Abstract
Background
Pyrazinamide still may be a useful drug for treatment of rifampin-resistant (RR-TB) or multidrug-resistant tuberculosis (MDR-TB) in China while awaiting scale up of new drugs and regimens including bedaquiline and linezolid. The level of pyrazinamide resistance among MDR-TB patients in China is not well established. Therefore, we assessed pyrazinamide resistance in a representative sample and explored determinants and patterns of pncA mutations.
Methods
MDR-TB isolates from the 2007 national drug resistance survey of China were sub-cultured and examined for pyrazinamide susceptibility by BACTEC MGIT 960 method. pncA mutations were identified by sequencing. Characteristics associated with pyrazinamide resistance were analyzed using univariable and multivariable log-binominal regression.
Results
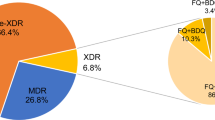
Of 401 MDR-TB isolates, 324 were successfully sub-cultured and underwent drug susceptibility testing. Pyrazinamide resistance was prevalent in 40.7% of samples, similarly among new and previously treated MDR-TB patients. Pyrazinamide resistance in MDR-TB patients was associated with lower age (adjusted OR 0.54; 95% CI, 0.34–0.87 for those aged ≧60 years compared to < 40 years). Pyrazinamide resistance was not associated with gender, residential area, previous treatment history and Beijing genotype. Of 132 patients with pyrazinamide resistant MDR-TB, 97 (73.5%) had a mutation in the pncA gene; with 61 different point mutations causing amino acid change, and 11 frameshifts in the pncA gene. The mutations were scattered throughout the whole pncA gene and no hot spot region was identified.
Conclusions
Pyrazinamide resistance among MDR-TB patients in China is common, although less so in elderly patients. Therefore, pyrazinamide should only be used for treatment of RR/MDR-TB in China if susceptibility is confirmed. Molecular testing for detection of pyrazinamide resistance only based on pncA mutations has certain value for the rapid detection of pyrazinamide resistance in MDR-TB strains but other gene mutations conferring to pyrazinamide resistance still need to be explored to increase its predictive ability .
Similar content being viewed by others
Background
Multidrug-resistant tuberculosis (MDR-TB) including extensively drug-resistant tuberculosis (XDR-TB) has emerged as one of the health threats in China. The proportion of new and previously treated TB patients with MDR was 5.7 and 25.6%, respectively [1]. Pyrazinamide, a first-line drug with bactericidal activity, has an important role in the treatment of both drug-susceptible and drug-resistant tuberculosis. Although its role in the longer MDR-TB regimen has been limited with the availability of new core drugs, such as bedaquiline and linezolid, its role in novel shorter regimens currently under trial but with promising outlooks, is pivotal. Anti-tuberculosis regimens consisting of moxifloxacin, pyrazinamide and other drugs for shortening treatment of multi-drug resistant tuberculosis were evaluated and used [2,3,4,5] before the new guideline was issued by WHO. The new WHO guidelines (2018) recommend that fully oral longer regimens would include at least four agents likely to be effective in the first 6 months and three thereafter. All three group A agents including fluoroquinolones (levofloxacin or moxifloxacin), bedaquiline and linezolid and at least one group B agent should be included. If the regimen cannot be composed with agents from Groups A and B alone, the regimens are completed with Group C agent [6]. Bedaquiline is not widely used in China and only offered in very few provincial and prefecture level hospitals. Linezolid has a very high market price in China, which may bring some obstacles to nationwide use. Therefore, in China group C agents including pyrazinamide may still be used to compose both longer and shorter regimen for drug resistant TB treatment.
