Abstract
Background
Activated Vitamin D has anti-inflammatory properties and adequate 25-hydroxyvitamin D [25(OH)D] concentrations may be important for neurocognitive function and protection against neurologic injury. We examined whether mid-life 25(OH) D concentrations were associated with later-life performance on neuropsychological testing, functional ability, depressive symptoms, and incident dementia.
Methods
We studied 13,039 white and black ARIC participants who had serum 25(OH) D measured mid-life at visit 2 (1990–1992). Over the next ~ 20 years through visit 5 (2011–2013), participants underwent 3 additional in-person visits, annual telephone calls, and hospitalization surveillance. An extensive battery of neuropsychological outcomes were assessed at visit 5 using standardized protocols. Incident dementia was ascertained through a formal algorithm that included data from in-person cognitive testing, telephone interviews, hospital discharge codes, and death certificate codes. Diagnoses of dementia were adjudicated by expert clinician committee. For the primary cognitive analyses, we imputed for missing covariates and outcomes and used linear regression to evaluate non-concurrent cross-sectional associations of mid-life 25(OH) D (visit 2) with late-life neuropsychological outcomes (visit 5). We also used Cox regression models to examine associations of mid-life 25(OH) D and incident dementia.
Results
In mid-life, the mean (SD) age of participants was 57 (6) years, 57% were women, and 24% black. Mean (SD) 25(OH) D was 24.3 (8.6) ng/mL; 33% had deficient (< 20 ng/mL), 44% intermediate (20- < 30 ng/mL), and 23% sufficient (≥30 ng/mL) 25(OH) D concentrations. Association between mid-life 25(OH) D and late-life performance on neuropsychological testing were mostly null. There was no significant association with functional ability or depressive symptoms. Results were similar in a sensitivity analysis using complete-case data (no imputation). However, after a median follow-up of 20 years, low 25(OH) D concentrations were associated with increased risk for incident dementia (p = 0.01 for trend across categories), with HR of 1.26 (95% CI 1.06, 1.49) for participants with deficient 25(OH) D, compared to sufficient concentrations.
Conclusion
In this community cohort, mid-life serum 25(OH) D concentrations were associated with incident dementia but not with performance on neuropsychological testing, functional ability, or depressive symptoms, 20 years later. Whether serum 25(OH) D concentrations are causally related to dementia or confounded by poorer health status remains uncertain.
Trial registration
Registered on clinicaltrials.gov NCT00005131.
Similar content being viewed by others
Introduction
Vitamin D in its activated form [1,25-dihydroxyvitamin D] may be important for cognitive functioning and protective against neurovascular injury [1, 2]. Vitamin D receptors are located in the cortex and hippocampus, areas of the brain important for cognitive functioning, and vitamin D receptor downregulation in these areas has been associated with Alzheimer’s disease [1]. Therefore, adequate serum concentrations of 25-hydroxyvitamin D [25(OH)D], the primary circulating form of vitamin D, in mid-life may help prevent cognitive decline, Alzheimer’s disease and vascular dementia in later-life. However, prior research on the associations between 25(OH) D and cognitive functioning have provided mixed results [3,4,5,6,7,8,9,10,11]. Nevertheless, a recent systematic review and meta-analysis of five cohort studies provided some evidence towards a positive and significant association of low 25(OH) D with dementia risk [5].
Additionally, vitamin D receptor gene polymorphisms have been associated with depressive symptoms [12]. Low 25(OH) D concentrations have also been associated with muscle weakness [13], reduced physical performance [14], frailty [15], and falls [16], but interventional trials of vitamin D supplementation on functional outcomes have shown no benefit or have been inconclusive [17,18,19]. The identification of easily modifiable risk factors in the regulation of mood and physical function in the elderly is of great importance as these affect the quality of life [20, 21].
In sum, the relationship of 25(OH) D concentrations with cognitive function, depression, and physical functioning have been inconclusive to date. Cross-sectional studies conducted in the elderly of the associations of 25(OH) D with neuropsychological outcomes may be limited by reverse causation. To further address this knowledge gap, we therefore examined associations between mid-life 25(OH) D concentrations and late-life performance on a comprehensive battery of neuropsychological, functional, and depression testing, and the association with incident dementia, in the Atherosclerosis Risk in Communities (ARIC) cohort.
Methods
Study population
The ARIC study is an ongoing community-based cohort which in 1987–1989 enrolled 15,792 participants, aged 45–65 years, from four U.S. communities, as previously described [22]. After baseline, participants attended up to five additional in-person study visits (which included cognitive testing at 4 of these visits), and they were also followed by semi-annual telephone interviews and active surveillance of community hospitals. ARIC was approved by the institutional review boards of each participating institution, and all participants provided written informed consent at each visit.
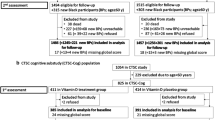
The present analysis includes all ARIC participants (N = 13,039) who had 25(OH) D measurement in mid-life at visit 2 (1990–1992) and were free from dementia at this visit. See Fig. 1 for exclusions. At ARIC visit 5 (2011–2013), all surviving participants were invited to participate in the ARIC Neurocognitive Study (ARIC-NCS) exam (n = 5914). In this present study, we examined the association of mid-life (visit 2) 25(OH) D levels with neuropsychological performance assessed at the ARIC-NCS study ~ 20-years later and with incident dementia occurring over this 20-year follow-up.
