Abstract
Background
The influence of intensive glucose control in diabetic patients on the macrovascular outcomes is controversial. Thus, this study aimed to elucidate the effect of preprocedural hemoglobin A1c (HbA1c) on clinical outcomes after endovascular therapy for lower extremity artery disease (LEAD) in diabetic patients.
Methods
Diabetic patients were enrolled from the retrospective cohorts of a Korean multicenter endovascular therapy registry and were divided according to the HbA1c level during index admission into the optimal (< 7.0%) or suboptimal (≥ 7.0%) glycemic control groups. The primary endpoints were major adverse limb events (MALE, a composite of major amputation, minor amputation, and reintervention).
Results
Of the 1103 patients enrolled (897 men, mean age 68.2 ± 8.9 years), 432 (39.2%) were classified into the optimal glycemic control group and 671 (60.8%) into the suboptimal glycemic control group. In-hospital events and immediate procedural complications were not different between the two groups. The suboptimal group showed a trend towards a higher incidence of MALE than the optimal group (log-rank p = 0.072). Although no significant differences were found between the two groups in terms of overall survival or amputation, the risk of reintervention was significantly higher in the suboptimal group (log-rank p = 0.048). In the multivariate Cox regression model, suboptimal glycemic control was one of the independent predictors for reintervention. When our data were analyzed according to the initial presentation, suboptimal preprocedural HbA1c significantly increased the incidence of MALE compared with optimal preprocedural HbA1c only in patients with intermittent claudication.
Conclusion
In diabetic patients undergoing endovascular therapy for LEAD, suboptimal preprocedural HbA1c is associated with an increased risk of adverse limb events, especially in patients with intermittent claudication. Further prospective research will be required to validate the role of more intensive glycemic control on the reduction of adverse limb events in diabetic patients undergoing endovascular therapy for LEAD.
Similar content being viewed by others
Background
Diabetes mellitus (DM) is associated with the development of peripheral artery disease (PAD) [1]. Both the duration and severity of DM are associated with increased risk of PAD [2, 3]. The prognosis of PAD is worse in DM patients than in non-DM patients. Infrapopliteal arterial involvement is more common and the need for a major amputation is higher in DM patients than in non-DM patients [4, 5].
The cardiovascular effect of intensive glucose control on the macrovascular events among DM patients is controversial. In randomized trials, intensive glucose control in DM patients did not reduced major cardiovascular events compared with standard glucose management [6,7,8]. However, several studies suggested that poor glycemic control at the time of peripheral angioplasty was associated with worse clinical outcomes in patients with critical limb ischemia (CLI) [9, 10]. In a recent retrospective analysis of US veterans undergoing lower extremity revascularization, patients with lower extremity artery disease (LEAD) and poor glycemic control were at higher risk of amputation and modified major adverse limb events than were those with good glycemic control [11].
The present study aimed to investigate the effect of suboptimal preprocedural hemoglobin A1c (HbA1c) on clinical outcomes of endovascular therapy in LEAD patients with DM using a nationwide, multicenter, real-world registry.
Methods
Study population
The Korean Vascular Intervention Society Endovascular therapy in Lower Limb Artery diseases (K-VIS ELLA) registry is a multicenter observational study with retrospective and prospective cohorts of patients with lower extremity artery disease treated with endovascular therapy (ClinicalTrials.gov NCT02748226). The retrospective patient cohort consisted of 3434 patients with 5097 affected limbs treated between January 2006 and July 2015 in 31 Korean hospitals. The K-VIS ELLA registry study design and results have been described in detail previously [12]. A total of 3073 patients with 3972 target limbs were finally analyzed after exclusion of 56 limbs with acute limb ischemia, 82 limbs with Buerger’s disease, 11 limbs lacking procedural or in-hospital data, 528 limbs lacking follow-up data after hospital discharge, and 448 limbs treated for repeat revascularization following the index procedure.
