fever clearance times were shorter with PA versus AL in the paediatric study (P = .049) and there was no difference in the study conducted versus AL mostly in adults (P = .55)[22, 25]. This again probably reflects the greater proportion of patients recruited from Asian centres in the PA and MQ + AS groups versus the AL group in the integrated analysis.
In the integrated analysis, it appeared that AL more rapidly eradicated gametocytes versus PA and MQ + AS (Figure 7). However, this is also probably explained by the difference in baseline populations. To investigate further, gametocytes carriage was analysed in the two studies that enrolled both adults and children[15, 25], using log10 AUC [gametocyte density][54, 55]. In patients with baseline gametocytes, MQ + AS did appear to more rapidly reduce gametocyte carriage versus PA, though in patients with no gametocytes at baseline PA appeared to more effectively suppress gametocyte emergence (Figure 8). There appeared to be no differences between AL and PA in respect to gametocyte clearance or suppression.
Children are the most important target group for anti-malarial therapy, having reduced immunity and consequently poorer outcomes. Despite this, until recently paediatric ACT formulations have been generally lacking[56]. Paediatric formulations are easier to administer and may be better tolerated, particularly in terms of vomiting, which may affect anti-malarial drug levels[57]. A granule formulation was included in the PA development plan to ensure early availability after drug registration. For the primary efficacy outcome used in the Phase III studies – day-28 PCR-corrected ACPR – the granule and tablet formulation had similar efficacy in this analysis. Efficacy outcomes at day 42 were also similar for the two pyronaridine-artesunate formulations.
For the efficacy analysis, this report is concerned with the integrated analysis of the PA Phase III P. falciparum clinical trials. However, the efficacy of PA in P. vivax has also been evaluated in one Phase III study in adults and children[23]. In summary, for the primary outcome – the day-14 crude cure rate (PP population) – PA efficacy was 99.5%, (217/218; 95% CI 97.5, 100). This was non-inferior to CQ 100% efficacy (209/209; 95% CI 98.3, 100); treatment difference −0.5% (95% CI −2.6, 1.4). Non-inferiority of PA to CQ was maintained throughout follow-up (days 21, 28, 35 and 42)[23]. Additional clinical trials will report PA safety and efficacy in young children with P. vivax malaria and PA efficacy in areas of chloroquine-resistant P. vivax.
Conclusions
Overall, PA was well tolerated with a similar adverse event profile to comparators. Although PA was associated with transient increases in transaminases in a relatively small proportion of patients, there was no indication of a risk of progressive liver injury. Pyronaridine-artesunate efficacy against P. falciparum was consistently high regardless of geographical region, patient age, gender, or degree of parasitaemia. Against P. vivax, PA had efficacy at least as good as CQ but with more rapid parasite and fever clearance and a lower parasite re-emergence rate. Importantly, PA has been developed to have a specific paediatric granule formulation available, shown to have equivalent pharmacokinetics and efficacy to the tablet formulation[24]. Initially, PA will be used in areas of low endemicity and where cases of artemisinin resistance have been reported with deployment to areas of high endemicity once further data on repeated treatment with PA have been obtained. Pyronaridine-artesunate is a useful new ACT and should be a valuable addition to anti-malarial treatment programmes.
References
World Health Organization: World Malaria Report. 2011,http://www.who.int/malaria/world_malaria_report_2011/9789241564403_eng.pdf,
Roll Back Malaria Partnership Secretariat: World Malaria Day. 2010,Africa Updatehttp://www.rollbackmalaria.org/ProgressImpactSeries/docs/wmd2010report-en.pdf,
Mueller I, Galinski MR, Baird JK, Carlton JM, Kochar DK, Alonso PL, del Portillo HA: Key gaps in the knowledge of Plasmodium vivax, a neglected human malaria parasite. Lancet Infect Dis. 2009, 9: 555-566. 10.1016/S1473-3099(09)70177-X.
Price RN, Tjitra E, Guerra CA, Yeung S, White NJ, Anstey NM: Vivax malaria: neglected and not benign. Am J Trop Med Hyg. 2007, 77: 79-87.
