Abstract
Background
Delayed cerebral ischemia is one of the leading causes of death and disability in patients with subarachnoid hemorrhage (SAH). Transluminal balloon angioplasty (TBA) is a therapeutic option for vasospasms affecting proximal intracranial arteries.
Methods
Aim of this study was to report our experience using the Scepter C balloon catheter in the treatment of cerebral vasospasms due to SAH and evaluate the postprocedural result with the iFlow tool. We reviewed cases of patients treated at our hospital from 2014 to 2018. Patients were screened with transcranial doppler sonography (TCD) and multimodal computed tomography. In case of significant vasospasms, patients were transferred to the angiography suite and treated. We used the iFlow tool to quantify and evaluate the angiographic results by measuring and comparing peak density values on angiograms before and after the mechanical dilation.
Results
The use of the Scepter C balloon catheter was feasible in all cases. Vasospasms of the anterior cerebral artery were treated in ten cases. We didn’t observe complications or vasospasm recurrences of the treated arteries. The temporal difference between distal vessels and the proximal reference vessel was significantly reduced from a mean of 53%, prior to dilatation, to 26% after the treatment. The difference between pre-dilatation and post-dilatation values was statistically significant for the anterior circulation at the proximal as well as at the distal vessels.
Conclusions
We successfully treated endovascularly patients suffering from cerebral vasospasms refractory to medical treatment using the Scepter C balloon catheter. We didn’t observe any complications. The therapeutic effect could be easily and reliably assessed with the iFlow tool.
Similar content being viewed by others
Background
Cerebral vasospasm is defined as the narrowing of large or small intracranial arteries after a subarachnoid hemorrhage (SAH). Angiographic vasospasms are very common in patients with a ruptured intracranial aneurysm, with an incidence of 50–90% [1, 2]. Delayed ischemic neurological deficit or symptomatic vasospasm is one of the leading causes of death and disability in these patients and occurs in 20–25% of them [3, 4]. Although the mechanism of nimodipine’s beneficial effect is not completely clear, in eight randomized clinical trials nimodipine has shown to have a statistically significant effect on the outcome [5,6,7,8,9,10,11]. Thus, it is routinely used as a preventive measure as well as a treatment for cerebral vasospasms.
Transluminal balloon angioplasty (TBA) is a therapeutic option for symptomatic vasospasms in proximal vessels after SAH. The results of a recent international survey by Hollingworth et al. demonstrated that 83% of non-United States (U.S.) physicians and 91% of U.S. physicians performed angioplasty for treatment of vasospasms. Despite the universally accepted efficacy of angioplasty in patients with cerebral vasospasm, only 3% of U.S. responders and 6% of non-U.S. responders used it as a first-line endovascular therapy [12].
Multiple studies have reported a reversal of neurological deficits after angioplasty in 30–70% of patients in whom the medical treatment failed [13,14,15,16]. However, complications including wire perforation, vessel dissection and ischemic stroke have been reported. Nevertheless, endovascular therapies, techniques as well as materials have been evolved since the first report of balloon catheter usage [17].
We report our experience with the dual lumen, compliant balloon catheter in the endovascular treatment of vasospasms after SAH. We used a commercially available software to retrospectively assess the treatment efficacy of angioplasty comparing time-density curves before and after treatment.
Methods
Patient selection
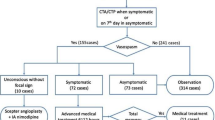
We reviewed patients from our center from 2014 to 2018 who suffered from vasospasms after cerebral aneurysm rupture and were treated with the Scepter C balloon catheter. All SAH-patients underwent screening with transcranial doppler sonography (TCD) on a daily basis. A mean blood flow velocity (BFV) > 120 cm/sec was defined as TCD-confirmed vasospasm [18]. We performed computed tomography angiography (CTA) and computed tomography perfusion (CTP) routinely in the acute phase (3rd - 5th day after aSAH) and/or in case of clinical deterioration. In intubated patients, we performed a CT-imaging on the 3rd and 7th day or in the event of significantly elevated TCD velocities (higher as 120 cm/s or increase of 50 cm/sec within 24 h).