Pyrazinamide is a prodrug that requires conversion into pyrazinoic acid by the bacterial enzyme pyrazinamidase/nicotinamidase encoded by pncA gene in M.tuberculosis [7]. Mutations in pncA encoding pyrazinamidase lead to the loss of pyrazinamidase activity and are the major mechanism of pyrazinamide resistance in M. tuberculosis [7, 8]. Pyrazinamide has no activity in vitro at neutral pH but is active at an acid pH (pH 5.5) [9,10]. Pyrazinamide susceptibility testing is difficult because the acidity of culture medium needed for drug activity also restricts the growth of M. tuberculosis. Because of these technical challenges, drug susceptibility for pyrazinamide is seldomly performed in routine settings in many countries including China. This partly explains the paucity of data on the prevalence of pyrazinamide resistance among MDR-TB patients in China. The available data show a large variation in pyrazinamide prevalence, which may be explained through inclusion of selected cases [11,12,13,14]. In this study, we analyzed pyrazinamide resistance, risk factors for resistance, and mutations in the pncA gene, among patients identified with MDR-TB in a nationally representative sample of TB patients in China.
Methods
Patients and mycobacterial isolates
A nationally representative sample of 3634 smear-positive pulmonary tuberculosis patients were included in the 2007 national drug resistance survey, of which 401 (11.0%) cases were identified as MDR-TB cases with the proportion method on Löwenstein-Jensen medium [1]. Out of the 401 MDR-TB strains, 75 strains failed to grow in subculture and 2 strains failed on pyrazinamide susceptibility testing, leaving 324 MDR-TB strains for analysis. These 324 patients were from 30 of all 31 provinces in China (except for Hainan province). The mean age (standard deviation) of the 324 MDR-TB patients included for final analysis was 43.0 (SD 16.5) years and 211 (65.1%) were male. Ethics approval of this study was waived by the Ethical Committees of the Chinese Center for Disease Control and Prevention. The 2007 national drug resistance survey was approved by the Tuberculosis Research Ethics Review Committee of the Chinese Center for Disease Control and Prevention and written informed consent was obtained from each participant.
Patient information
Basic demographic data including age, gender, occupation, area of residence within China, residence in an area with DOTS implementation before 2000 or afterwards, previous anti-TB treatment episodes and previous pyrazinamide usage were collected from the standardized questionnaire used in survey [1].
Drug susceptibility testing
Susceptibility to pyrazinamide was determined with the BACTEC MGIT 960 system (Becton Dickinson) as recommended by the manufacturer. The medium was modified Middlebrook 7H9 broth (pH 5.9) containing 100 μg/ml pyrazinamide. Mycobacterium bovis BCG (ATCC 34540) and Mycobacterium tuberculosis H37Rv (ATCC 27294) were used as pyrazinamide resistant and susceptible controls, respectively. Susceptibility to ofloxacin and kanamycin had been tested with the proportion method on L-J medium in 2007 [1].
Amplification and sequencing of the pncA gene
DNA Sanger sequencing of the pncA gene and its upstream region was performed on all isolates. DNA was extracted from isolates by transferring one loopful of bacteria from L-J slants to a 1.5-ml tube containing 1 ml of Tris-EDTA buffer. Each tube was vortexed for 30 s and placed in a heat block at 80 °C for at least 30 min for inactivation. Tubes were then moved to 100 °C for 15 min and then centrifuged. The supernatant was kept for pncA amplication. The entire pncA gene and 82 bp of an upstream putative regulatory region were amplified as described previously [8]. The primers were as follows: PNCA-F: GTC GGT CAT GTT CGC GAT CG, PNCA-R: GCT TTG CGG CGA GCG CTC CA. The PCR cycling parameters were 95 °C for 5 min, followed by 30 cycles of 95 °C for 1 min, 55 °C for 1 min, and 72 °C for 1 min. PCR was performed in a total volume of 25 μl, and the PCR reaction mixture consisted of 12.5ul 2 × Taq Master Mix (Kangwei, China), 20 pmol of each primer and 2 μl of DNA. Finally, PCR products were directly sequenced using the PNCA-F primers as sequencing primers. The sequencing results were entered into the Basic Local Alignment Search Tool (BLAST, https://blast.ncbi.nlm.nih.gov/Blast.cgi) for comparison with the pncA gene of the Mycobacterium tuberculosis H37Rv.