Guerra CA, Snow RW, Hay SI: Mapping the global extent of malaria in 2005. Trends Parasitol. 2006, 22: 353-358. 10.1016/j.pt.2006.06.006.
Guerra CA, Howes RE, Patil AP, Gething PW, Van Boeckel TP, Temperley WH, Kabaria CW, Tatem AJ, Manh BH, Elyazar IR, Baird JK, Snow RW, Hay SI: The international limits and population at risk of Plasmodium vivax transmission in 2009. PLoS Negl Trop Dis. 2009, 4: e774.
World Health Organization: Guidelines for the treatment of malaria (second edition).http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf,
Wongsrichanalai C, Wimonwattrawatee T, Sookto P, Laoboonchai A, Heppner DG, Kyle DE, Wernsdorfer WH: In vitro sensitivity of Plasmodium falciparum to artesunate in Thailand. Bull World Health Organ. 1999, 77: 392-398.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM: Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008, 359: 2619-2620. 10.1056/NEJMc0805011.
World Health Organization: Report of an informal consultation, Phnom Penh. Containment of malaria multi-drug resistance on the Cambodia-Thailand border.29–30 January 2007http://www.who.int/malaria/publications/multi_drug_resistance_en.pdf,
World Health Organization: Global malaria control and elimination: report of a meeting on containment of artemisinin tolerance.http://whqlibdoc.who.int/publications/2008/9789241596817_eng.pdf,
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, Lwin KM, Ariey F, Hanpithakpong W, Lee SJ, Ringwald P, Silamut K, Imwong M, Chotivanich K, Lim P, Herdman T, An SS, Yeung S, Singhasivanon P, Day NP, Lindegardh N, Socheat D, White NJ: Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009, 361: 455-467. 10.1056/NEJMoa0808859.
Song J, Socheat D, Tan B, Seila S, Xu Y, Ou F, Sokunthea S, Sophorn L, Zhou C, Deng C, Wang Q, Li G: Randomized trials of artemisinin-piperaquine, dihydroartemisinin-piperaquine phosphate and artemether-lumefantrine for the treatment of multi-drug resistant falciparum malaria in Cambodia-Thailand border area. Malar J. 2011, 10: 231. 10.1186/1475-2875-10-231.
Wongsrichanalai C, Meshnick SR: Declining artesunate-mefloquine efficacy against falciparum malaria on the Cambodia-Thailand border. Emerg Infect Dis. 2008, 14: 716-719. 10.3201/eid1405.071601.
Rueangweerayut R, Phyo A, Uthaisin C, Poravuth Y, Binh T, Tinto H, Pénali L, Valecha N, Tien N, Abdulla S, Borghini-Fuhrer I, Duparc S, Shin C-S, Fleckenstein L: Pyronaridine-artesunate versus mefloquine plus artesunate for malaria. NEJM. 2012, 366: 1298-1309. 10.1056/NEJMoa1007125.
Phyo AP, Nkhoma S, Stepniewska K, Ashley EA, Nair S, McGready R, Ler Moo C, Al-Saai S, Dondorp AM, Lwin KM, Singhasivanon P, Day NP, White NJ, Anderson TJ, Nosten F: Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet. 2012, 379: 1960-1966. 10.1016/S0140-6736(12)60484-X.
Douglas NM, Anstey NM, Angus BJ, Nosten F, Price RN: Artemisinin combination therapy for vivax malaria. Lancet Infect Dis. 2010, 10: 405-416. 10.1016/S1473-3099(10)70079-7.
Baird JK: Resistance to therapies for infection by Plasmodium vivax. Clin Microbiol Rev. 2009, 22: 508-534. 10.1128/CMR.00008-09.
Mueller I, Widmer S, Michel D, Maraga S, McNamara DT, Kiniboro B, Sie A, Smith TA, Zimmerman PA: High sensitivity detection of Plasmodium species reveals positive correlations between infections of different species, shifts in age distribution and reduced local variation in Papua New Guinea. Malar J. 2009, 8: 41. 10.1186/1475-2875-8-41.
