Abstract
Background
Sortilin is a 95-kDa protein which has recently been linked to circulating cholesterol concentration and lifetime risk of developing significant atherosclerotic disease. Sortilin is found inside different cell types and circulating in blood. Higher circulating sortilin concentration has been found in patients with coronary atherosclerosis compared to control subjects. Sortilin concentration is influenced by statin therapy.
Methods
We enrolled statin-naïve subjects with type 2 diabetes mellitus and we performed a cross-sectional study to evaluate the association between sortilin levels and the presence of clinically significant lower limb peripheral artery disease (PAD) in a population of statin-free diabetic subjects.
Results
Out of the 154 patients enrolled in our study, 80 patients were free from PAD, while 74 had clinically significant PAD. Sortilin concentration was significantly higher in the latter group compared to the former (1.61 ± 0.54 ng/mL versus 0.67 ± 0.30 ng/mL, P < 0.01) and there was a trend toward increased sortilin levels as disease severity increased. The association of sortilin levels with PAD remained after adjusting for major risk factors in a multivariate analysis.
Conclusions
We showed that sortilin is significantly and independently associated with the presence of lower limb PAD in a statin-free diabetic population and it may be a promising marker for clinically significant atherosclerosis of the lower limbs. Further studies are needed to confirm this finding and to evaluate its clinical usefulness.
Similar content being viewed by others
Background
Sortilin, a 95-kDa protein mainly expressed in hepatocytes, takes part in intracellular protein sorting between the trans-Golgi network and endosomes [1]. In a lesser quantity, it is also expressed on cell membrane and small quantities of sortilin have been found in circulating form. Sortilin is codified on chromosome 13 by the gene SORT1, whose polymorphisms have been linked with circulating levels of low-density lipoprotein (LDL) cholesterol and with the lifetime risk of developing clinically significant atherosclerosis [2,3,4,5,6,7,8,9,10,11,12].
Sortilin seems to take part in apolipoproteins trafficking inside hepatocytes, binding to apoB100 and promoting its trafficking to endosomal system, thereby promoting its degradation and reducing circulating levels of very low-density lipoprotein (VLDL). Moreover, membrane sortilin acts as a receptor for circulating LDL, promoting their uptake by hepatocytes via an LDL-receptor (R)-independent mechanism [13,14,15,16,17]. After the discovery of its link to atherosclerosis, there has been considerable interest in elucidating additional functions of sortilin in different cell types. Thus, sortilin has been discovered to play a role in intracellular cytokine traffic [18, 19] and to be expressed in platelets, from where it is released after activation [20]. Among those additional roles, the sortilin function as a membrane LDL-R has been implicated in LDL uptake by macrophages and in foam cell formation and directly in inflammatory mechanisms during atherosclerotic plaque formation and progression [21, 22]. Additionally, sortilin seems to be a fundamental player in hepatic and muscular response to insulin and may be a missing link between insulin resistance and hypercholesterolemia [23,24,25].
Aside from its potential as a therapeutic target, sortilin has been found in increased quantities in patients with coronary artery disease (CAD) and in patients with CAD risk factors compared to control subjects [20, 26].
Peripheral artery disease (PAD) is a well-known manifestation of atherosclerosis, which is associated with considerable disability and mortality. Lower limb PAD (LL-PAD) is of particular concern in diabetic patients and in active or current smokers, where the incidence and prevalence of the disease are particularly high. Ankle-brachial index (ABI) is currently recommended as the main screening tool for PAD in diabetic patients and in those with multiple risk factors [27]. A reduction in ABI, however, represents an already clinically significant stage of the disease. A tool used to find patients with higher risk of developing significant LL-PAD would be useful in identifying patients at a particularly high risk of developing clinically significant PAD and in tailoring more aggressive preventive and diagnostic strategies.
Considering the already proven links between the sortilin and multiple aspects of atherosclerosis [28, 29], metabolic imbalance [30] and diabetes [31], it is possible to hypothesize a connection between sortilin and PAD in the diabetic scenario.