Angioplasty technique
In the case of perfusion deficits, notable acceleration of the TCD velocities or clinical vasospasms, and after exclusion of a large cerebral infarct in CT, patients were transferred to the angiography suite. An experienced neuroradiologist (more than 5 years of experience) performed a TBA via a transfemoral approach in cases of significant vasospasms of proximal vessels. We performed a diagnostic angiography after the placement of a 5F or 6F sheath in the femoral artery to elucidate which vessels should be treated. The images were acquired after injection of 8 mL of contrast agent (Imeron 400, Bracco, Konstanz, Germany) manually by hand at a flow rate of 4 mL/s for 2 s.
If a TBA was necessary, we placed proximally a heparinized saline-flushed 5 or 6 French guide catheter and dilated the vasospastic vessels with the Scepter C balloon catheter (Microvention Tustin, California, USA) (Figs. 1 and 2). The use of additional intra-arterial nimodipine was based on the discretion of the interventionalist and was administered either before or after the angioplasty. All interventions were performed under general anesthesia; patients without contraindications were extubated directly after the procedure in the angiography suite and underwent neurologic examination. Indicators for complications related to the procedure were the angiographic images after the angioplasty and the clinical examination of the patients, who were intubated only for the procedure and extubated immediately after that. According to our procedural standard patients underwent a flat-detector computed tomography at the end of the intervention in order to exclude a new bleeding.
Angiographic and color-coded images processed with the iFlow tool of a 47-year-old female patient. Rupture and immediate coiling of a ACom-aneurysm. After 4 days significant vasospasms of the left and right MCA and Carotis-T arteries are depicted. Distal ICA and right M1 segment, left M1 and M2 were successfully treated with the Scepter C balloon catheter. An angioplasty of ACA wasn’t initially performed because of the recent coiling. Temporal delay between proximal and distal segments was significantly reduced after treatment
We transferred patients to the intensive care unit, where they were treated for 14 days or longer if needed. We were able to acquire the follow-up mRS at 3 months in 11 patients.
Analysis
We retrospectively analyzed our data and postprocessed hemodynamic parameters of angiograms before and after the TBA in a dedicated image reconstruction workstation (syngo X Workplace; Siemens Healthcare, Forchheim, Germany) using quantitative DSA with syngo iFlow software (Siemens). This software provides a color-coded single image by calculating and displaying time-intensity curves for each image pixel [19]. We placed 6 regions of interest (ROI) in two projection angiograms in order to assess the hemodynamic parameters in proximal arteries (middle cerebral artery [MCA] and anterior cerebral artery [ACA], M1 and A1 segment), as well as in distal arteries (postcentral branch of MCA and pericallosal artery, M4- and A2 segment). For the posterior circulation, we used 3 ROIs in the distal basilar artery, in the proximal posterior cerebral artery (P1 segment) and in the distal posterior cerebral artery (P2 segment). Reference vessels were the extradural or cavernous internal carotid artery for the anterior circulation and the extradural vertebral artery for the posterior circulation where no vasospasms were noticed. The hemodynamic parameters were processed with the aforementioned software and were analyzed with the MedCalc statistical package (MedCalc Statistical Software version 17.7, MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2017). The significance level for all tests was set to α = 0.05.
Results
We treated nineteen SAH-patients (average age 51, ±11.6 years, eleven women) suffering from SAH-related vasospasms with the Scepter C balloon catheter. Because of motion artifacts the angiograms of two patients could not be processed with the abovementioned software and these patients were excluded from the evaluation. We retrospectively analyzed 22 cases (procedures) of the seventeen included patients.