World Health Organization Regional Office for the Western Pacific: Interregional workshop on the control of vivax malaria in East Asia (Shanghai, China, 17–20 November 2003). http://whqlibdoc.who.int/wpro/2004/RS_2003_GE_42(CHN).pdf
Croft SL, Duparc S, Arbe-Barnes SJ, Craft JC, Shin CS, Fleckenstein L, Borghini-Fuhrer I, Rim HJ: Review of pyronaridine anti-malarial properties and product characteristics. Malar J. 2012, 11: 270. 10.1186/1475-2875-11-270.
Kayentao K, Doumbo OK, Pénali LK, Offianan AT, Bhatt KM, Kimani J, Tshefu AK, Tambwe JKH, Ramharter M, Martinez de Salazar P, Tiono AB, Ouédraogo A, Bustos MDG, Quicho F, Borghini-Fuhrer I, Duparc s, Shin C-S, Fleckenstein L: Pyronaridine-artesunate granules versus artemether-lumefantrine crushed tablets in children with Plasmodium falciparum malaria: a randomized controlled trial. Malar J. 2012, 11: 364. 10.1186/1475-2875-11-364.
Poravuth Y, Socheat D, Rueangweerayut R, Uthaisin C, Pyae Phyo A, Valecha N, Rao BH, Tjitra E, Purnama A, Borghini-Fuhrer I, Duparc S, Shin CS CS, Fleckenstein L: Pyronaridine-artesunate versus chloroquine in patients with acute Plasmodium vivax malaria: a randomized, double-blind, non-inferiority trial. PLoS One. 2011, 6: e14501. 10.1371/journal.pone.0014501.
Ramharter M, Kurth F, Schreier AC, Nemeth J, Glasenapp I, Belard S, Schlie M, Kammer J, Koumba PK, Cisse B, Mordmuller B, Lell B, Issifou S, Oeuvray C, Fleckenstein L, Kremsner PG: Fixed-dose pyronaridine-artesunate combination for treatment of uncomplicated falciparum malaria in pediatric patients in Gabon. J Infect Dis. 2008, 198: 911-919. 10.1086/591096.
Tshefu AK, Gaye O, Kayentao K, Thompson R, Bhatt KM, Sesay SS, Bustos DG, Tjitra E, Bedu-Addo G, Borghini-Fuhrer I, Duparc S, Shin CS, Fleckenstein L: Efficacy and safety of a fixed-dose oral combination of pyronaridine-artesunate compared with artemether-lumefantrine in children and adults with uncomplicated Plasmodium falciparum malaria: a randomised non-inferiority trial. Lancet. 2010, 375: 1457-1467. 10.1016/S0140-6736(10)60322-4.
Price RN, Marfurt J, Chalfein F, Kenangalem E, Piera KA, Tjitra E, Anstey NM, Russell B: In vitro activity of pyronaridine against multidrug-resistant Plasmodium falciparum and Plasmodium vivax. Antimicrob Agents Chemother. 2010, 54: 5146-5150. 10.1128/AAC.00801-10.
Okombo J, Kiara SM, Mwai L, Pole L, Ohuma E, Ochola LI, Nzila A: Baseline in vitro activities of the antimalarials pyronaridine and methylene blue against Plasmodium falciparum isolates from Kenya. Antimicrob Agents Chemother. 2012, 56: 1105-1107. 10.1128/AAC.05454-11.
Zhang CL, Zhou HN, Wang J, Liu H: [In vitro sensitivity of Plasmodium falciparum isolates from China-Myanmar border region to chloroquine, piperaquine and pyronaridine]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2012, 30: 41-44.
World Health Organization: Assessment and monitoring of antimalarial drug efficacy for the treatment of uncomplicated falciparum malaria (WHO/HTM/RBM/2003.50).http://whqlibdoc.who.int/hq/2003/WHO_HTM_RBM_2003.50.pdf,
Felger I, Beck HP: Genotyping of Plasmodium falciparum. PCR-RFLP analysis. Methods Mol Med. 2002, 72: 117-129.