Methods
The aim of this study was to assess the possible role of sortilin as an easy-to-measure marker for the presence of LL-PAD in an in-patient population with type 2 diabetes mellitus (T2DM).
Study design
We performed a cross-sectional study which was approved by the Ethics Committee of the Fondazione Policlinico Universitario A. Gemelli IRCCS and adhered to the principles of the Declaration of Helsinki. All the individuals agreed to participate in the study and gave informed consent. We analyzed the diabetic patients consecutively admitted to the Department of Vascular Diseases of the Fondazione Policlinico Universitario A. Gemelli IRCCS, Roma, Italy, from October 1, 2015 to January 30, 2018. Each patient admitted to the unit during the study time was evaluated for the enrollment in the present study. To be enrolled, each patient had to fulfill the criteria shown in Table 1.
We enrolled diabetic patients with or without PAD. Type 2 diabetes mellitus was defined as a fasting plasma glucose ≥ 126 mg/dL and/or HbA1c ≥ 6.5% or as medical history for the presence of diabetes plus treatment with diabetes medication. Each patient enrolled in the study had his/her medical history assessed for the presence of PAD symptoms or a confirmed PAD diagnosis. For each diabetic patient evaluated in the study, ABI was performed. Patients with clinical findings consistent with PAD underwent ABI measurement and either lower limb arterial Doppler-enhanced ultrasonography, lower limb angiography or computed tomography (CT)-angiography, at the attending physician’s judgment. The patients with a > 0.90 ABI measurement and without symptoms of PAD did not undergo further testing and were deemed to be without PAD.
The patients were considered to have PAD if:
-
They had had a history of previous lower limb percutaneous transluminal angioplasty, with or without stent placement, or
-
They had had at least one instrumental and one clinical criterion among those listed in Table 2.
Table 2 Criteria for PAD definition in patients without a history of lower limb amputation, PTA or by-pass surgery
Such criteria were consistent with published literature [32,33,34,35].
The extent of PAD was determined by using the Fontaine classification, which defines four stages:
Stage I, asymptomatic; stage II, intermittent claudication; stage III, rest pain; stage IV ischemic ulcers or gangrene [36, 37].
Biochemical measurement
All patients enrolled underwent a blood test after an overnight fasting period of 8 h. For every patient, fasting glucose, triglycerides, total cholesterol, low and high-density lipoprotein, creatinine, aspartate aminotransferase, alanine aminotransferase, total bilirubin, alkaline phosphatase and complete blood count were determined. Renal function was assessed using estimated glomerular filtration rate (eGFR), which was calculated using the modification of diet in renal disease (MDRD) formula, as previously described [38]. Serum obtained and separated by centrifugation of blood samples was stored at − 80 °C before every measurement. Serum sortilin level were determined by a commercially available ELISA kit (RAB1709 SIGMA, Sigma-Aldrich) according to its protocol. The intra and inter-assay coefficients of variation were 3.5 and 10.5%, respectively. The sensitivity, defined as the mean ± 3 SD of the 0 standard, was calculated to be 0.15 pmol/mL. For each patient, the serum levels were measured twice and the results were averaged.
Statistical analysis
Demographic and clinical data between the groups were compared using Chi squared and t tests. Sortilin serum levels were compared through Mann–Whitney test. A log transformation was applied to not-normally distributed variables (fasting glucose, glycated hemoglobin, triglyceride, and sortilin levels) prior to performing further analysis. A multivariate stepwise logistic regression analysis was performed, adjusted for traditional risk factors and sortilin levels. The area under the receiver-operating characteristics (ROC) curve was calculated to test its predictive discrimination of PAD. All analyses were performed using the STATA version 11.0 for Windows (Statistics/Data Analysis, Stata Corporation, College Station, TX, USA). Statistical significance was established at P < 0.05.