Three patients suffered from rupture of an aneurysm of the intradural internal carotid artery (6 cases), two patients from rupture of an aneurysm of the MCA (2 cases), five patients suffered from the rupture of an aneurysm of the anterior communicating artery (6 angioplasty cases), two patients from rupture of an aneurysm of the basilar artery (2 cases), two patients from rupture of an aneurysm of the posterior inferior cerebellar artery (3 cases), and one patient suffered from the rupture of an aneurysm of the vertebral artery (1 case). One patient suffered from SAH after the endovascular therapy of an aneurysm of the basilar artery (coil-embolization) and one patient suffered from SAH and vasospasms but no aneurysm or vessel malformation were detected on initial or follow-up digital subtraction angiography (DSA) (Table 1).
SAH Fisher grade III was depicted in four patients and in thirteen patients (18 cases) grade IV SAH. Five patients (8 cases) suffered from SAH Hunt and Hess grade I, two patients (2 cases) from grade II, three patients (3 cases) from grade III, three (3) from grade IV and in four patients an SAH Hunt und Hess (6) grade V was diagnosed.
Ten patients (14 cases) were treated by a neuroradiologist of our institute with coil embolization. In six patients the ruptured aneurysm was clipped. In 1 case, clipping was performed after incomplete coil embolization.
The TBA was performed on median 8th day (IQR 7–10.25) after aneurysm rupture. We always used the Scepter C balloon catheter, which is provided in 3 sizes. We used 11 times the 4 × 15 mm balloon catheter, 7 times the 4 × 10 mm and 6 times the 4 × 20 mm. The distal internal carotid artery (incl. Carotid T) was dilated in 13 cases, the A1 segment in 9 cases, the M1 segment in 21 cases, the M2 segment in 3 cases, the A2 segment in 1 case, the distal vertebral artery in 3 cases and the basilar artery in 4 cases.
In 15 out of 22 cases, we decided on the intra-arterial use of a dihydropyridine calcium channel blocker (nimodipine) and in 1 case, opium alkaloid antispasmodic drug (papaverine) was administered. Intra-arterial doses ranged from 1.8 to 20.0 mg per treatment session.
There was a decrease of the percental temporal difference between distal vessels and the proximal reference vessel from a median of 25% (IQR 14–42) prior to dilatation, to 13% (IQR 0–22) after treatment of the vasospasm. Using the Wilcoxon-test, we noticed a statistically significant reduction of the temporal difference for the anterior circulation at proximal and at distal vessels (A1-segment P < 0.001, M1-segment P < 0.001, A2-segment P < 0.001, M3-segment P = 0.002). The statistical analysis of the hemodynamic values of the posterior circulation did not show any significant reduction (P = 0.54); however, all flow parameters showed a mild to moderate reduction of the percental temporal difference between the reference vessel and the vessel of choice after the TBA, ranging from a median of 34% (SD 14) to a median of 28% (IQR 16–35).
In 14 cases, we were able to compare the TCD values before and after the intervention. We observed a statistical significant decrease of the medial TCD values (P < 0.001, Wilcoxon-test). In 7 cases we extubated the patients in the angiography suite and in 5 of them we observed a postinterventional improvement of neurological deficits. That was considered as clinical improvement due to angioplasty. In the other 15 cases the patients remained intubated (Table 2).
Discussion
The delayed cerebral ischemia (DCI) is one of leading causes of mortality or morbidity in patients with ruptured cerebral aneurysms and consecutive SAH. Due to the improvement of the survival among hospitalized patients, mortality has halved in the last two decades; however, delayed cerebral ischemia remains one of the leading preventable reasons of poor outcome [20,21,22,23].
The endovascular treatment of vasospasms includes pharmacological and mechanical dilatation. Intraarterial infusion of papaverine, nimodipine, nicardipine or verapamil has been used with various outcomes [24]. Their limitation is the short duration of benefit. A moderate clinical improvement, a reversal of delayed ischemic neurological deficits and an angiographic improvement as high as 100% has been reported after a TBA (Table 3) [24,25,26].