Covariates of interest
Serum 25(OH) D was only measured at ARIC visit 2 for the whole cohort, which is why this visit is the baseline for the present analysis. The baseline characteristics of study participants were obtained at visit 2 from questionnaires, medication inventory, physical exam, and laboratory data, except as otherwise noted. Body mass index (BMI) was measured from height and weight. Systolic blood pressure (SBP) was calculated from the mean of the second and third measurements out of three obtained. Diabetes was defined as a fasting glucose ≥126 mg/dL or non-fasting glucose ≥200 mg/dL, a self-reported physician diagnosis of diabetes, or current use of hypoglycemic medication. Total and HDL-cholesterol were measured using standardized enzymatic assays [23]. The Chronic Kidney Disease Epidemiology Collaboration formula [24] was used to estimate glomerular filtration rate (eGFR). Serum intact parathyroid hormone (PTH) concentrations was measured using an Elecsys assay (Roche Diagnostics, Indianapolis, IN), and calcium and phosphate concentrations were measured by a colorimetric method through a Modular P-Chemistry Analyzer (Roche Diagnostics) [25].
25(OH) D measurement
Serum 25(OH) D concentrations were measured from fasting samples that had been collected at visit 2 (1990–1992) and stored at − 70 °C until measured in 2012–2013 using liquid chromatography-tandem high-sensitivity mass spectrometry (Waters Alliance e2795, Milford, MA, USA) [26]. Concentrations of serum/plasma 25(OH) D have previously been shown to have long-term stability when measured from frozen samples [27, 28]. The coefficients of variation were 20.8 and 6.9% for 25(OH)D2 and 25(OH)D3, respectively. Using blind duplicate samples, the intraclass correlation coefficients, calculated by the icc() function in the R package irr, were 0.96 (95% CI 0.95–0.96) for 25(OH)D2 and 0.91 (0.86–0.92) for 25(OH)D3. Total 25(OH) D concentration was calculated from the sum of 25(OH)D2 and 25(OH)D3. To convert 25(OH) D from ng/mL to nmol/L, multiply by 2.496.
Outcome measures
Previously, in the ARIC cohort, we evaluated the association of 25(OH) D with cognitive decline using a global cognitive Z-score based on repeated measures of just 3 cognitive tests [7, 8], and no relationships were found. Our primary outcome for the present analysis is the association of mid-life 25(OH) D with the late-life performance on a more extensive battery of neuropsychological tests at the ARIC-NCS exam.
Neuropsychological testing at the ARIC-NCS were administered in a quiet room by trained examiners using standardized protocols [29, 30] and included the following cognitive domains: memory (Delayed Word Recall Test, Logical Memory Test Part I and II, Incidental Learning), language (Animal Naming, Boston Naming Test, Word Fluency Test), and processing speed and executive function (Trail Making Test A and B, Digital Symbol Substitution Test, Digit Span Backwards). Secondary outcomes assessed includes functional ability [Functional Activities Questionnaire (FAQ), Time to Walk 4 m, Short Physical Performance Battery (SPPB) score and grip strength], mental status [Mini-Mental State Examination (MMSE)], and depressive symptoms using the 11-item Center for Epidemiological Studies-Depression (CES-D). The (Additional file 1: Supplemental Methods) section provides more details about how these tests are performed and the normative scores for the ARIC cohort.
Dementia ascertainment
Incident dementia cases in ARIC were adjudicated by an expert dementia classification committee comprised of eight clinicians including four physicians and four neuropsychologists [31]. Dementia was ascertained using a pre-determined algorithm, incorporating data from the cognitive tests performed at ARIC visits 2, 4, and 5, the full neuropsychological assessment performed at visit 5, participant interviews, informant (family member) interviews, and also hospital discharge codes and diagnostic codes from death certificates, as has been previously described in ARIC [31,32,33,34,35]. Each dementia case was adjudicated by a physician (either a geriatrician or neurologist) and a neuropsychologist, and in cases of disagreement a third clinician confirmed the diagnosis.
Statistical analyses
We used seasonally-adjusted 25(OH) D concentrations as previously described in ARIC [26] and categorized them based on established clinical cut-points [36, 37] as deficient (< 20), intermediate (20- < 30), or sufficient (≥30 ng/mL). We also examined 25(OH) D continuously per standard deviation (SD) decrement. We used multivariable-adjusted linear regression models to examine the non-concurrent cross-sectional associations between mid-life 25(OH) D (at visit 2) and later-life neuropsychological and cognitive testing, functional ability, and depressive symptoms (at visit 5). Cox regression models were used for the incident dementia analysis. We verified that the proportionally hazards assumption was not violated by interacting 25(OH) D categories with log follow-up time; results were not significant.
We used progressively adjusted models. Model 1, our main model, adjusted for demographic, behavioral, and genetic factors: age (years), sex, race/center (MD-whites; MN-whites; NC-whites; NC-blacks; MS-blacks), education (<high school; high school or equivalent; college, graduate or professional school; assessed at visit 1), BMI (continuous, kg/m2), smoking status (current; former; never), alcohol consumption (current; former; never), physical activity (score range 1 to 5, using Baecke Physical Activity questionnaire [38] at visit 1), and APOE ε4 genotype. Model 2 further adjusted for cardiovascular disease risk factors: SBP, use of hypertension medication, total and HDL cholesterol (mg/dL), use of cholesterol medications, diabetes, prevalent coronary heart disease, prevalent stroke, and estimated glomerular filtration rate (eGFR, mL/min/1.73 m2). Model 3 additionally adjusted for biomarkers related to 25(OH) D metabolism: PTH (pg/mL), calcium (mg/dL), and phosphorus (mg/dL).