Medicines for Malaria Venture, World Health Organization: Methods and techniques for clinical trials on antimalarial drug efficacy: genotyping to identify parasite populations.http://whqlibdoc.who.int/publications/2008/9789241596305_eng.pdf,
Price R, van Vugt M, Phaipun L, Luxemburger C, Simpson J, McGready R, ter Kuile F, Kham A, Chongsuphajaisiddhi T, White NJ, Nosten F: Adverse effects in patients with acute falciparum malaria treated with artemisinin derivatives. Am J Trop Med Hyg. 1999, 60: 547-555.
Ribeiro IR, Olliaro P: Safety of artemisinin and its derivatives. A review of published and unpublished clinical trials. Med Trop (Mars). 1998, 58: 50-53.
Ringwald P, Bickii J, Basco L: Randomised trial of pyronaridine versus chloroquine for acute uncomplicated falciparum malaria in Africa. Lancet. 1996, 347: 24-28. 10.1016/S0140-6736(96)91558-5.
Ringwald P, Bickii J, Basco LK: Efficacy of oral pyronaridine for the treatment of acute uncomplicated falciparum malaria in African children. Clin Infect Dis. 1998, 26: 946-953. 10.1086/513942.
Agomo PU, Meremikwu MM, Watila IM, Omalu IJ, Odey FA, Oguche S, Ezeiru VI, Aina OO: Efficacy, safety and tolerability of artesunate-mefloquine in the treatment of uncomplicated Plasmodium falciparum malaria in four geographic zones of Nigeria. Malar J. 2008, 7: 172. 10.1186/1475-2875-7-172.
Bhatt KM, Samia BM, Bhatt SM, Wasunna KM: Efficacy and safety of an artesunate/mefloquine combination, (artequin) in the treatment of uncomplicated P. falciparum malaria in Kenya. East Afr Med J. 2006, 83: 236-242.
Bouyou-Akotet MK, Ramharter M, Ngoungou EB, Mamfoumbi MM, Mihindou MP, Missinou MA, Kurth F, Belard S, Agnandji ST, Issifou S, Heidecker JL, Trapp S, Kremsner PG, Kombila M: Efficacy and safety of a new pediatric artesunate-mefloquine drug formulation for the treatment of uncomplicated falciparum malaria in Gabon. Wien Klin Wochenschr. 2010, 122: 173-178. 10.1007/s00508-010-1317-1.
Frey SG, Chelo D, Kinkela MN, Djoukoue F, Tietche F, Hatz C, Weber P: Artesunate-mefloquine combination therapy in acute Plasmodium falciparum malaria in young children: a field study regarding neurological and neuropsychiatric safety. Malar J. 2010, 9: 291. 10.1186/1475-2875-9-291.
Krudsood S, Looareesuwan S, Tangpukdee N, Wilairatana P, Phumratanaprapin W, Leowattana W, Chalermrut K, Ramanathan S, Navaratnam V, Olliaro P, Vaillant M, Kiechel JR, Taylor WR: New fixed-dose artesunate-mefloquine formulation against multidrug-resistant Plasmodium falciparum in adults: a comparative phase IIb safety and pharmacokinetic study with standard-dose nonfixed artesunate plus mefloquine. Antimicrob Agents Chemother. 2010, 54: 3730-3737. 10.1128/AAC.01187-09.
Massougbodji A, Kone M, Kinde-Gazard D, Same-Ekobo A, Cambon N, Mueller EA: A randomized, double-blind study on the efficacy and safety of a practical three-day regimen with artesunate and mefloquine for the treatment of uncomplicated Plasmodium falciparum malaria in Africa. Trans R Soc Trop Med Hyg. 2002, 96: 655-659. 10.1016/S0035-9203(02)90344-5.