Although it is considered that the angioplasty is only effective at the segment of the vessel which was dilated, our results of iFlow values showed that there was a statistical significant augmentation of the hemodynamic parameters in proximal dilated arteries as well as in their distal segments. Some authors noticed that the recurrence of a symptomatic vasospasm or the depiction of vasospasm in an adjacent, distal arterial segment could be also possible [1, 27, 28]. In our collective, only two patients with SAH Fisher grade III underwent further angioplasty of more distal segment of the same vessel; nevertheless, we observed no recurrence of vasospasm of the already dilated segments or of adjacent segments. (Figs. 1 and 2).
We noticed no complications related to the use of the Scepter C balloon catheter, which is in line with findings of others [29]. Nevertheless, the comparison with the initial angiographic imaging for the estimation of the real vessel size is very important to prevent a rupture or perforation due to overinflation. This balloon catheter showed improved feasibility and trackability compared to the commonly used single-lumen over the wire balloon catheters. We could reach and treat the affected vessels in all cases. The angioplasty of the M2 or A2 segment was also possible with a 0.014 in. hydrophilic microwire (Fig. 3). This catheter is provided in 3 sizes with a constant diameter of 4 mm. A smaller diameter (e.g. 3 mm) would be even better in some cases.
The syngo iFlow software is not widely used in the clinical praxis. It provides the visualization of a complete DSA run in a color-coded single image in push-button approach (Figs. 1 and 2). Clinicians can evaluate the inflow and outflow of contrast agent in regions of interest. Measures with this software are feasible, easy, quick and reliable and offer an immediate evaluation of results of the angioplasty.
There are no guidelines for the interventional treatment of cerebral vasospasms in the literature [30]. In our experience, the intra-arterial treatment of SAH-related vasospasms seems safe and efficient. In many cases, TBA is performed after the detection of vasospasm-related infarction or severe stenosis of proximal arteries. It remains to be proved with a randomized prospective trial, if TBA should be applied earlier for the treatment of vasospasms.
The primary limitation of our study is the retrospective character and the highly selected group of patients. Another limitation is the absence of an independent core lab. We extracted data from a prospectively collected database and consecutive patients were included in our analysis. All interventions were performed only by experienced neuroradiologists. The fact that we did not observe any complications does not mean that the use of this catheter is accompanied with no risk.
Conclusions
The aim of this retrospective study is to report our experience with the Scepter C balloon-catheter for the treatment of cerebral vasospasms after SAH and the postprocedural result evaluation with the above-mentioned software. This is the first study, which confirms that the angioplasty of proximal arteries of circle of Willis is effective also at the peripheral branches. The use of the above-mentioned balloon catheter showed improved feasibility and trackability and was not associated with complications. Additionally, we find the described software useful and reliable for the purposes of decision making. Since 2015, we use it periinterventional during a TBA to evaluate the flow of proximal and distal arteries after the angioplasty.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACA:
-
Anterior cerebral artery
- ACM:
-
Middle cerebral artery
- BFV:
-
Blood flow velocity
- CTA:
-
Computed tomography angiography
- CTP:
-
Computed tomography perfusion
- DCI:
-
Delayed cerebral ischemia
- DSA:
-
Digital subtraction angiography
- ROI:
-
Region of interest
- SAH:
-
Subarachnoid hemorrhage
- TBA:
-
Transluminal balloon angioplasty
- TCD:
-
Transcranial doppler sonography
References
Findlay JM, Nisar J, Darsaut T. Cerebral vasospasm: a review. Can J Neurol Sci. 2016;43(1):15–32.
Dorsch NW, King MT. A review of cerebral vasospasm in aneurysmal subarachnoid haemorrhage part I: incidence and effects. J Clin Neurosci. 1994;1(1):19–26.