In our primary cognitive analyses, to account for missing data and loss of follow-up between visits 2 and 5, we imputed missing covariates at baseline (visit 2) and missing neurocognitive outcomes at the ARIC-NCS (visit 5) using multiple imputation by chained equation methods [39] (see Additional file 1: Table Se-1 for imputed numbers). This method of accounting for attrition is recommended by the ARIC-NCS working group and has been previously validated in the ARIC cohort [40]. However, in a sensitivity analysis, we also considered a “complete-case” analysis of only those participants who attended both visit 2 and visit 5 (2011–2013) (n = 5914). In another sensitivity analysis, we examined all participants who were not known to be deceased at the time of the ARIC-NCS visit (participants who came to the ARIC-NCS and those who did not attend but were alive). In our Cox models, we assessed for interactions by age, race/center, and sex. We considered p-values < 0.05 to be statistically significant and performed analyses using Stata Version 15 (StataCorp, College Station, TX).
Results
Baseline characteristics
Among the 13,039 participants, the mean (SD) age in mid-life was 57.4 (5.7) years and 25(OH) D concentration was 24.3 (8.6) ng/mL. Participants were 57% women, 24% black, and 33% had deficient, 44% intermediate, and 23% sufficient 25(OH) D concentrations. On average, participants with sufficient mid-life 25(OH) D were older, had lower BMI, SBP, total cholesterol, eGFR, PTH, and phosphate levels, and higher HDL-cholesterol and physical activity index compared to participants with deficient 25(OH) D concentrations. They were more likely to be white, current drinkers and on cholesterol lowering medications. They were less likely to be women, current smokers, on antihypertensive medications, have diabetes, or prevalent stroke (Table 1). The baseline characteristics of participants by attrition status is presented in Additional file 1: Table Se-2. Participants who attended the ARIC-NCS visit (at visit 5) tended to be younger, female, white, and had a more favorable cardio-metabolic profile at baseline than those who did not attend the ARIC-NCS visit.
Neuropsychological test performance, functional ability, mental status, and depressive symptoms
The mean (SD) age in late-life was 75.8 (5.3) years. 25(OH) D concentrations at mid-life were not associated with most of the neuropsychological testing outcomes (Fig. 2). In the domain of memory, we found intermediate concentrations of 25(OH) D to be associated with the Delayed Word Recall test in our main model but further adjustment for cardiovascular disease risk factors in model 2 yielded null results (Table 2). We found no association of 25(OH) D with outcomes in the domain of language and verbal fluency (Table 2). In the domain of processing speed and executive function, lower 25(OH) D per 1 SD decrement was associated with lower Trail B times and higher digit span backwards score (i.e. more favorable scores), which is in contrast to our hypotheses (Table 3). There was no significant associations of 25(OH) D with functional ability, mental status, and depressive symptoms 20-years after measurement of 25(OH) D (all p > 0.05, Table 4). In our sensitivity analyses, the results were also mostly null (and consistent with primary analysis) among only the participants who presented for the ARIC-NCS visit [n = 5914 (“complete-case” analysis); Additional file 1: Table Se-3] and among all the participants who were known to be alive at the ARIC-NCS visit (n = 9356; Additional file 1: Table Se-4).
Association between mid-life 25(OH)D (1990-1992) and Later Life. Neuropsychological Test Performance (2011-2013): ARIC-NCS. DWR=Delayed word recall test; LM=Logical memory; IL=Incidental learning symbol; WFT=Word fluency test; DSS=Digit symbol substitution; DSB=Digit span backwards; FAQ=Functional activities questionnaire; 4 MS=Time to walk 4 meters; GS=Grip strength; SPPB=Short Physical Performance Battery; CES-D=Center for Epidemiologic. Studies Depression; MMSE=Mini-mental state exam. aA higher value indicates a more favorable performance/measure; b a lower value indicates a more favorable performance/measure. Results were derived from multivariable linear regression models. Figure presents the adjusted difference in neuropsychological performance for intermediate 25(OH)D (20-29 ng/ml) [shown in black circles] and deficient vitamin D (<20 ng/ml) [shown in red circles], compared to sufficient 25(OH)D ≥30 ng/mL as reference. Models were adjusted for age, sex, race/center, educational, body mass index, smoking status, alcohol consumption, physical activity, and APOE ε. To covert 25(OH)D from ng/mL to nmol/L, multiply by 2.496
Dementia
There were 1323 incident cases of dementia over a median follow-up of 20 years (235,308 person-years). The unadjusted incidence rate (95% CI) per 1000 person-years were 4.83 (4.29, 5.44), 5.73 (5.28, 6.20), and 6.07 (5.54, 6.66) for sufficient, intermediate, and deficient concentrations of 25(OH) D, respectively. When compared to participants with sufficient 25(OH) D, the hazard ratios (95% CI) were 1.12 (0.97, 1.30) for intermediate and 1.26 (1.06, 1.49) for deficient 25(OH) D concentrations after adjustment for variables in our main model which included demographic, behavioral, and genetic factors, p = 0.01 for trend across categories (Table 5, model 1). Results remained statistically significant for trends across categories (p = 0.01) in our fully-adjusted model 3, with an increased risk for incident dementia (HR 1.24 [95% CI 1.05, 1.48] for participants with deficient 25(OH) D, compared to sufficient concentrations. There were no interactions by age, race, or sex (all p > 0.05).