Synonymous single-nucleotide polymorphisms (sSNP), or nonsynonymous single-nucleotide polymorphisms (nSNP) in the sequencing results of pncA gene that had been reported not to be related to pyrazinamide resistance [15] were excluded when calculating specificity of the genetic mutation. Strains with all other SNPs or insertions or deletions were considered mutant and likely were resistant to pyrazinamide.
Genotyping
Beijing or non-beijing strains were distinguished based on spoligotyping, as described previously [16]. The original binary data were submitted to the SITVITWEB database to obtain the spoligotype.
Statistical analysis
Patients with pyrazinamid resistant M. tuberculosis strains were compared with patients with pyrazinamide susceptible strains with regard to the characteristics provided in the questionnaire used in 2007 drug resistance survey [1] and M. tuberculosis genotype, separately for phenotypically and genotypically determined resistance profiles. Univariable log-binominal regression modeling was used to calculate prevalence ratios (PRs) for factors associated with pyrazinamide resistance. Age, gender, and number of previous TB treatment episodes were fixed in the multivariable model and other characteristics with a p-value < 0.1 or plausibly (epidemiologically or biologically) associated with pyrazinamide resistance were included in the initial multivariable log-binominal regression model. The final model was determined using backward selection, guided by statistical significance (p-value < 0.05) of variables and fit of the model. Data was analyzed using IBM SPSS software, version 19.0.
Results
Phenotypic pyrazinamide resistance
Of 324 MDR-TB isolates, 132 (40.7%) were phenotypically resistant to pyrazinamide, coming from 25 provinces.
Risk factors for phenotypic pyrazinamide resistance
Univariable analysis showed that MDR-TB cases with pyrazinamide resistance were more likely to be younger (crude PR for age ≥ 60 compared to < 40 years: 0.55; 95% CI, 0.35–0.86) and more likely to have non-farming occupations (crude PR: 1.34; 95% CI, 1.03–1.73). In multivariable analysis, only younger age was associated with pyrazinamide resistance (adjusted PR for age ≥ 60 compared to < 40 years: 0.54; 95% CI, 0.34–0.87) (Table 1). The database for Univariable and multivariable analysis of risk factors associated with phenotypic pyrazinamide resistance was available in Additional file 1.
Mutations in the pncA gene
Among 132 strains phenotypically resistant to pyrazinamide, nucleotide changes that include non-synonymous mutations, insertions and deletions in the pncA gene were detected in 97 (73.5%) isolates compared to 13 of 192 (6.8%) pyrazinamide susceptible isolates. The concordance between phenotypic and genotypic results was 85.3% (276/324). Only four point mutations (Met1Thr, Asp12Asn, His137Arg, Thr47Ala) were detected both in phenotypically resistant and in phenotypically susceptible strains. Among the 97 isolates with gene mutations or frameshifts, we found 61 different point mutations causing amino acid change, and 11 frameshift changes. In phenotypically susceptible isolates 15 non-synonymous mutations, 1 frameshift mutation was detected. The mutations were scattered throughout the whole pncA gene and no hot spot regions were found. The frequency of mutations in different regions along the pncA gene is shown in Table 2.
Risk factors for genotypic pyrazinamide resistance
Univariable analysis showed that younger age and Beijing genotype were associated with pncA gene mutations. In multivariable analysis, younger age and Beijing genotype were still risk factors for genotypic resistance (pncA mutation). The adjusted PR for patients aged≧60 compared to < 40 years was 0.56 (95% CI, 0.34–0.91) and for Beijing genotype was 1.84 (95% CI, 1.01–3.34) in comparison with non-Beijing genotype (Table 3). The database for Univariable and multivariable analysis of risk factors with genotypic pyrazinamide resistance was available in Additional file 1.
Association between drug susceptibility to pyrazinamide, and to ofloxacin and kanamycin
Table 4 shows a positive association between drug susceptibility for pyrazinamide versus ofloxacin and kanamycin. Pyrazinamide resistance proportions among ofloxacin-resistant and -susceptible isolates were 62.2 and 33.5% (p < 0.001), respectively. These proportions were 54.8 and 38.7% among kanamycin resistant and susceptible MDR-TB patients (p = 0.05), respectively.