Mayxay M, Keomany S, Khanthavong M, Souvannasing P, Stepniewska K, Khomthilath T, Keola S, Pongvongsa T, Phompida S, Ubben D, Valecha N, White NJ, Newton PN: A phase III, randomized, non-inferiority trial to assess the efficacy and safety of dihydroartemisinin-piperaquine in comparison with artesunate-mefloquine in patients with uncomplicated Plasmodium falciparum malaria in southern Laos. Am J Trop Med Hyg. 2010, 83: 1221-1229. 10.4269/ajtmh.2010.10-0276.
Abdulla S, Sagara I, Borrmann S, D’Alessandro U, Gonzalez R, Hamel M, Ogutu B, Martensson A, Lyimo J, Maiga H, Sasi P, Nahum A, Bassat Q, Juma E, Otieno L, Bjorkman A, Beck HP, Andriano K, Cousin M, Lefevre G, Ubben D, Premji Z: Efficacy and safety of artemether-lumefantrine dispersible tablets compared with crushed commercial tablets in African infants and children with uncomplicated malaria: a randomised, single-blind, multicentre trial. Lancet. 2008, 372: 1819-1827. 10.1016/S0140-6736(08)61492-0.
Hatz C, Soto J, Nothdurft HD, Zoller T, Weitzel T, Loutan L, Bricaire F, Gay F, Burchard GD, Andriano K, Lefevre G, De Palacios PI, Genton B: Treatment of acute uncomplicated falciparum malaria with artemether-lumefantrine in nonimmune populations: a safety, efficacy, and pharmacokinetic study. Am J Trop Med Hyg. 2008, 78: 241-247.
Mueller EA, van Vugt M, Kirch W, Andriano K, Hunt P, de Palacios PI: Efficacy and safety of the six-dose regimen of artemether-lumefantrine for treatment of uncomplicated Plasmodium falciparum malaria in adolescents and adults: a pooled analysis of individual patient data from randomized clinical trials. Acta Trop. 2006, 100: 41-53. 10.1016/j.actatropica.2006.09.007.
Sagara I, Rulisa S, Mbacham W, Adam I, Sissoko K, Maiga H, Traore OB, Dara N, Dicko YT, Dicko A, Djimde A, Jansen FH, Doumbo OK: Efficacy and safety of a fixed dose artesunate-sulphamethoxypyrazine-pyrimethamine compared to artemether-lumefantrine for the treatment of uncomplicated falciparum malaria across Africa: a randomized multi-centre trial. Malar J. 2009, 8: 63. 10.1186/1475-2875-8-63.
Naing C, Aung K, Win DK, Wah MJ: Efficacy and safety of chloroquine for treatment in patients with uncomplicated Plasmodium vivax infections in endemic countries. Trans R Soc Trop Med Hyg. 2010, 104: 695-705. 10.1016/j.trstmh.2010.08.009.
Mengesha T, Makonnen E: Comparative efficacy and safety of chloroquine and alternative antimalarial drugs: a meta-analysis from six African countries. East Afr Med J. 1999, 76: 314-319.
White NJ: Cardiotoxicity of antimalarial drugs. Lancet Infect Dis. 2007, 7: 549-558. 10.1016/S1473-3099(07)70187-1.
Karbwang J, Na-Bangchang K, Thanavibul A, Bunnag D, Chongsuphajaisiddhi T, Harinasuta T: Comparison of oral artesunate and quinine plus tetracycline in acute uncomplicated falciparum malaria. Bull World Health Organ. 1994, 72: 233-238.
Karbwang J, Bangchang KN, Thanavibul A, Bunnag D, Chongsuphajaisiddhi T, Harinasuta T: Comparison of oral artemether and mefloquine in acute uncomplicated falciparum malaria. Lancet. 1992, 340: 1245-1248. 10.1016/0140-6736(92)92947-E.
Sowunmi A, Oduola AM: Efficacy of artemether in severe falciparum malaria in African children. Acta Trop. 1996, 61: 57-63. 10.1016/0001-706X(95)00143-3.
Jambou R, Legrand E, Niang M, Khim N, Lim P, Volney B, Ekala MT, Bouchier C, Esterre P, Fandeur T, Mercereau-Puijalon O: Resistance of Plasmodium falciparum field isolates to in-vitro artemether and point mutations of the SERCA-type PfATPase6. Lancet. 2005, 366: 1960-1963. 10.1016/S0140-6736(05)67787-2.