From this registry population, 1103 DM patients (1420 limbs) who had HbA1c levels available during index admission were finally included in the current analysis (Fig. 1). HbA1c levels were dichotomized into optimal (< 7.0%) and suboptimal (≥ 7.0%) according to American Diabetes Association recommendations [13]. Data on patient demographics, baseline clinical and lesion characteristics, medication history, clinical presentation, laboratory test results, treatments, and follow-up outcomes were collected from electronic medical records.
The study protocol was approved by the institutional review board of each hospital and was conducted according to the principles of the Declaration of Helsinki. The institutional review boards of the participating hospitals waived the requirement of informed consent due to the retrospective nature of the study.
Definitions and study endpoints
LEAD was defined as the presence of ≥ 50% narrowing of a lower extremity artery. Claudication was defined as Rutherford category 1, 2, or 3 disease and CLI was defined as Rutherford category 4, 5, or 6 disease [14]. The presence of diabetes was identified by history and medical records including outpatient clinics and prescriptions of oral hypoglycemic agents or insulin. Definitions of hypercholesterolemia, smoking, congestive heart failure, anemia, and chronic kidney disease were described in a previous report [12].
Technical success was defined as successful revascularization with residual stenosis < 30% and absence of flow-limiting dissection or a hemodynamically significant translesion pressure gradient. Major amputation was defined as any lower extremity amputation at the level of or above the ankle, and a minor amputation was defined as any lower extremity amputation below the ankle, including the foot or toe(s).
The primary endpoints of this study were major adverse limb events (MALE; a composite of major amputation, minor amputation, and reintervention). Secondary endpoints were all-cause mortality, any amputation, and reintervention. These outcomes were compared between optimal glycemic control and suboptimal glycemic control groups according to the HbA1c level during the index admission.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and were compared using the Student’s t-test for parametric data and the Mann–Whitney test for nonparametric data. Categorical variables were expressed as number (percentage) and were compared using the Chi square test or Fisher’s exact test. Data were analyzed on a per-patient basis for clinical characteristics and on a per-lesion basis for the limb, lesion, or procedural characteristics. Cumulative incidences of clinical events were presented as Kaplan–Meier estimates and were compared using the log-rank test. Univariate Cox proportional hazards regression analyses using baseline clinical, lesion, and procedural variables were performed to identify factors associated with clinical events. The variables achieving P-values < 0.20 in the univariate analysis were evaluated in the multivariate analysis model to determine the independent predictors of clinical events. All statistical analyses were performed using SPSS (version 23.0; IBM Corp., Armonk, NY, USA). All tests were two-sided, and P < 0.05 was considered statistically significant.
Results
Baseline characteristics
Baseline clinical characteristics of patients according to HbA1c levels during index admission are summarized in Table 1. Of the 1103 patients enrolled, 432 (39.2%) were categorized into the optimal glycemic control group (HbA1c < 7.0) and 671 (60.8%) were placed into the suboptimal glycemic control group (HbA1c ≥ 7.0). The mean age of the entire cohort was 68.2 ± 8.9 years, and 897 (81.3%) patients were men. Compared with the patients in the suboptimal group, those in the optimal group were older, were predominantly male, and had a higher prevalence of chronic kidney disease and congestive heart failure. Patients in the suboptimal group were more likely to be on insulin therapy for glycemic control. Initial clinical presentations based on the Rutherford classification were not different between the two groups.
Procedural characteristics and complications
Table 2 demonstrates baseline lesion and procedural characteristics according to HbA1c levels during the index admission. No significant differences were found between the groups except that there were slightly more targeted blood vessels in the suboptimal group. Total in-hospital events and immediate procedural complications were not different between the two groups (Fig. 2).