Discussion
Before a new RR/MDR treatment regimen composed of bedaquiline and linezolid can be implemented in the whole of China, pyrazinamide is still being considered an important optional drug in the treatment regimen of RR/MDR-TB given that such a regimen is widely accessible and currently more affordable. The hitherto available data from China showed a large variation in pyrazinamide prevalence as representative data were lacking. This is the first study assessing pyrazinamide resistance among MDR-TB cases from a nationwide representative sample. We showed that 40.7% of MDR-TB isolates exhibited resistance against pyrazinamide and 73.5% of these resistant isolates also showed genotypic resistance. Pyrazinamide resistance proportions among ofloxacin-resistant and kanamycin-resistant strains were both significantly higher than those among susceptible isolates. The reported prevalence of pyrazinamide resistance in MDR-TB isolates elsewhere varied substantially by country, ranging from 36.7 to 84.6% [17,18,19,20,21]. The range of previously reported proportions of pyrazinamide resistance in selected samples from China was 43.1–62.4% [11,12,13,14].
In our study, there were no obvious clinical characteristics significantly associated with phenotypic pyrazinamide resistance except for elderly MDR-TB patients less often having pyrazinamide resistance, as observed before in the USA [20]. One possible explanation is that the younger patients were recently infected with pyrazinamide resistant strains, while the elderly patients had reactivation of more remote infection, when pyrazinamide resistance levels were lower. Inadequate treatment, improper drug regimens, interrupted availability of drugs, or treatment for a very short period and an increased incidence of previous pyrazinamide exposure are possible causes for pyrazinamide resistance [21,22,23]. In one study conducted in Estonia and Latvia, findings were different as for the association between previous pyrazinamide usage and pyrazinamide resistance. In Estonia, the rates of resistance to pyrazinamide showed no difference between new and previously treated cases, whereas in Latvia, pyrazinamide resistance was higher in new cases than in previously treated cases [24]. Our present study also showed that there was no difference between pyrazinamide resistance in new cases versus in the previously treated cases. Patient’s age and lung cavities were previously reported to be associated with pyrazinamide resistance in MDR-TB cases [22], however, the extent to which age affects pyrazinamide resistance among MDR-TB cases was smaller compared with the effects of cavities and treatment history. Unfortunately, we do not have chest X-ray information on cavitation. One mathematical modeling suggested that resistance to second line injectable drugs is the result, rather than the cause, of accumulated resistance to pyrazinamide [25]. In our study, we saw an association between ofloxacin and kanamycin resistance on the one hand and pyrazinamide resistance on the other hand, but almost no full resistance profile among pyrazinamide resistant strains. So pyrazinamide may be a condition for ofloxacin and kanamycin resistance, which supports the above mathematical modeling that resistance of second-line drugs is the result of pyrazinamide resistance. More specific studies need to be conducted to investigate this hypothesis.
The high diversity of pncA mutations in pyrazinamide resistant strains is in contrast to the spectrum of mutations conferring resistance to rifampin and isoniazid. That the pncA gene accumulates multiple and diverse mutations may imply that there is a large target for resistance or resistance can result from multiple different variants acting individually or in concert. However, one study showed that an M. tuberculosis strain harboring a deletion in pncA conferring pyrazinamide resistance was estimated to be endemic longer before the use of pyrazinamide for TB treatment [26]. This finding supports the idea that purifying selection on pncA is relatively weak, which would contribute to its exceedingly high diversity and broaden the adaptive paths to resistance [27].