Discussion
In this community-based cohort, deficient 25(OH) D concentrations in mid-life were significantly associated with risk of incident dementia but were mostly not associated with late-life performance on neuropsychological testing, functional ability, or depression testing approximately 20-years later.
Low serum concentrations of 25(OH) D have previously been associated with stroke [26], coronary heart disease [26], and cardiovascular risk factors such as hypertension, diabetes, and lipids [23, 41, 42]. A growing body of evidence has also suggested a possible role of vitamin D in the development of dementia [1] and our findings appears to be consistent with some of such observational studies [5]. This may be due to the role of activated vitamin D in preserving healthy neurons and protection against known risk factors of dementia [1, 2, 5]. Despite this, vitamin D supplementation has not been shown to prevent dementia in prior randomized control trials, albeit some of these trials used lower doses of vitamin D supplements or studied patients with existing impaired cognition [43, 44]. It is also possible that vitamin D in the form of supplementation does not confer the same benefit as when obtained from natural sources such as diet and sunlight. Vitamin D supplementation, when combined with calcium supplements, may actually be associated with some harms such as hypercalcemia, hypercalcuria, kidney stones, and vascular events [19, 45,46,47]. However, a Mendelian randomization study did not find evidence of genetically-determined 25(OH) D concentrations to be causally related to cognitive function [48].
Using data from the ARIC cohort, we previously had found that 25(OH) D concentrations were not associated with 10-year or 20-year cognitive decline using a global Z-score based on repeated measures of just 3 cognitive tests [7, 8]. However, in a subset of the ARIC cohort (n = 1652) from the southern ARIC field centers (Jackson, MS and Forsyth County, NC) who were participating in the ARIC Brain MRI ancillary study, we found a suggestive association of lower 25(OH) D concentrations with hospitalized incident dementia (based on only ICD9 codes), but results were not statistically significant [7]. In that earlier study, comparing the lowest vs. highest race-specific tertiles of 25(OH) D, the hazard ratio for incident dementia for whites was 1.32 (95% CI 0.69, 2.55) and for blacks was 1.53 (0.84, 2.79)], but our analyses may have been underpowered with only 145 cases of hospitalized incident dementia [7].
In this extension of our prior work, our present study provides 1) a much larger sample size from ARIC (N = 13,039) from all 4 field centers (including the northern sites of Minnesota and Maryland), 2) a more extensive battery of neuropsychological and cognitive testing outcomes, 3) a longer follow-up period (20-years) and 4) a greater number of incident dementia cases (N = 1323) that have now been formally adjudicated. In the present analyses, the determination of incident dementia used a very formal algorithm that incorporated all of the available data from in-person testing spanning over 20-years, participant and informant interviews, and ICD9 codes from hospitalizations and death certificates that was then adjudicated by an expert clinician panel.
We now confirm a failure to find a consistent association of mid-life 25(OH) D with performance on a more extensive battery of neuropsychological, functional, and depressive symptoms testing administered 20-years later. In an exploratory model, we also examined more extreme vitamin D deficiency [comparing severe deficiency (< 5 ng/mL), moderate deficiency (5- < 10 ng/mL), and mild 25(OH) D deficiency (10- < 20 ng/mL) to adequate 25(OD) H concentrations (≥ 20 ng/mL)] with neuropsychological performance measures and findings were still largely null and consistent with primary analyses (results not shown).
However, in our current analysis, we did find an association with incident dementia, which warrants further explanation. Considering that some of these neuropsychological testing outcomes were used in the adjudication of dementia, our inability to find positive associations with most of these individual neuropsychological tests seems inconsistent with the positive association we found with incident dementia. Dementia affects the quality of life and may have prevented some participants from returning for the ARIC-NCS visit where all the neuropsychological, functional ability, and depression testing were done; whereas the diagnosis of incident dementia was made by both in-person visits and also by telephone interviews and hospitalization surveillance outside of the visit and included individuals who were unable or unwilling to attend the in-person visits. We did account for this attrition for the in-person visits with multiple imputation using methods previously validated in ARIC [40]; however some selection bias may have remained. It is possible that 25(OH) D is associated with dementia through other vascular mechanisms not captured by these neuropsychological and functional tests. Or it is possible that the association of 25(OH) D and incident dementia may be due to residual confounding in this observational study, despite our efforts to perform robust statistical adjustment for a number of key confounding factors.
The VITamin D and OmegA-3 TriaL (VITAL), which randomized over 20,000 community-dwelling adults aged ≥50 years to a higher dose of vitamin D supplementation (2000 IU/day) vs. placebo, will further evaluate the role of vitamin D supplementation for the prevention of cognitive decline [49]. Note that the VITAL trial recently reported that vitamin D supplementation did not reduce incident cardiovascular disease or cancer outcomes [50], but the cognitive outcomes have not yet been reported. The Study to Understand Vitamin D and Fall Reduction in You (STURDY) is an on-going randomized clinical trial investigating the role of vitamin D supplements (at doses ranging from 200 to 4000 IU/day) on the outcomes of functional measures (short physical performance battery, gait speed, and grip strength) and incident falls [16], which will also be informative when published.