Bousema T, Okell L, Shekalaghe S, Griffin JT, Omar S, Sawa P, Sutherland C, Sauerwein R, Ghani AC, Drakeley C: Revisiting the circulation time of Plasmodium falciparum gametocytes: molecular detection methods to estimate the duration of gametocyte carriage and the effect of gametocytocidal drugs. Malar J. 2010, 9: 136. 10.1186/1475-2875-9-136.
Sowunmi A, Balogun T, Gbotosho GO, Happi CT, Adedeji AA, Bolaji OM, Fehintola FA, Folarin OA: Activities of artemether-lumefantrine and amodiaquine-sulfalene-pyrimethamine against sexual-stage parasites in falciparum malaria in children. Chemotherapy. 2008, 54: 201-208. 10.1159/000140463.
Agnandji ST, Kurth F, Belard S, Mombo-Ngoma G, Basra A, Fernandes JF, Soulanoudjingar SS, Adegnika AA, Ramharter M: Current status of the clinical development and implementation of paediatric artemisinin combination therapies in Sub-Saharan Africa. Wien Klin Wochenschr. 2011, 123 (1): 7-9. 10.1007/s00508-011-0039-3.
Kurth F, Belard S, Adegnika AA, Gaye O, Kremsner PG, Ramharter M: Do paediatric drug formulations of artemisinin combination therapies improve the treatment of children with malaria? A systematic review and meta-analysis. Lancet Infect Dis. 2010, 10: 125-132. 10.1016/S1473-3099(09)70327-5.
Acknowledgements
We thank the study population and local staff who made these studies possible. We would also like to acknowledge the contributions of Ghiorghis Belai, David Asante, and Pongphaya Choosakulchart (Family Health International) and their teams and Hermann Garden (Swiss Tropical Institute) and his team who were in charge of the studies monitoring. Eric Didillon, Audrey Mulder (Fulcrum Pharma, UK) and Claude Oeuvray (MMV) for their dedicated work in the set-up and execution of the trials. Hanspeter Marti and Hans-Peter Beck (Swiss Tropical Institute), who performed the slides central reading and the PCR analysis. We thank Stephen Allen (Swansea University, UK), Frank Stephen Wignall (Family Health International) for their participation in the Safety Review Team. We thank Colin Sutherland (London School of Hygiene & Tropical Medicine) for his contribution on the analysis and discussion related to the gametocytes. Statistical analyses were carried out by Aptiv Solutions (formerly Averion), Basel, Switzerland, with the dedicated work of Mikael Saulay, Arnaud Demange and Abdallah Ennaji and by DataMap (Freiburg, Germany) with the dedicated work of Martina Wibberg and Carmen Wiesmann. Naomi Richardson of Magenta Communications Ltd provided editorial assistance and was funded by Medicines for Malaria Venture. Pyronaridine-artesunate is being developed in a public–private partnership between Shin Poong Pharmaceutical Company Ltd, Seoul, Republic of Korea and Medicines for Malaria Venture, Geneva, Switzerland. The sponsors and study site principal investigators developed the protocols, interpreted the data and developed the report. The study sponsors were responsible for data collection and statistical analysis. All authors had access to the primary data, take responsibility for data reporting accuracy and completeness and had responsibility for the final decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
SD, and IB-F are employees of MMV; JCC is a former employee of MMV; SA-B and RMM are contractors employed by MMV; C-SS is a former employee of Shin Poong Pharmaceutical Co. Ltd.; LF is an advisor to MMV.
Authors’ contributions
All authors were involved in study design and conduct, contributed to the paper and approved the final version for submission.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Duparc, S., Borghini-Fuhrer, I., Craft, C.J. et al. Safety and efficacy of pyronaridine-artesunate in uncomplicated acute malaria: an integrated analysis of individual patient data from six randomized clinical trials. Malar J 12, 70 (2013). https://doi.org/10.1186/1475-2875-12-70
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-12-70