Results
During the study period, 154 patients with a confirmed diagnosis of T2DM and not on statin therapy in the last 30 days, were included in the study. Eighty of the patients did not fulfill the criteria for a diagnosis of PAD, while the remaining 74 had a confirmed diagnosis of PAD or received a diagnosis of PAD during the index hospitalization. The demographic and clinical characteristics of the two groups are reported in Table 3. PAD patients had higher blood pressure values (P = 0.024), were more often smokers (P = 0.032) and were affected by CAD (defined as history of ischemic heart disease and/or previous coronary revascularization) more frequently (P = 0.031). There were no significant differences between groups regarding body mass index (BMI) (P = 0.52), median duration of diabetes (P = 0.97), fasting glucose (P = 0.75), glycated hemoglobin (P = 0.59), total cholesterol (TC) (P = 0.78), HDL-cholesterol (P = 0.67), LDL-cholesterol (P = 0.73) and triglyceride (P = 0.99). No statistical difference in terms of eGFR (P = 0.12), aspartate aminotransferase (P = 0.61), alanine aminotransferase (P = 0.45), total bilirubin (P = 0.33) and alkaline phosphatase (P = 0.56). Furthermore, there were no significant differences between groups regarding the complete blood count (Table 3). No statistical difference in terms of diabetic therapy was observed between the two patient groups. According to the Fontaine’s classification 36 patients were defined as stage II, 24 as stage III and 14 as stage IV.
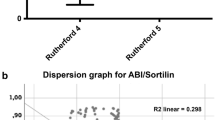
Sortilin concentration was higher among patients with PAD than among those without PAD (1.61 ± 0.54 ng/mL versus 0.67 ± 0.30 ng/mL, P < 0.01), as highlighted in Fig. 1. Moreover, when evaluating sortilin concentration according to patients’ functional status, a trend was evident, with higher levels of circulating sortilin in patients with more advanced disease (Fig. 2).
The multivariate logistic regression analysis showed that, after adjustments for cardiovascular risk factors, male gender, smoking, hypertension, hyperlipidemia, total cholesterol, HDL-cholesterol, LDL-cholesterol and sortilin levels were independent determinants for PAD occurrence in patients with T2DM (Table 4).
The ability of the area under the ROC curve based on sortilin levels to predict the presence of PAD in diabetic patients was 0.9133 (Fig. 3).
Discussion
The ABI is a very commonly used tool, easy to operate and it is able to identify PAD very effectively. When ABI is suggestive of PAD, however, we are often faced with a patient with an already advanced disease [39]. If we consider that PAD in diabetic patients can be even more aggressive and can manifest the symptoms later, the research for tools useful for an early diagnosis appears essential [40]. There are some potential biomarkers able to identify a subset of diabetic patients with PAD more prone to suffer major amputations; for instance, the tumor necrosis factor receptor 1 (TNFR1) has been associated with major amputation outcome [41]. Another possible biomarker for the presence of PAD in diabetic patients is represented by the high mobility group box 1 (HMGB1) which, together with the osteoprotegerin (OPG), has been associated with the presence of PAD in these patients [42]. Furthermore, also the fibroblast growth factor (FGF) 23 has been correlated with the presence of lower extremity atherosclerotic disease in diabetic patients [43]. In this scenario, sortilin may be of clinical interest as a simple, easy to measure biochemical marker for atherosclerotic disease. Numerous evidence suggests that sortilin is implicated in the pathogenesis of many inflammatory and metabolic diseases, including T2DM and atherosclerotic complications of diabetes [31]. In addition, sortilin has been shown to be an energetic regulator of lipid metabolism [44]. No definitive data about the role of sortilin in atherosclerosis and diabetes, however, are available. We have evidence that sortilin is decisive in the formation of atherosclerotic plaque and that therapeutic agents capable of reducing serum sortilin levels are able to improve atherosclerosis [30]. Sortilin-dependent uptake of LDL into macrophages represents an interesting mechanism of foam cell formation, the fundamental lesion of atherosclerotic disease [21]. There are data demonstrating that liver sortilin, however, could play a positive role in atherosclerosis, improving cholesterol metabolism and reducing LDL levels, which are fundamental players in the formation of atherosclerotic lesion [15]. Recent data have shown that a process dependent on autophagy degrades apoB that was diverted from the secretory pathway by sortilin and provides a mechanism contributing to the reduction of LDL cholesterol [45]. It is therefore possible that sortilin performs different functions depending