In older adults, lower 25(OH) D concentrations have also been shown to be cross-sectionally associated with depressive symptoms [51, 52]. Tryptophan hydroxylase 2 (the catalyst which produces serotonin, a neurotransmitter implicated in the pathogenesis of depression, from tryptophan) has been found to be modulated by 25(OH) D [53]. However, a prior study of older adults (the Pro.V.A. Study) only found 25(OH) D to be cross-sectionally but not longitudinally associated with depressive symptoms [52]. In another analysis of older women enrolled in the Women’s Health Initiative Observational Study, higher vitamin D intake from food sources was associated with a lower risk of depression after 3 years; however supplementation with vitamin D (400 IU/day) in the Women’s Health Initiative randomized clinical trial was not associated with depression score [54]. In this current analysis from ARIC, we did not find any association of mid-life 25(OH) D with late-life depression score (assessed by CESD). The VITAL clinical trial mentioned above, evaluating a higher dose of vitamin D supplements (2000 IU/day) vs. placebo, will provide further understanding of the role of vitamin D for the prevention of depression in mid-life and older adults [55].
Strengths and limitations
Our study has several limitations, which should be noted. First, we had only one measure of 25(OH) D in mid-life for the whole cohort (which we seasonally-adjusted); however 25(OH) D concentrations may vary over time and one-time measurements may not be reflective of concentrations at the time outcomes were ascertained. We also examined the use of vitamin D supplementation across visits (i.e. ARIC visits 2–5) and found little to no significant differences in proportion of participants who were on supplementation across baseline 25(OH) D groups at a given ARIC visit. Additionally, vitamin D supplement use was very infrequent at ARIC visit 2 (baseline for this analysis), at < 2%. Second, we imputed outcomes for a large number of participants not present at the ARIC-NCS visit. Nevertheless, “complete-case” results for participants present at the ARIC-NCS visit (visit 5) were very similar to those obtained from our imputation. We performed numerous linear regression models for a large battery of neuropsychological/functional tests and any significant associations may have been found by chance; however our findings for the neuropsychological/functional tests were largely null, so correcting for multiple testing would only further emphasize the null relationships noted. Other factors that might be associated with dementia (such as homocysteine, folate, B-vitamins, dietary intake of dairy products and fatty fish etc.) were not measured in ARIC at visit 2. (A food frequency questionnaire was administered only at ARIC visit 1 and 3). Thyroid stimulating hormone (TSH) was measured but it was not associated with 25(OH) D after adjustment for age, race, and sex.
Importantly though, our study has many strengths. In the well-characterized ARIC cohort, we were able to evaluate the association of mid-life 25(OH) D concentrations with a large battery of neuropsychological and functional tests conducted approximately 20-years later, as well as incident dementia outcomes over this same period. We measured 25(OH) D in mid-life when our participants were free from dementia and assessed outcomes in later life (~ 20 years), thereby limiting the effect of reverse causation, a problem which has plagued many other studies. We accounted for numerous potentially confounding lifestyle variables which have been found to be associated with serum 25(OH) D concentrations [56] and increased risk of dementia such as increasing age, black race, physical activity etc. as well as for the APOE ε4 genotype [57]. Individuals in poorer health states may be less likely to participate in outdoor physical activity and thus more likely to be 25(OH) D deficient. Nevertheless, despite robust adjustment, residual confounding may still explain associations see with incident dementia. Finally, our method of dementia ascertainment may be more comprehensive than other studies because in addition to review of medical and death certificate records, an in-person neuropsychological assessment, informant interview, and expert review were all used to adjudicate the cases of dementia [31,32,33,34,35].
Conclusions
In conclusion, we found lower concentrations of 25(OH) D in mid-life were not associated with an extensive battery of neuropsychological, functional, and depression testing in late-life, but were associated with incident dementia in this biracial cohort. Although our long-term prospective design makes reverse causation unlikely, residual confounding may still explain associations seen. It is difficult to explain the association of serum 25(OH) D with dementia, given the lack of association of 25(OH) D concentrations with well-measured cognitive testing spanning 20 years [8]. Low serum concentrations of 25(OH) D may simply be a surrogate marker of a poorer health status. The VITAL interventional trial of vitamin D supplements (at 2000 IU/day) vs placebo failed to show a reduction in cancer or cardiovascular outcomes [50], but the cognitive and depression outcomes from VITAL have not yet been reported. Thus, whether the association with incident dementia is causal, or due to another process, is unclear and warrants further study in the on-going interventional trials.
Availability of data and materials
The ARIC cohort participates in the National Heart, Lung, and Blood Institute’s Biologic Specimen and Data Repository (BioLINCC). The ARIC data are available upon request through BioLINCC (https://biolincc.nhlbi.nih.gov/studies/aric/).
Abbreviations
- 25(OH)D:
-
25-hydroxyvitamin D
- ARIC:
-
Atherosclerosis Risk in Communities
- ARIC-NCS:
-
ARIC Neurocognitive Study
- BMI:
-
Body mass index
- CDR:
-
Clinical Dementia Rating
- CES-D:
-
Center for Epidemiological Studies-Depression
- eGFR:
-
estimated glomerular filtration rate
- FAQ:
-
Functional Activities Questionnaire
- MMSE:
-
Mini-mental state examination
- PTH:
-
Parathyroid hormone
- SBP:
-
Systolic blood pressure
- SPPB:
-
Short Physical Performance Battery
- TICSm:
-
Telephone Interview for Cognitive Status–Modified
- VDR:
-
Vitamin D receptors
- VITAL:
-
VITamin D and OmegA-3 TriaL
References
Buell JS, Dawson-Hughes B. Vitamin D and neurocognitive dysfunction: preventing "D"ecline? Mol Asp Med. 2008;29(6):415–22.
Schlogl M, Holick MF. Vitamin D and neurocognitive function. Clin Interv Aging. 2014;9:559–68.
Annweiler C, Allali G, Allain P, Bridenbaugh S, Schott AM, Kressig RW, Beauchet O. Vitamin D and cognitive performance in adults: a systematic review. Eur J Neurol. 2009;16(10):1083–9.