In-hospital outcomes and procedural complication rates according to HbA1c level during index admission. Crude incidence of death, reintervention, amputation, bleeding complication, access site complication, distal embolization, and vascular rupture for optimal (blue) and suboptimal (red) glucose control groups. HbA1c hemoglobin A1c
Follow-up clinical outcomes and independent predictors
The median follow-up duration was 724 days (interquartile range 326–782 days). The Kaplan–Meier curves in Fig. 3 illustrate freedom from MALE, death, amputation, and reintervention stratified by initial HbA1c status. The suboptimal group showed a trend toward higher incidence of MALE than the optimal group (log-rank p = 0.072, Fig. 3a). No significant differences were observed between the two groups in terms of overall survival (Fig. 3b) or amputation (Fig. 3c) during the follow-up period. However, the suboptimal group demonstrated a significant disadvantage with regard to reintervention (log-rank p = 0.048, Fig. 3d). In the multivariate Cox regression model, the use of insulin for glycemic control, end-stage renal disease, previous history of amputation, previous history of endovascular therapy, and CLI were independent predictors of MALE (Table 3). Independent predictors for reintervention during follow-up were end-stage renal disease, previous history of endovascular therapy, and suboptimal glycemic control defined as HbA1c ≥ 7.0% (Table 4).
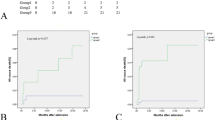
Influence of preprocedural HbA1c levels on clinical outcomes according to the initial presentation
To assess the influence of preprocedural HbA1c levels on clinical outcomes according to the initial clinical presentation, we analyzed data separately in patients with intermittent claudication or CLI (Fig. 4). Among CLI patients, no difference was found in the incidence of MALE between the optimal and suboptimal groups (Fig. 4a). However, among patients who presented with claudication, the suboptimal group showed a higher incidence of MALE than the optimal group (log rank p = 0.039, Fig. 4b).
Discussion
Main findings
We reported the association between the preprocedural glycemic control based on HbA1c during index admission and clinical outcomes in DM patients undergoing endovascular therapy for LEAD. Although not statistically significant, the suboptimal glycemic control group (HbA1c ≥ 7.0) showed a tendency towards higher incidence of MALE than in the optimal glycemic control group (HbA1c < 7.0). Elevated preprocedural HbA1c was associated with higher risk of reintervention. Suboptimal glycemic control was an independent predictor of reintervention during the follow-up period after endovascular therapy in DM patients with LEAD. Because CLI was one of the independent predictors for MALE, we further analyzed our data by dividing it into the presence of claudication and CLI according to the initial presentation. Suboptimal preprocedural HbA1c did not affect the outcome in CLI patients; however, among those with intermittent claudication, suboptimal preprocedural HbA1c significantly increased the incidence of MALE compared with optimal glycemic control.
Role of glycemic control on vascular outcomes
The role of intensive glucose control on the macrovascular outcomes in DM patients is unclear. Although large randomized controlled trials failed to demonstrate the benefits of intensive glucose control in reducing major cardiovascular events [6,7,8], recent post hoc analyses of several randomized trials demonstrated that higher HbA1c was associated with increased risk of major cardiovascular events [15, 16] and lower extremity amputation [17].
For the management of LEAD, recent practice guidelines recommended adequate glycemic control in DM patients [18,19,20], and several retrospective observational studies suggested that poor glycemic control may be associated with worse clinical outcomes of vascular procedure in DM patients with LEAD. In a single-center study of 278 CLI patients undergoing balloon angioplasty, Takahara et al. reported that the presence of diabetes was independently associated with major amputation and, in the DM subgroup, poor glycemic control was associated with higher amputation rates [9]. Similarly, in another single-center study, Singh et al. analyzed the effect of pre-procedural fasting blood glucose on primary patency and limb outcomes following infrapopliteal balloon angioplasty in 149 DM patients with CLI [10]. They found that fasting blood glucose above the median value at the time of the procedure was associated with lower primary patency at 1 year [10]. However, these were single-center studies with relatively small sample size and only CLI patients were enrolled. Therefore, the results cannot be generalized to all LEAD patients.