Murayama Y, Malisch T, Guglielmi G, Mawad ME, Vinuela F, Duckwiler GR, et al. Incidence of cerebral vasospasm after endovascular treatment of acutely ruptured aneurysms: report on 69 cases. J Neurosurg. 1997;87(6):830–5.
Charpentier C, Audibert G, Guillemin F, Civit T, Ducrocq X, Bracard S, et al. Multivariate analysis of predictors of cerebral vasospasm occurrence after aneurysmal subarachnoid hemorrhage. Stroke. 1999;30(7):1402–8.
Allen GS, Ahn HS, Preziosi TJ, Battye R, Boone SC, Chou SN, et al. Cerebral arterial spasm--a controlled trial of nimodipine in patients with subarachnoid hemorrhage. N Engl J Med. 1983;308(11):619–24.
Barker FG 2nd, Ogilvy CS. Efficacy of prophylactic nimodipine for delayed ischemic deficit after subarachnoid hemorrhage: a metaanalysis. J Neurosurg. 1996;84(3):405–14.
Mee E, Dorrance D, Lowe D, Neil-Dwyer G. Controlled study of nimodipine in aneurysm patients treated early after subarachnoid hemorrhage. Neurosurgery. 1988;22(3):484–91.
Ohman J, Heiskanen O. Effect of nimodipine on the outcome of patients after aneurysmal subarachnoid hemorrhage and surgery. J Neurosurg. 1988;69(5):683–6.
Petruk KC, West M, Mohr G, Weir BK, Benoit BG, Gentili F, et al. Nimodipine treatment in poor-grade aneurysm patients. Results of a multicenter double-blind placebo-controlled trial. J Neurosurg. 1988;68(4):505–17.
Philippon J, Grob R, Dagreou F, Guggiari M, Rivierez M, Viars P. Prevention of vasospasm in subarachnoid haemorrhage. A controlled study with nimodipine. Acta Neurochir. 1986;82(3–4):110–4.
Pickard JD, Murray GD, Illingworth R, Shaw MD, Teasdale GM, Foy PM, et al. Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. BMJ. 1989;298(6674):636–42.
Hollingworth M, Chen PR, Goddard AJ, Coulthard A, Soderman M, Bulsara KR. Results of an international survey on the investigation and endovascular Management of Cerebral Vasospasm and Delayed Cerebral Ischemia. World Neurosurg. 2015;83(6):1120–6 e1121.
Eskridge JM, Newell DW, Winn HR. Endovascular treatment of vasospasm. Neurosurg Clin N Am. 1994;5(3):437–47.
Coyne TJ, Montanera WJ, Macdonald RL, Wallace MC. Percutaneous transluminal angioplasty for cerebral vasospasm after subarachnoid hemorrhage. Can J Surg. 1994;37(5):391–6.
Bejjani GK, WOF B, Olan WJ, Sekhar LN. The efficacy and safety of angioplasty for cerebral vasospasm after subarachnoid hemorrhage. Neurosurgery. 1998;42(5):979–86 discussion 986-977.
Fujii Y, Takahashi A, Yoshimoto T. Effect of balloon angioplasty on high grade symptomatic vasospasm after subarachnoid hemorrhage. Neurosurg Rev. 1995;18(1):7–13.
Teitelbaum GP, Larsen DW, Zelman V, Lysachev AG, Likhterman LB. A tribute to Dr. Fedor a. Serbinenko, founder of endovascular neurosurgery. Neurosurgery. 2000;46(2):462–9 discussion 469-470.
Gonzalez NR, Boscardin WJ, Glenn T, Vinuela F, Martin NA. Vasospasm probability index: a combination of transcranial doppler velocities, cerebral blood flow, and clinical risk factors to predict cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2007;107(6):1101–12.
Yamamoto K, Nakai G, Azuma H, Narumi Y. Novel software-assisted hemodynamic evaluation of pelvic flow during Chemoperfusion of pelvic arteries for bladder cancer: double- versus single-balloon technique. Cardiovasc Intervent Radiol. 2016;39(6):824–30.