Balion C, Griffith LE, Strifler L, Henderson M, Patterson C, Heckman G, Llewellyn DJ, Raina P. Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology. 2012;79(13):1397–405.
Sommer I, Griebler U, Kien C, Auer S, Klerings I, Hammer R, Holzer P, Gartlehner G. Vitamin D deficiency as a risk factor for dementia: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):16.
van der Schaft J, Koek HL, Dijkstra E, Verhaar HJ, van der Schouw YT, Emmelot-Vonk MH. The association between vitamin D and cognition: a systematic review. Ageing Res Rev. 2013;12(4):1013–23.
Michos ED, Carson KA, Schneider AL, Lutsey PL, Xing L, Sharrett AR, Alonso A, Coker LH, Gross M, Post W, et al. Vitamin D and subclinical cerebrovascular disease: the atherosclerosis risk in communities brain magnetic resonance imaging study. JAMA Neurol. 2014;71(7):863–71.
Schneider ALC, Zhao D, Lutsey PL, Gottesman RF, Sharrett AR, Rawlings AM, Alonso A, Knopman D, Mosley TH, Selvin E, et al. Serum Vitamin D concentrations and cognitive change over 20 years: the atherosclerosis risk in communities neurocognitive study. Neuroepidemiology. 2018;51(3–4):131–7.
Slinin Y, Paudel ML, Taylor BC, Fink HA, Ishani A, Canales MT, Yaffe K, Barrett-Connor E, Orwoll ES, Shikany JM, et al. 25-Hydroxyvitamin D levels and cognitive performance and decline in elderly men. Neurology. 2010;74(1):33–41.
Tolppanen AM, Williams DM, Lawlor DA. The association of serum ionized calcium and vitamin D with adult cognitive performance. Epidemiology. 2011;22(1):113–7.
McGrath J, Scragg R, Chant D, Eyles D, Burne T, Obradovic D. No association between serum 25-hydroxyvitamin D3 level and performance on psychometric tests in NHANES III. Neuroepidemiology. 2007;29(1–2):49–54.
Kuningas M, Mooijaart SP, Jolles J, Slagboom PE, Westendorp RG, van Heemst D. VDR gene variants associate with cognitive function and depressive symptoms in old age. Neurobiol Aging. 2009;30(3):466–73.
Dawson-Hughes B. Serum 25-hydroxyvitamin D and muscle atrophy in the elderly. Proc Nutr Soc. 2012;71(1):46–9.
Toffanello ED, Perissinotto E, Sergi G, Zambon S, Musacchio E, Maggi S, Coin A, Sartori L, Corti MC, Baggio G, et al. Vitamin D and physical performance in elderly subjects: the Pro.V.A study. PLoS One. 2012;7(4):e34950.
Zhou J, Huang P, Liu P, Hao Q, Chen S, Dong B, Wang J. Association of vitamin D deficiency and frailty: a systematic review and meta-analysis. Maturitas. 2016;94:70–6.
Michos ED, Mitchell CM, Miller ER 3rd, Sternberg AL, Juraschek SP, Schrack JA, Szanton SL, Walston JD, Kalyani RR, Plante TB, et al. Rationale and design of the study to understand fall reduction and Vitamin D in you (STURDY): a randomized clinical trial of Vitamin D supplement doses for the prevention of falls in older adults. Contemp Clin Trials. 2018;73:111–22.
Stockton KA, Mengersen K, Paratz JD, Kandiah D, Bennell KL. Effect of vitamin D supplementation on muscle strength: a systematic review and meta-analysis. Osteoporos Int. 2011;22(3):859–71.
Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 2018;6(11):847–58.
Kahwati LC, Weber RP, Pan H, Gourlay M, LeBlanc E, Coker-Schwimmer M, Viswanathan M. Vitamin D, Calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: evidence report and systematic review for the US preventive services task force. JAMA. 2018;319(15):1600–12.
Windham BG, Harrison KL, Lirette ST, Lutsey PL, Pompeii LA, Gabriel KP, Koton S, Steffen LM, Griswold ME, Mosley TH. Relationship between midlife cardiovascular health and late-life physical performance: the ARIC study. J Am Geriatr Soc. 2017;65(5):1012–8.
Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–89.
The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702.
Faridi KF, Zhao D, Martin SS, Lupton JR, Jones SR, Guallar E, Ballantyne CM, Lutsey PL, Michos ED. Serum vitamin D and change in lipid levels over 5 y: the atherosclerosis risk in communities study. Nutrition. 2017;38:85–93.
Pugliese G, Solini A, Bonora E, Orsi E, Zerbini G, Giorgino F, Cavalot F, Pontiroli AE, Baroni MG, Morano S, et al. The chronic kidney disease epidemiology collaboration (CKD-EPI) equation provides a better definition of cardiovascular burden associated with CKD than the modification of diet in renal disease (MDRD) study formula in subjects with type 2 diabetes. Atherosclerosis. 2011;218(1):194–9.
Kim SM, Zhao D, Schneider ALC, Korada SK, Lutsey PL, Guallar E, Alonso A, Windham BG, Gottesman RF, Michos ED. Association of parathyroid hormone with 20-year cognitive decline: the ARIC study. Neurology. 2017;89(9):918–26.