on the district where it is produced, on the receptors which it binds and on the extracellular milieu where it is released. Oh and colleagues [26] have shown that this protein is associated with coronary artery disease and diabetes. To our knowledge, this is the first time that the sortilin serum concentration has been assessed as a potential biomarker for peripheral atherosclerotic artery disease of the lower limbs in a diabetic population. Our study shows a strong correlation between sortilin concentration and lower limb clinically significant atherosclerotic disease in T2DM patients. Previous experimental evidence has shown that sortilin is involved in the formation of atherosclerotic plaque. In particular, in a mouse model it has been shown that sortilin facilitates plaque formation by promoting the inflammatory setting [22]. It is therefore possible that in our population of diabetic patients, high sortilin values are responsible, at least in part, for atherosclerotic lesions of the lower limbs. An additional important data is that the levels of sortilin correlate with the PAD severity in diabetic patients, as if there were a dose-dependent relationship. Of particular interest, there is very little overlap between sortilin concentration in patients with PAD and in patients without PAD. The ROC curve also confirms that sortilin levels are able to predict the presence of PAD in our population of diabetic patients. If such result was confirmed, sortilin concentration could prove a biomarker with excellent sensitivity and specificity for peripheral artery disease in diabetic subjects.
A strength of this study is the fact that we enrolled only patients who were not on statin therapy. Given that statin therapy may affect sortilin concentration, our result, thus, are unlikely to be due to interference of pharmacological therapy. On the other hand, as many patients with diabetes or at high cardiovascular risk are more likely to be on statin therapy, our results need to be confirmed in a larger, more representative population. Statin therapy has been shown to reduce statin levels in patients with CAD [30]. Even circulating PCSK9 has been independently related to sortilin, and also their correlation is affected by the statin therapy [46]. Since our patient population was statin-free, the data we have documented are not affected by this aspect. At the same time, this finding could reinforce the hypothesis of using this biomarker to stratify patients, both from a diagnostic and a therapeutic point of view. It would be justified to assess PAD in diabetic patients with higher sortilin levels and it would be useful to start a more aggressive statin treatment in this subset of patients.
It is not possible to definitively clarify whether sortilin levels are a cause or effect of atherosclerosis, or even both, in a sort of vicious circle. The earlier studies on sortilin highlighted its causative role in atherosclerotic disease, mainly due to the action of intracellular sortilin. In fact, in the study by Musunuru and colleagues [15], protective SNP was associated with a reduced intracellular concentration of sortilin and it was this intracellular action that is thought as associated with atherosclerosis. It has been later shown, however, that sortilin is actively secreted by activated platelet and may play a role in foam-cell formation. Thus, circulating sortilin concentration may also be a consequence of atherosclerosis.
A limitation of our study is that its cross-sectional nature is not able to establish causal relationship between the findings. Even so, our result lend support to the hypothesis that sortilin actions in extra-hepatic tissue are important in the atherosclerosis physiopathology. A further limitation is the small number of patients included in the study, due to the particular condition that required the presence of diabetes and the absence of statin treatment. Another major limitation of our study is the lack of prospective data. We didn’t aim, however, to investigate sortilin as a maker for increased risk, we tested it as a marker for active disease. A further limitation of our study is in that we chose to define PAD as a clinically apparent disease. In fact, to overcome this limitation a prospective study would be needed. We believe that our present result may lay the foundation for such a subsequent prospective study.
Conclusions
We demonstrated that circulating sortilin levels are associated with PAD in diabetic patients, that sortilin levels correlate with disease severity and that, therefore, sortilin is a promising marker for PAD in diabetic patients. Furthermore, in addition to risk factor-based validated scores, sortilin may help clinicians to better stratify atherosclerotic risk in diabetic patients. Further studies to confirm this hypothesis are needed and warranted.