Among 132 pyrazinamide-resistant MDR-TB isolates, mutations in 97 isolates were scattered along the whole pncA gene. Mutations of the gene coding for pyrazinamidase, pncA is the major mechanism of pyrazinamide resistance. Detection of pncA gene mutations may provide pyrazinamide susceptibility information. The concordance between pncA gene mutations and pyrazinamide susceptibility varies substantially among previous studies, ranging from lower than 50% [28, 29] to higher than 75% [8, 10,11,12, 30]. Our finding was similar to that of most other studies. Scorpio et al reported that the distribution of pncA mutations clustered at three regions 3–7, 61–85, 132–142 [7]. Miotto et al reported that the most frequently affected regions (representing more than 70% of mutated strains) were found at the promoter(− 13 to − 3) and at codons 6 to 15, 50 to70, 90 to 100, 130 to 145, and 170 to 175 [31]. In our study, we found a high variety of pncA gene mutations in the MDR-TB isolates. Our findings support similar observations of widely dispersed mutations in previous studies. Although the basis of this diversity is unclear, it is hypothesized that either the gene is situated in a hot spot region, or that it is a consequence of the lack of DNA mismatch repair mechanisms in MTB [32]. For the mutations in pncA, 40/61 point mutations conferring pyrazinamide resistance that we found have been reported previously [33,34,35], and to our knowledge, 21 novel mutations and all 11 frameshift changes (insertions or deletions) were first found in this study. There are also other unknown resistance mechanisms responsible for the resistance phenotype, such as mutations in rpsA gene, however, low frequency of rpsA gene mutations showed that rpsA gene mutation was not the main mechanism of pyrazinamide resistance [36, 37]. Zimic et al have demonstrated that the efflux rate of pyrazinamide’s active moiety, pyrazinoc acid, predicts pyrazinamide resistance with up to 93% sensitivity [38]. Pyrazinamide acid efflux accounted for 61% of the variability in pyrazinamide susceptibility [39]. One study based on more than 100,000 genomes showed that the sensitivity of genotypic prediction of pyrazinamide resistance based on mutations in and upstream of pncA gene was 91.3% [40]. Whole genome sequencing cannot be routinely conducted and afforded in most areas of China due to technical challenges of whole genome sequencing and analysis of data. There is only one commercial molecular based assay (Genoscholar PZA-TB II) for pyrazinamide resistance detection, developed by the Nipro Corporation (Osaka, Japan), a line-probe assay that includes probes covering the entire pncA coding region and 18 nucleotides upstream [41]. This line-probe assay is unavailable in China, however.
The strength of the present study is that the MDR-TB strains were isolated from a random sample of patients distributed almost around the whole China (30/31 provinces) and were not restricted to only one or a few counties or provinces or one hospital setting. There are also some limitations. Firstly, some of the MDR-TB strains could not be recovered successfully. Secondly, the sample size of the original survey was not set to study geographic, clinical and demographic variation in pyrazinamide resistance, so our analyses may have failed to detect true differences in this regard. Thirdly, only the pncA gene was sequenced and other mechanisms possibly responsible for the pyrazinamide resistance were not explored. Fourthly, the strains and data were collected 12 years ago. It is to be expected that the prevalence of resistance has increased, in line with the finding of higher prevalence among the younger group of patients, who on average have been infected more recently than older patients. The higher prevalence in more recent years from several sub-national studies in China [11,12,13,14] also support this expectation. Further studies of larger samples collected during more recent years and exploring the resistance by using of whole genome sequence may provide more accurate and deeper insights into the mechanism and associated factors of pyrazinamide resistance in China. Fortunately the strains from routine drug resistance surveillance in recent years has been collected and transferred to the Chinese National Tuberculosis Reference Laboratory and we are planning to assess the pyrazinamide resistance status and even the trend of change during these years in a subsequent study.
Conclusion
Pyrazinamide resistance among MDR-TB patients is common, especially in patients aged < 40 years in China. Pyrazinamide therefore should not be used as priority option of Group 3 drugs for treatment of RR/MDR-TB in China while awaiting scale up of new drugs and regimens including bedaquiline and linezolid if the susceptibility of pyrazinamide is not confirmed. The only pncA-based molecular method has certain value for detection of pyrazinamide resistance but is not as sensitive as molecular methods for detection of rifampin resistance such as XpertMTB/RIF. Other gene mutations conferring to pyrazinamide resistance still need to be explored to increase the predictive ability of molecular methods for pyrazinamide resistance testing.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- MDR-TB:
-
Multidrug-resistant tuberculosis
- PRs:
-
Prevalence ratios
- RR-TB:
-
Rifampin-resistant tuberculosis
- XDR-TB:
-
Extensively drug-resistant tuberculosis
References
Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant tuberculosis in China. N Engl J Med. 2012;366(23):2161–70.