Recently, Arya et al. reported a large retrospective study using Veterans Health Administration data to evaluate the influence of elevated perioperative HbA1c on outcomes in LEAD patients undergoing surgical or endovascular revascularization procedures [11]. In that study, high HbA1c level was incrementally associated with higher risk of amputation and MALE regardless of the preoperative diagnosis of DM [11]. In the present study, we found no significant differences between the two groups in terms of risk of amputation or MALE, although the suboptimal group showed a trend toward higher incidence of MALE than the optimal group. Compared with the aforementioned studies, the relatively lower incidence of amputation in our study groups may be one of the reasons for the differences. Furthermore, the subjects of Arya et al.’s study were veterans, most of whom were male, and approximately 40% of the subjects were not diagnosed with DM preoperatively. Furthermore, LEAD severity was not specified in more than a third of the enrolled patients. These might be possible reasons for the discrepancies between our results and those of Arya et al. Recent studies in patients undergoing open vascular surgery demonstrated that poor glycemic control was associated with earlier postoperative outcomes such as in-hospital limb events [21] or 30-day mortality [22, 23]. Compared with the results from studies in patients undergoing endovascular therapy, earlier effect of poor glycemic control on postoperative outcomes observed in patients undergoing vascular surgery may be attributed to surgery-related complications such as wound complications or postoperative infections.
When our data were analyzed separately in two groups according to initial presentation, the benefit of optimal glycemic control in reducing the risk of MALE was observed only in patients presenting with claudication. Considering the seriousness of the CLI as an independent risk factor for MALE, intensive glucose control possibly did not significantly reduce the incidence of MALE in CLI patients. Relatively lower incidence of amputation in our study may also have affected the results. A recent study evaluated the association between preoperative HbA1c levels and clinical outcomes after lower extremity bypass surgery and found that poor preoperative glycemic control increased the risk of in-hospital limb events [21]. Similar to our findings, the increased risk for adverse limb events in patients with high preoperative HbA1c level was only observed in patients without CLI [21].
Other factors related to PAD outcomes
In addition to HbA1c, various biomarkers have been suggested to be related to clinical outcomes of PAD in DM patients. Zhao et al. investigated the association of vascular damage with the triglyceride-glucose index as a simple surrogate marker of insulin resistance [24]. They demonstrated that an increased triglyceride-glucose index was significantly associated with a higher risk of arterial stiffness and renal microvascular damage, but not with PAD [24]. Biscetti et al. demonstrated that circulating sortilin levels were associated with the presence and severity of LEAD in statin-naïve DM patients [25]. Biscetti et al. found that omentin-1 serum levels were significantly lower in DM patients with PAD than in DM patients without PAD, and omentin-1 levels were related to disease severity [26]. Elevated levels of various inflammatory cytokines such as osteoprotegerin, tumor necrosis factor-a, interleukin-6, and C-reactive protein were also reported to be related with worse vascular outcomes in DM patients with LEAD undergoing infrapopliteal endovascular therapy [27]. These potential surrogate biomarkers may be helpful to better stratify PAD risk in DM patients. Their usefulness should be confirmed in future studies.
In addition to molecular biomarkers, several clinical confounding factors may influence on clinical outcomes of LEAD in DM patients. It has been shown that women with LEAD have more functional impairment and worse outcomes than men [28]. Although these gender differences were not observed in the present study population, in a previous study performed on the entire cohort from our registry, women had higher rates of major adverse cardiovascular events and MALE [29]. Frailty is also associated with poor clinical outcomes after vascular interventions for LEAD [30], although increasing numbers of peripheral vascular intervention for older patients was shown to correlate with decreasing major amputation rates [31].
Limitations
This study has several limitations. First, given the retrospective nature of the study, the causal relationships could not be determined. Therefore, prospective randomized trials will be required to validate the role of more intensive glycemic control on the reduction of adverse limb events in DM patients with LEAD undergoing endovascular therapy. Second, the HbA1c level that we used as the basis of glycemic control was measured once before the procedure, and data on changes in glycemic control during the follow-up period were not available. Therefore, dramatic changes in blood glucose levels during follow-up may have affected the clinical outcomes. However, HbA1c reflects the average blood glycemic level over approximately 3 months [13], and the measurement of HbA1c was performed during the index admission in all cases. At least our data highlight the importance of glycemic control during preprocedural period. Third, the strategy for hyperglycemia management was not standardized. Recent studies have shown that novel glucose-lowering agents can reduce the risk of cardiovascular events in patients with atherosclerotic cardiovascular disease [32]. However, increased risk of lower limb amputation has been reported for certain sodium-glucose cotransporter type-2 inhibitors in patients with LEAD [33]. For these reasons, the optimal method of glycemic control is an important topic to be addressed in future studies.