Schneider AL, Lutsey PL, Selvin E, Mosley TH, Sharrett AR, Carson KA, Post WS, Pankow JS, Folsom AR, Gottesman RF, et al. Vitamin D, vitamin D binding protein gene polymorphisms, race and risk of incident stroke: the atherosclerosis risk in communities (ARIC) study. Eur J Neurol. 2015;22(8):1220–7.
Agborsangaya C, Toriola AT, Grankvist K, Surcel HM, Holl K, Parkkila S, Tuohimaa P, Lukanova A, Lehtinen M. The effects of storage time and sampling season on the stability of serum 25-hydroxy vitamin D and androstenedione. Nutr Cancer. 2010;62(1):51–7.
Bodnar LM, Catov JM, Wisner KL, Klebanoff MA. Racial and seasonal differences in 25-hydroxyvitamin D detected in maternal sera frozen for over 40 years. Br J Nutr. 2009;101(2):278–84.
Rawlings AM, Bandeen-Roche K, Gross AL, Gottesman RF, Coker LH, Penman AD, Sharrett AR, Mosley TH. Factor structure of the ARIC-NCS neuropsychological battery: an evaluation of invariance across vascular factors and demographic characteristics. Psychol Assess. 2016;28(12):1674–83.
Schneider AL, Sharrett AR, Gottesman RF, Coresh J, Coker L, Wruck L, Selnes OA, Deal J, Knopman D, Mosley TH. Normative data for 8 neuropsychological tests in older blacks and whites from the atherosclerosis risk in communities (ARIC) study. Alzheimer Dis Assoc Disord. 2015;29(1):32–44.
Knopman DS, Gottesman RF, Sharrett AR, Wruck LM, Windham BG, Coker L, Schneider ALC, Hengrui S, Alonso A, Coresh J, et al. Mild cognitive impairment and dementia prevalence: the atherosclerosis risk in communities neurocognitive study. Alzheimers Dement. 2016;2:1–11.
Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, Coresh J, Knopman D, Power MC, Rawlings A, et al. Midlife hypertension and 20-year cognitive change: the atherosclerosis risk in communities neurocognitive study. JAMA Neurol. 2014;71(10):1218–27.
Norby FL, Chen LY, Soliman EZ, Gottesman RF, Mosley TH, Alonso A. Association of left ventricular hypertrophy with cognitive decline and dementia risk over 20 years: the atherosclerosis risk in communities-neurocognitive study (ARIC-NCS). Am Heart J. 2018;204:58–67.
Chen LY, Norby FL, Gottesman RF, Mosley TH, Soliman EZ, Agarwal SK, Loehr LR, Folsom AR, Coresh J, Alonso A. Association of Atrial Fibrillation With Cognitive Decline and Dementia Over 20 Years: The ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study). J Am Heart Assoc. 2018;7(6):e007301.
Wang S, Fashanu OE, Zhao D, Guallar E, Gottesman RF, Schneider ALC, McEvoy JW, Norby FL, Aladin AI, Alonso A, et al. Relation of elevated resting heart rate in mid-life to cognitive decline over 20 years (from the atherosclerosis risk in communities [ARIC] study). Am J Cardiol. 2019;123(2):334–40.
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, et al. The 2011 report on dietary reference intakes for calcium and Vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–8.
Holick MF, Vitamin D. Deficiency. N Engl J Med. 2007;357(3):266–81.
Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–42.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Rawlings AM, Sang Y, Sharrett AR, Coresh J, Griswold M, Kucharska-Newton AM, Palta P, Wruck LM, Gross AL, Deal JA, et al. Multiple imputation of cognitive performance as a repeatedly measured outcome. Eur J Epidemiol. 2017;32(1):55–66.
Lutsey PL, Michos ED. Vitamin D, Calcium, and atherosclerotic risk: evidence from serum levels and supplementation studies. Curr Atheroscler Rep. 2013;15(1):293.
Lupton JR, Faridi KF, Martin SS, Sharma S, Kulkarni K, Jones SR, Michos ED. Deficient serum 25-hydroxyvitamin D is associated with an atherogenic lipid profile: The Very Large Database of Lipids (VLDL-3) study. J Clin Lipidol. 2016;10(1):72–81.e71.
Rossom RC, Espeland MA, Manson JE, Dysken MW, Johnson KC, Lane DS, LeBlanc ES, Lederle FA, Masaki KH, Margolis KL. Calcium and vitamin D supplementation and cognitive impairment in the women's health initiative. J Am Geriatr Soc. 2012;60(12):2197–205.
Stein MS, Scherer SC, Ladd KS, Harrison LC. A randomized controlled trial of high-dose vitamin D2 followed by intranasal insulin in Alzheimer's disease. J Alzheimers Dis. 2011;26(3):477–84.
Khan SU, Khan MU, Riaz H, Valavoor S, Zhao D, Vaughan L, Okunrintemi V, Riaz IB, Khan MS, Kaluski E, et al. Effects of nutritional supplements and dietary interventions on cardiovascular outcomes: an umbrella review and evidence map. Ann Intern Med. 2019;171(3):190–19.
Razzaque MS. Can adverse effects of excessive vitamin D supplementation occur without developing hypervitaminosis D? J Steroid Biochem Mol Biol. 2018;180:81–6.
Malihi Z, Wu Z, Stewart AW, Lawes CM, Scragg R. Hypercalcemia, hypercalciuria, and kidney stones in long-term studies of vitamin D supplementation: a systematic review and meta-analysis. Am J Clin Nutr. 2016;104(4):1039–51.
Maddock J, Zhou A, Cavadino A, Kuzma E, Bao Y, Smart MC, Saum KU, Schottker B, Engmann J, Kjaergaard M, et al. Vitamin D and cognitive function: a Mendelian randomisation study. Sci Rep. 2017;7(1):13230.