Dawson R, Diacon AH, Everitt D, et al. Efficiency and safety of the combination of moxifloxacin, pretomanid (PA-824), and pyrazinamide during the first 8 weeks of antituberculosis treatment: a phase 2b, open-label, partly randomised trial in patients with drug-susceptible or drug-resistant pulmonary tuberculosis. Lancet. 2015;385(9979):1738–47.
Diacon AH, Dawson R, von Groote-Bidlingmaier F. 14-day bactericidal activity of PA-824, bedaquiline, pyrazinamide, and moxifloxacin combinations: a randomised trial. Lancet. 2012;380(9846):986–93.
Dawson R, Diacon A. PA-824 , moxifloxacin and pyrazinamide combination therapy for tuberculosis. Expert Opin Investig Drugs. 2013;22(7):927–32.
Trébucq A, Schwoebel V, Kashongwe Z, et al. Treatment outcome with a short multidrug-resistant tuberculosis regimen in nine African countries. Int J Tuberc Lung Dis. 2018;22(1):17–25.
World Health Organization. WHO consolidated guidelines on drug-resistant tuberculosis treatment. Geneva: World Health Organization; 2019.Licence: CC BY-NC-SA 3.0 IGO.
Scorpio A, Zhang Y. Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat Med. 1996;2(6):662–7.
Scorpio A, Lindholm-Levy P, Heifets L, et al. Characterization of pncA mutations in pyrazinamide-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1997;41(3):540–3.
Tarshis MS, Weed WA Jr. Lack of significant in vitro sensitivity of Mycobacterium tuberculosis to pyrazinamide on three different solid media. Am Rev Tuberc. 1953;67(3):391–5.
McDeermott W, Tompsett R. Activation of pyrazinamide and nicotinamide in acidic environment in vitro. Am Rev Tuberc. 1954;70(4):748–54.
Xia Q, Zhao LL, Li F, et al. Phenotypic and genotypic characterization of pyrazinamide resistance among multidrug-resistant Mycobacterium tuberculosis isolates in Zhejiang, China. Antimicrob Agents Chemother. 2015;59(3):1690–5.
Liu W, Chen J, Shen Y, et al. Phenotypic and genotypic characterization of pyrazinamide resistance among multidrug-resistant Mycobacterium tuberculosis clinical isolates in Hangzhou, China. Clin Microbiol Infect. 2018;24(9):1016.e1–5.
Pang Y, Zhu D, Zheng H, et al. Prevalence and molecular characterization of pyrazinamide resistance among multidrug-resistant Mycobacterium tuberculosis isolates from southern China. BMC Infect Dis. 2017;17(1):711.
Gu Y, Yu X, Jiang G, et al. Pyrazinamide resistance among multidrug-resistant tuberculosis clinical isolates in a national referral center of China and its correlations with pncA, rpsA, and panD gene mutations. Diagn Microbiol Infect Dis. 2016;84(3):207–11.
Whitfield MG, Warren RM, Streicher EM, et al. Mycobacterium tuberculosis pncA polymorphisms that do not confer pyrazinamide resistance at a breakpoint concentration of 100 micrograms per milliliter in MGIT. J Clin Microbiol. 2015;53(11):3633–5.
Kremer K, Bunschoten A, Schouls L, et al. “Spoligotyping”a PCR-based method to simultaneously detect and type Mycobacterium tuberculosis complex bacteria. National Institute of Public Health and the Environment; 2002. Available: http://nl.sitestat.com/rivm/rivm-nl/s?link.documenten_en_publicaties.professioneel_praktisch.protocollen.protocollen_mycobacterium_tuberculosis&ns_type=pdf&ns_url=http://www.rivm.nl/dsresource?objectid=bbb706c2-b8fd-4abb-835f-27b9ff364747&type=org&disposition=inline
Jonmalung J, Prammananan T, Leechawengwongs M, et al. Surveillance of pyrazinamide susceptibility among multidrug-resistant Mycobacterium tuberculosis isolates from Siriraj hospital, Thailand. BMC Microbiol. 2010;10:223.