Abbreviations
- ABI:
-
ankle-brachial index
- BMI:
-
body mass index
- CT:
-
computed tomography
- CAD:
-
coronary artery disease
- eGFR:
-
estimated glomerular filtration rate
- LDL:
-
low-density lipoprotein
- LL-PAD:
-
lower limb PAD
- MDRD:
-
modification of diet in renal disease
- PAD:
-
peripheral artery disease
- ROC:
-
receiver-operating characteristics
- R:
-
receptor
- TC:
-
total cholesterol
- T2DM:
-
type 2 diabetes mellitus
- VLDL:
-
very low-density lipoprotein
References
Petersen CM, Nielsen MS, Nykjaer A, Jacobsen L, Tommerup N, Rasmussen HH, et al. Molecular identification of a novel candidate sorting receptor purified from human brain by receptor-associated protein affinity chromatography. J Biol Chem. 1997;272:3599–605.
Samani NJ, Erdmann J, Hall AS, Hengstenberg C, Mangino M, Mayer B, et al. Genomewide association analysis of coronary artery disease. N Engl J Med. 2007;357:443–53.
Kathiresan S, Manning AK, Demissie S, D’Agostino RB, Surti A, Guiducci C, et al. A genome-wide association study for blood lipid phenotypes in the Framingham Heart Study. BMC Med Genet. 2007;8(Suppl 1):S17.
Kathiresan S, Melander O, Guiducci C, Surti A, Burtt NP, Rieder MJ, et al. Six new loci associated with blood low-density lipoprotein cholesterol, high-density lipoprotein cholesterol or triglycerides in humans. Nat Genet. 2008;40:189–97.
Willer CJ, Sanna S, Jackson AU, Scuteri A, Bonnycastle LL, Clarke R, et al. Newly identified loci that influence lipid concentrations and risk of coronary artery disease. Nat Genet. 2008;40:161–9.
Wallace C, Newhouse SJ, Braund P, Zhang F, Tobin M, Falchi M, et al. Genome-wide association study identifies genes for biomarkers of cardiovascular disease: serum urate and dyslipidemia. Am J Hum Genet. 2008;82:139–49.
Kathiresan S, Willer CJ, Peloso GM, Demissie S, Musunuru K, Schadt EE, et al. Common variants at 30 loci contribute to polygenic dyslipidemia. Nat Genet. 2009;41:56–65.
Aulchenko YS, Ripatti S, Lindqvist I, Boomsma D, Heid IM, Pramstaller PP, et al. Loci influencing lipid levels and coronary heart disease risk in 16 European population cohorts. Nat Genet. 2009;41:47–55.
Chasman DI, Paré G, Mora S, Hopewell JC, Peloso G, Clarke R, et al. Forty-three loci associated with plasma lipoprotein size, concentration, and cholesterol content in genome-wide analysis. PLoS Genet. 2009;5:e1000730.
Teslovich TM, Musunuru K, Smith AV, Edmondson AC, Stylianou IM, Koseki M, et al. Biological, clinical and population relevance of 95 loci for blood lipids. Nature. 2010;466:707–13.
Myocardial Infarction Genetics Consortium, Kathiresan S, Voight BF, Purcell S, Musunuru K, Ardissino D, et al. Genome-wide association of early-onset myocardial infarction with single nucleotide polymorphisms and copy number variants. Nat Genet. 2009;41:334–41.
Schunkert H, König IR, Kathiresan S, Reilly MP, Assimes TL, Holm H, et al. Large-scale association analysis identifies 13 new susceptibility loci for coronary artery disease. Nat Genet. 2011;43:333–8.
Kjolby M, Andersen OM, Breiderhoff T, Fjorback AW, Pedersen KM, Madsen P, et al. Sort1, encoded by the cardiovascular risk locus 1p13.3, is a regulator of hepatic lipoprotein export. Cell Metab. 2010;12:213–23.