Manson JE, Bassuk SS, Lee IM, Cook NR, Albert MA, Gordon D, Zaharris E, Macfadyen JG, Danielson E, Lin J, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials. 2012;33(1):159–71.
Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Gordon D, Copeland T, D'Agostino D, et al. Vitamin D supplements and prevention of Cancer and cardiovascular disease. New Engl J Med. 2019;380(1):33–44.
Hoogendijk WG, Lips P, Dik MG, Deeg DH, Beekman AF, Penninx BH. Depression is associated with decreased 25-hydroxyvitamin d and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. 2008;65(5):508–12.
Toffanello ED, Sergi G, Veronese N, Perissinotto E, Zambon S, Coin A, Sartori L, Musacchio E, Corti MC, Baggio G, et al. Serum 25-hydroxyvitamin D and the onset of late-life depressive mood in older men and women: the pro.V.a. study. J Gerontol A Biol Sci Med Sci. 2014;69(12):1554–61.
Patrick RP, Ames BN. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. FASEB J. 2015;29(6):2207–22.
Bertone-Johnson ER, Powers SI, Spangler L, Larson J, Michael YL, Millen AE, Bueche MN, Salmoirago-Blotcher E, Wassertheil-Smoller S, Brunner RL, et al. Vitamin D supplementation and depression in the women's health initiative calcium and vitamin D trial. Am J Epidemiol. 2012;176(1):1–13.
Okereke OI, Reynolds CF 3rd, Mischoulon D, Chang G, Cook NR, Copeland T, Friedenberg G, Buring JE, Manson JE. The VITamin D and OmegA-3 TriaL-depression endpoint prevention (VITAL-DEP): rationale and design of a large-scale ancillary study evaluating vitamin D and marine omega-3 fatty acid supplements for prevention of late-life depression. Contemp Clin Trials. 2018;68:133–45.
McKibben RA, Zhao D, Lutsey PL, Schneider ALC, Guallar E, Mosley TH, Michos ED. Factors associated with change in 25-Hydroxyvitamin D levels over longitudinal follow-up in the ARIC study. J Clin Endocrinol Metab. 2016;101(1):33–43.
Gottesman RF, Albert MS, Alonso A, Coker LH, Coresh J, Davis SM, Deal JA, McKhann GM, Mosley TH, Sharrett AR, et al. Associations between midlife vascular risk factors and 25-year incident dementia in the atherosclerosis risk in communities (ARIC) cohort. JAMA Neurol. 2017;74(10):1246–54.
Acknowledgements
The authors thank the staff and participants of the ARIC study for their vital contributions.
Abstract presentation
An abstract from this work was presented at the 2018 American Heart Association Epidemiology and Lifestyle Meeting in New Orleans, LA. The full manuscript has not been previously published, and is not under consideration elsewhere.
Funding
This work was supported by grant R01NS072243 to Dr. Michos from the National Institute of Neurologic Disorders and Stroke (NINDS) at the National Institutes of Health (NIH). This work was also supported by R01HL103706 from the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health and R01HL103706-S1 from the NIH Office of Dietary Supplements, both to Dr. Lutsey. This TSH measurements was made possible by a NIH/NIDDK grant R01DK089174 to Dr. Elizabeth Selvin. Reagents for the thyroid assays were donated by Roche Diagnostics.
The ARIC Study is a collaborative research supported by National Heart, Lung, and Blood Institute contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C. The ARIC-NCS was funded by U01 HL096812, HL096814, HL096899, HL096902, and HL096917, with additional support from the National Institute of Neurologic Disorders and Stroke.
Drs. Michos and Zhao are also supported by the Blumenthal Scholars Fund for Preventive Cardiology research. Dr. Schneider was supported by National Institute of Neurologic Disorders and Stroke through an administrative supplement to award R25NS065729. Dr. Gross was supported by K01-AG050699 from the National Institute on Aging at the National Institute of Health.
The funding agents were not involved in the design of the study; the collection, analysis and interpretation of data; or in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
O.E.F. and E.D.M. designed the research. O.E.F. analyzed the data under the supervision of D.Z. and E.D.M. P.L.L. and E.D.M. obtained funding for the 25(OH) D measurement. O.E.F. wrote the first draft of the paper. D.Z., A.L.C.S., A.M.R., A.R.S, P.L.L., R.F.G., A.L.G., E.G., A.A., T.H.M., and E.D.M. all reviewed manuscript and provided critical scientific input. O.E.F. and E.D.M. had main responsibility for final content. All authors have approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocols were approved by the Institutional Review Board (IRB) at the Johns Hopkins Bloomberg School of Public Health [615 N. Wolfe Street, Suite E1100, Baltimore, MD 21205]. The study title is the Atherosclerosis Risk in Communities (ARIC) Study. The IRB number is H.34.99.07.02.A1. The ARIC principal investigator is Dr. Josef Coresh. This research was performed in accordance with the Declaration of Helsinki, and all participants provided written informed consent at each visit.
Consent for publication
Not applicable. No personal/individual data was included.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Supplemental Methods.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fashanu, O.E., Zhao, D., Schneider, A.L.C. et al. Mid-life serum Vitamin D concentrations were associated with incident dementia but not late-life neuropsychological performance in the Atherosclerosis Risk in Communities (ARIC) Study. BMC Neurol 19, 244 (2019). https://doi.org/10.1186/s12883-019-1483-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-019-1483-3