Conclusion
In DM patients undergoing endovascular therapy for LEAD, suboptimal preprocedural HbA1c is associated with increased risk of adverse limb events, especially in patients with intermittent claudication. Future research will have to determine whether more intensive glycemic control can improve clinical outcomes after endovascular therapy in DM patients with LEAD.
Abbreviations
- CLI:
-
Critical limb ischemia
- DM:
-
Diabetes mellitus
- HbA1c:
-
Hemoglobin A1c
- LEAD:
-
Lower extremity artery disease
- MALE:
-
Major adverse limb events
- PAD:
-
Peripheral artery disease
References
Fowkes FG, Aboyans V, Fowkes FJ, McDermott MM, Sampson UK, Criqui MH. Peripheral artery disease: epidemiology and global perspectives. Nat Rev Cardiol. 2017;14(3):156–70.
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, Golden SH. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141(6):421–31.
Kallio M, Forsblom C, Groop PH, Groop L, Lepantalo M. Development of new peripheral arterial occlusive disease in patients with type 2 diabetes during a mean follow-up of 11 years. Diabetes Care. 2003;26(4):1241–5.
Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24(8):1433–7.
Haltmayer M, Mueller T, Horvath W, Luft C, Poelz W, Haidinger D. Impact of atherosclerotic risk factors on the anatomical distribution of peripheral arterial disease. Int Angiol. 2001;20(3):200–7.
Action to Control Cardiovascular Risk in Diabetes Study G, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Group AC, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–39.
Takahara M, Kaneto H, Iida O, Gorogawa S, Katakami N, Matsuoka TA, Ikeda M, Shimomura I. The influence of glycemic control on the prognosis of Japanese patients undergoing percutaneous transluminal angioplasty for critical limb ischemia. Diabetes Care. 2010;33(12):2538–42.
Singh S, Armstrong EJ, Sherif W, Alvandi B, Westin GG, Singh GD, Amsterdam EA, Laird JR. Association of elevated fasting glucose with lower patency and increased major adverse limb events among patients with diabetes undergoing infrapopliteal balloon angioplasty. Vasc Med. 2014;19(4):307–14.
Arya S, Binney ZO, Khakharia A, Long CA, Brewster LP, Wilson PW, Jordan WD Jr, Duwayri Y. High hemoglobin A1c associated with increased adverse limb events in peripheral arterial disease patients undergoing revascularization. J Vasc Surg. 2018;67(1):217–228.e211.
Ko Y-G, Ahn C-M, Min P-K, Lee J-H, Yoon C-H, Yu CW, Lee SW, Lee S-R, Choi SH, Koh YS, et al. Baseline characteristics of a retrospective patient cohort in the korean vascular intervention society endovascular therapy in lower limb artery diseases (K-VIS ELLA) registry. Korean Circ J. 2017;47(4):469–76.
Glycemic Targets: Standards of medical care in diabetes-2019. Diabetes Care. 2019, 42(Suppl 1):S61–S70.
Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, Jones DN. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517–38.
Cavender MA, Scirica BM, Raz I, Steg PG, McGuire DK, Leiter LA, Hirshberg B, Davidson J, Cahn A, Mosenzon O, et al. Cardiovascular outcomes of patients in SAVOR-TIMI 53 by baseline hemoglobin A1c. Am J Med. 2016;129(3):340 e341–8.
Low Wang CC, Blomster JI, Heizer G, Berger JS, Baumgartner I, Fowkes FGR, Held P, Katona BG, Norgren L, Jones WS, et al. Cardiovascular and limb outcomes in patients with diabetes and peripheral artery disease: the EUCLID trial. J Am Coll Cardiol. 2018;72(25):3274–84.
Goldman MP, Clark CJ, Craven TE, Davis RP, Williams TK, Velazquez-Ramirez G, Hurie JB, Edwards MS. Effect of intensive glycemic control on risk of lower extremity amputation. J Am Coll Surg. 2018;227(6):596–604.
Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, Driver VR, Frykberg R, Carman TL, Marston W, et al. The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;63(2 Suppl):3S–21S.