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL. The international cooperative study on the timing of aneurysm surgery. Part 1: overall management results. J Neurosurg. 1990;73(1):18–36.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A. Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke. 1994;25(7):1342–7.
Proust F, Hannequin D, Langlois O, Freger P, Creissard P. Causes of morbidity and mortality after ruptured aneurysm surgery in a series of 230 patients. The importance of control angiography. Stroke. 1995;26(9):1553–7.
Lovelock CE, Rinkel GJ, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage: population-based study and systematic review. Neurology. 2010;74(19):1494–501.
Zwienenberg-Lee M, Hartman J, Rudisill N, Muizelaar JP. Endovascular management of cerebral vasospasm. Neurosurgery. 2006;59(5 Suppl 3):S139–47 discussion S133–113.
Jestaedt L, Pham M, Bartsch AJ, Kunze E, Roosen K, Solymosi L, et al. The impact of balloon angioplasty on the evolution of vasospasm-related infarction after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2008;62(3):610–7 discussion 610-617.
Hoh BL, Ogilvy CS. Endovascular treatment of cerebral vasospasm: transluminal balloon angioplasty, intra-arterial papaverine, and intra-arterial nicardipine. Neurosurg Clin N Am. 2005;16(3):501–16 vi.
Santillan A, Knopman J, Zink W, Patsalides A, Gobin YP. Transluminal balloon angioplasty for symptomatic distal vasospasm refractory to medical therapy in patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2011;69(1):95–101 discussion 102.
Tekle WG, Chaudry SA, Hassan AE, Qaiser H, Grigoryan M, Rodriguez GJ, et al. High risk of new episode of symptomatic vasospasm in unaffected arteries in subarachnoid hemorrhage patients receiving targeted endovascular treatment for symptomatic focal vasospasm. Neurocrit Care. 2014;20(3):399–405.
John S, Spiotta AM, Turner RM, Chaudry MI, Turk AS, Hui F. Initial experience with the coaxial dual-lumen scepter C balloon catheter for endovascular management of cerebral vasospasm from subarachnoid hemorrhage. J Neurointerventional Surg. 2014;6(2):125–8.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–37.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. We acknowledge support by the Open Access Publication Funds of the Göttingen University.
Author information
Authors and Affiliations
Contributions
IT: designed the study and was involved in the acquisition of the data, analyzed raw data, performed statistics, drafted and finalized the manuscript and approved the manuscript before submission. VM: was involved in the acquisition of the data, contributed to the manuscript and approved the manuscript before submission. KS: revised and contribute to the manuscript and approved the manuscript before submission. DM: revised and contributed to the manuscript and approved the manuscript before submission. DB: was involved in the acquisition of the data, contributed to the manuscript and approved the manuscript before submission. VR: contributed to the manuscript and approved the manuscript before submission. MK: contributed to the manuscript and approved the manuscript before submission. MNP: designed the study, performed statistics, contributed to, finalized the manuscript, and approved the manuscript before submission. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee from University medical center Goettingen approved that all procedures performed in this study were in accordance with the ethical standards of our institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The data were prospectively collected for a previous research project, which was approved by the local ethics committee (Number 22/11/12). Informed consent was waived, given the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The Department of Neuroradiology has a research agreement with Siemens Medical Solutions, Forchheim, Germany. DB has received speaker’s honoraria from Stryker, Penumbra and Acandis. VR has received fees from B-Braun, Aesculap. MNP has received fees as consultant or lecturer from Siemens, Penumbra and Stryker.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tsogkas, I., Malinova, V., Schregel, K. et al. Angioplasty with the scepter C dual lumen balloon catheter and postprocedural result evaluation in patients with subarachnoid hemorrhage related vasospasms. BMC Neurol 20, 260 (2020). https://doi.org/10.1186/s12883-020-01792-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-020-01792-3