Linsel-Nitschke P, Heeren J, Aherrahrou Z, Bruse P, Gieger C, Illig T, et al. Genetic variation at chromosome 1p13.3 affects sortilin mRNA expression, cellular LDL-uptake and serum LDL levels which translates to the risk of coronary artery disease. Atherosclerosis. 2010;208:183–9.
Musunuru K, Strong A, Frank-Kamenetsky M, Lee NE, Ahfeldt T, Sachs KV, et al. From noncoding variant to phenotype via SORT1 at the 1p13 cholesterol locus. Nature. 2010;466:714–9.
Strong A, Rader DJ. Sortilin as a regulator of lipoprotein metabolism. Curr Atheroscler Rep. 2012;14:211–8.
Strong A, Ding Q, Edmondson AC, Millar JS, Sachs KV, Li X, et al. Hepatic sortilin regulates both apolipoprotein B secretion and LDL catabolism. J Clin Invest. 2012;122:2807–16.
Herda S, Raczkowski F, Mittrücker HW, Willimsky G, Gerlach K, Kühl AA, et al. The sorting receptor sortilin exhibits a dual function in exocytic trafficking of interferon-γ and granzyme A in T cells. Immunity. 2012;37:854–66.
Yabe-Wada T, Matsuba S, Takeda K, Sato T, Suyama M, Ohkawa Y, et al. TLR signals posttranscriptionally regulate the cytokine trafficking mediator sortilin. Sci Rep. 2016;6:26566.
Ogawa K, Ueno T, Iwasaki T, Kujiraoka T, Ishihara M, Kunimoto S, et al. Soluble sortilin is released by activated platelets and its circulating levels are associated with cardiovascular risk factors. Atherosclerosis. 2016;249:110–5.
Patel KM, Strong A, Tohyama J, Jin X, Morales CR, Billheimer J, et al. Macrophage sortilin promotes LDL uptake, foam cell formation, and atherosclerosis. Circ Res. 2015;116:789–96.
Mortensen MB, Kjolby M, Gunnersen S, Larsen JV, Palmfeldt J, Falk E, et al. Targeting sortilin in immune cells reduces proinflammatory cytokines and atherosclerosis. J Clin Invest. 2014;124:5317–22.
Li J, Matye DJ, Li T. Insulin resistance induces posttranslational hepatic sortilin 1 degradation in mice. J Biol Chem. 2015;290:11526–36.
Chamberlain JM, O’Dell C, Sparks CE, Sparks JD. Insulin suppression of apolipoprotein B in McArdle RH7777 cells involves increased sortilin 1 interaction and lysosomal targeting. Biochem Biophys Res Commun. 2013;430:66–71.
Bi L, Chiang JYL, Ding W-X, Dunn W, Roberts B, Li T. Saturated fatty acids activate ERK signaling to downregulate hepatic sortilin 1 in obese and diabetic mice. J Lipid Res. 2013;54:2754–62.
Oh TJ, Ahn CH, Kim BR, Kim KM, Moon JH, Lim S, et al. Circulating sortilin level as a potential biomarker for coronary atherosclerosis and diabetes mellitus. Cardiovasc Diabetol. 2017;16:1–7.
American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care. 2016. https://doi.org/10.2337/dc16-S001.
Ohashi K, Shibata R, Murohara T, Ouchi N. Role of anti-inflammatory adipokines in obesity-related diseases. Trends Endocrinol Metab. 2014;25:348–55.
Strong A, Patel K, Rader DJ. Sortilin and lipoprotein metabolism: making sense out of complexity. Curr Opin Lipidol. 2014;25:350–7.
Nozue T, Hattori H, Ogawa K, Kujiraoka T, Iwasaki TMI. Effects of statin therapy on plasma proprotein convertase subtilisin/kexin type 9 and sortilin levels in statin-naive patients with coronary artery disease. J Atheroscler Thromb. 2016;1:848–56.