Society for Vascular Surgery Lower Extremity Guidelines Writing G, Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, Mills JL, Moneta GL, Murad MH, Powell RJ, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015;61(3 Suppl):2S–41S.
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FGR, Hamburg NM, Kinlay S, et al. 2016 AHA/ACC Guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;69(11):e71–126.
Singh N, Zeng C, Lewinger JP, Wolfson AM, Shavelle D, Weaver F, Garg PK. Preoperative hemoglobin A1c levels and increased risk of adverse limb events in diabetic patients undergoing infrainguinal lower extremity bypass surgery in the Vascular Quality Initiative. J Vasc Surg. 2019;70(4):1225–34 e1221.
Long CA, Fang ZB, Hu FY, Arya S, Brewster LP, Duggan E, Duwayri Y. Poor glycemic control is a strong predictor of postoperative morbidity and mortality in patients undergoing vascular surgery. J Vasc Surg. 2019;69(4):1219–26.
McGinigle KL, Kindell DG, Strassle PD, Crowner JR, Pascarella L, Farber MA, Marston WA, Arya S, Kalbaugh CA. Poor glycemic control is associated with significant increase in major limb amputation and adverse events in the 30-day postoperative period after infrainguinal bypass. J Vasc Surg. 2020. https://doi.org/10.1016/j.jvs.2019.11.048.
Zhao S, Yu S, Chi C, Fan X, Tang J, Ji H, Teliewubai J, Zhang Y, Xu Y. Association between macro- and microvascular damage and the triglyceride glucose index in community-dwelling elderly individuals: the Northern Shanghai Study. Cardiovasc Diabetol. 2019;18(1):95.
Biscetti F, Bonadia N, Santini F, Angelini F, Nardella E, Pitocco D, Santoliquido A, Filipponi M, Landolfi R, Flex A. Sortilin levels are associated with peripheral arterial disease in type 2 diabetic subjects. Cardiovasc Diabetol. 2019;18(1):5.
Biscetti F, Nardella E, Bonadia N, Angelini F, Pitocco D, Santoliquido A, Filipponi M, Landolfi R, Flex A. Association between plasma omentin-1 levels in type 2 diabetic patients and peripheral artery disease. Cardiovasc Diabetol. 2019;18(1):74.
Biscetti F, Ferraro PM, Hiatt WR, Angelini F, Nardella E, Cecchini AL, Santoliquido A, Pitocco D, Landolfi R, Flex A. Inflammatory cytokines associated with failure of lower-extremity endovascular revascularization (ler): a prospective study of a population with diabetes. Diabetes Care. 2019;42(10):1939–45.
Patel T, Baydoun H, Patel NK, Tripathi B, Nanavaty S, Savani S, Mojadidi MK, Agarwal N, Patel G, Patel S, et al. Peripheral arterial disease in women: the gender effect. Cardiovasc Revasc Med. 2020;21(3):404–8.
Choi KH, Park TK, Kim J, Ko YG, Yu CW, Yoon CH, Lee JH, Min PK, Koh YS, Chae IH, et al. Sex Differences in outcomes following endovascular treatment for symptomatic peripheral artery disease: an analysis from the K- VIS ELLA registry. J Am Heart Assoc. 2019;8(2):e010849.
Drudi LM, Ades M, Mancini R, Boudrias C, Obrand DI, Steinmetz OK, Afilalo J. Frailty assessment in older adults undergoing interventions for peripheral arterial disease. J Vasc Surg. 2019;70(5):1594–1602.e1591.
Kreutzburg T, Peters F, Riess HC, Hischke S, Marschall U, Kriston L, L’Hoest H, Sedrakyan A, Debus ES, Behrendt CA. Editor’s Choice—comorbidity patterns among patients with peripheral arterial occlusive disease in Germany: a trend analysis of health insurance claims data. Eur J Vasc Endovasc Surg. 2020;59(1):59–66.
Das SR, Everett BM, Birtcher KK, Brown JM, Cefalu WT, Januzzi JL Jr, Kalyani RR, Kosiborod M, Magwire ML, Morris PB, et al. 2018 ACC Expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a report of the american college of cardiology task force on expert consensus decision pathways. J Am Coll Cardiol. 2018;72(24):3200–23.
Chatterjee S, Bandyopadhyay D, Ghosh RK, Majumdar U, Aneja A, Lavie CJ, Deedwania P. SGLT-2 inhibitors and peripheral artery disease: a statistical hoax or reality? Curr Probl Cardiol. 2019;44(7):207–22.
Acknowledgements
The K-VIS (Korean Vascular Intervention Society) investigators include Woong Chol Kang, Gachon University Gil Medical Center, Incheon, Korea; Sung-Ho Her, The Catholic University of Korea Daejon St. Mary’s Hospital, Daejon, Korea; Yoon Seok Koh, The Catholic University of Korea Seoul St. Mary’s Hospital, Seoul, Korea; Byung-Hee Hwang, The Catholic University of Korea St. Paul’s Hospital, Seoul, Korea; Ae-Young Her, Kangwon National University Hospital, Chuncheon, Korea; Weon Kim, Kyung Hee University Hospital, Seoul, Korea; Cheol Woong Yu, Korea University Anam Hospital, Seoul, Korea; Sang Cheol Jo, Gwangju Veterans Hospital, Gwangju, Korea; Sanghoon Shin, National Health Insurance Service Ilsan Hospital, Goyang, Korea; Yun Hyeong Cho, Myongi Hospital, Goyang, Korea; Woo-Young Chung, Seoul National University Boramae Medical Center, Seoul, Korea; In-Ho Chae, Chang-Hwan Yoon, Seoul National University Bundang Hospital, Seongnam, Korea; Jung Kyu Han, Seoul National University Hospital, Seoul, Korea; Seung Whan Lee, Asan Medical Center, University of Ulsan, Seoul, Korea; Seung Hyuk Choi, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; Young Jin Choi, Sejong General Hospital, Bucheon, Korea; Su Hyun Kim, St. Carollo Hospital, Suncheon, Korea; Sang Ho Park, Soon Chun Hyang University Cheonan Hospital, Cheonan, Korea; Pil-Ki Min, Gangnam Severance Hospital, Yonsei University, Seoul, Korea; Donghoon Choi, Young-Guk Ko, Chul-Min Ahn, Severance Cardiovascular Hospital, Yonsei University, Seoul, Korea; Young Jin Yoon, Wonju Severance Christian Hospital, Yonsei University, Wonju, Korea; Jung-Hee Lee, Yeungnam University Hospital, Daegu, Korea; Yu Jeong Choi, Eulji University Hospital, Daejon, Korea; Sung Kee Ryu, Eulji General Hospital, Seoul, Korea; Ju Han Kim, Chonnam National University Hospital, Gwangju, Korea; Sang-Rok Lee, Chonbuk National University Hospital, Jeonju, Korea; Hoyoun Won, Chung-Ang University Hospital, Seoul, Korea; Ju Yeol Baek, Cheongju St. Mary’s Hospital, Cheongju, Korea; Jae-Hwan Lee, Chungnam National University Hospital, Daejon, Korea; Jang-Hwan Bae, Chungbuk National University Hospital, Cheongju, Korea; Hyun-Sook Kim, Hallym University Sacred Heart Hospital, Seoul, Korea.
Author information
Authors and Affiliations
Consortia
Contributions
JC, HK, and PM conceived and designed the study; YK, DC, JL, CY, IC, CWY, SWL, SL, SHC, YSK, and PM contributed to data acquisition; JC, HK, and PM analyzed the data; JC and PM wrote the manuscript; YK, DC, JL, CY, IC, CWY, SWL, SL, SHC, YSK, and PM critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cha, JJ., Kim, H., Ko, YG. et al. Influence of preprocedural glycemic control on clinical outcomes of endovascular therapy in diabetic patients with lower extremity artery disease: an analysis from a Korean multicenter retrospective registry cohort. Cardiovasc Diabetol 19, 97 (2020). https://doi.org/10.1186/s12933-020-01072-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-020-01072-x