Goettsch C, Kjolby M, Aikawa E. Sortilin and its multiple roles in cardiovascular and metabolic diseases. Arterioscler Thromb Vasc Biol. 2017. https://doi.org/10.1161/ATVBAHA.117.310292.
Bosch J, Eikelboom JW, Connolly SJ, Bruns NC, Lanius V, Yuan F, et al. Rationale, design and baseline characteristics of participants in the cardiovascular outcomes for people using anticoagulation strategies (COMPASS) trial. Can J Cardiol. 2017;33:1027–35.
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377:1319–30.
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 2017;135:e686–725.
Aboyans V, Ricco J-B, Bartelink M-LEL, Björck M, Brodmann M, Cohnert T, et al. ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal. Eur Heart J. 2017;2018(39):763–816.
Becker F. Exploration of arterial function with noninvasive technics. Results in chronic arterial occlusive disease of the lower limbs according to Leriche and Fontaine classification. Int Angiol. 1985;4:311–22.
Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. Overview of classification systems in peripheral artery disease. Semin Interv Radiol. 2014;31:378–88.
Choi SW, Kim HY, Lee YH, Ryu SY, Kweon SS, Rhee JA, et al. EGFR is associated with subclinical atherosclerosis independent of albuminuria: the Dong-gu study. Atherosclerosis. 2010;212:616–67.
American Diabetes Association. Peripheral artery disease in people with diabetes. Diabetes Care. 2003;26:3333–41.
Nativel M, Potier L, Alexandre L, Baillet-Blanco L, Ducasse E, Velho G, et al. Lower extremity arterial disease in patients with diabetes: a contemporary narrative review. Cardiovasc Diabetol. 2018;17:138.
Schneider F, Saulnier PJ, Gand E, Desvergnes M, Lefort N, Thorin E, et al. Influence of micro- and macro-vascular disease and Tumor Necrosis Factor Receptor 1 on the level of lower-extremity amputation in patients with type 2 diabetes. Cardiovasc Diabetol. 2018;17:81.
Giovannini S, Tinelli G, Biscetti F, Straface G, Angelini F, Pitocco D, et al. Serum high mobility group box-1 and osteoprotegerin levels are associated with peripheral arterial disease and critical limb ischemia in type 2 diabetic subjects. Cardiovasc Diabetol. 2017;16:99.
He X, Hu X, Ma X, Su H, Ying L, Peng J, et al. Elevated serum fibroblast growth factor 23 levels as an indicator of lower extremity atherosclerotic disease in Chinese patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2017;16:77.
Hagita S, Rogers MA, Pham T, Wen JR, Mlynarchik AK, Aikawa M, et al. Transcriptional control of intestinal cholesterol absorption, adipose energy expenditure and lipid handling by Sortilin. Sci Rep. 2018;8:9006.
Amengual J, Guo L, Strong A, Madrigal-Matute J, Wang H, Kaushik S, et al. Autophagy is required for sortilin-mediated degradation of apolipoprotein B100. Circ Res. 2018;122:568–82.
Hu D, Yang Y, Peng DQ. Increased sortilin and its independent effect on circulating proprotein convertase subtilisin/kexin type 9 (PCSK9) in statin-naive patients with coronary artery disease. Int J Cardiol. 2017;227:61–5.
Authors’ contributions
FB, NB and FS participated in the design of the study, performed data analysis and reviewed the manuscript. FA and EN carried out the immunoassays. DP, AS and MF participated in the design of the study and performed statistical analyses. FB, RL and AF conceived the study, participated in its design and coordination and helped draft the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
All authors have read the paper and agree that it can be published.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Fondazione Policlinico Universitario A. Gemelli IRCCS and adhered to the principles of the Declaration of Helsinki. All the individuals agreed to participate in the study and gave informed consent.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Biscetti, F., Bonadia, N., Santini, F. et al. Sortilin levels are associated with peripheral arterial disease in type 2 diabetic subjects. Cardiovasc Diabetol 18, 5 (2019). https://doi.org/10.1186/s12933-019-0805-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-019-0805-5