Chiu YC, Huang SF, Yu KW, et al. Characteristics of pncA mutations in multidrug-resistant tuberculosis in Taiwan. BMC Infect Dis. 2011;11:240.
Kim HJ, Kwak HK, Lee J, et al. Patterns of pncA mutations in drug-resistant Mycobacterium tuberculosis isolated from patients in South Korea. Int J Tuberc Lung Dis. 2012;16(1):98–103.
Kurbatova EV, Cavanaugh JS, Dalton T, et al. Epidemiology of pyrazinamide-resistant tuberculosis in the United States, 1999-2009. Clin Infect Dis. 2013;57(8):1081–93.
Zignol M, Dean AS, Alikhanova N, et al. Population-based resistance of Mycobacterium tuberculosis isolates to pyrazinamide and fluoroquinolones: results from a multicountry surveillance project. Lancet Infect Dis. 2016;16(10):1185–92.
Li D, Hu Y, Werngren J, et al. Multicenter study of the emergence and genetic characteristics of pyrazinamide-resistant tuberculosis in China. Antimicrob Agents Chemother. 2016;60(9):5159–66.
Louw GE, Warren RM, Donald PR, et al. Frequency and implications of pyrazinamide resistance in managing previously treated tuberculosis patients. Int J Tuberc Lung Dis. 2006;10(7):802–7.
Stagg HR, Brown J, Ibraim E, et al. Drug susceptibility patterns in MDR-TB patients: challenges for future regimen design. A Cross-Sectional Study. PLoS One. 2015;10(11):e0142425.
Fofana MO, Shrestha S, Knight GM, et al. A Multistrain Mathematical Model To Investigate the Role of Pyrazinamide in the Emergence of Extensively Drug-Resistant Tuberculosis. Antimicrob Agents Chemother. 2017;61(3):e00498–16.
Nguyen D, Brassard P, Menzies D, et al. Genomic characterization of an endemic Mycobacterium tuberculosis strain: evolutionary and epidemiologic implications. J Clin Microbiol. 2004;42(6):2573–80.
Mortimer TD, Weber AM, Pepperell CS. Signatures of Selection at Drug Resistance Loci in Mycobacterium tuberculosis. mSystems. 2018;3(1):e00108–17.
Fonseca Lde S, Marsico AG, Vieira GB, et al. Correlation between resistance to pyrazinamide and resistance to other antituberculosis drugs in Mycobacterium tuberculosis strains isolated at a referral hospital. J Bras Pneumol. 2012;38(5):630–3.
Akhmetova A, Kozhamkulov U, Bismilda V, et al. Mutations in the pncA and rpsA genes among 77 Mycobacterium tuberculosis isolates in Kazakhstan. Int J Tuberc Lung Dis. 2015;19(2):179–84.
Marttila HJ, Marjamäki M, Vyshnevskaya E, et al. pncA mutations in pyrazinamide-resistant Mycobacterium tuberculosis isolates from northwestern Russia. Antimicrob Agents Chemother. 1999;43(7):1764–6.
Miotto P, Cabibbe AM, Feuerriegel S, et al. Mycobacterium tuberculosis pyrazinamide resistance determinants: a multicenter study. MBio. 2014;5(5):e01819–4.
Mizrahi V, Andersen SJ. DNA repair in Mycobacterium tuberculosis. What have we learnt from the genome sequence? Mol Microbiol. 1998;29(6):1331–9.
Zignol M, Cabibbe AM, Dean AS, et al. Genetic sequencing for surveillance of drug resistance in tuberculosis in highly endemic countries: a multi-country population-based surveillance study. Lancet Infect Dis. 2018 Jun;18(6):675–83.
Miotto P, Tessema B, Tagliani EA, et al. Standardised method for interpreting the association between mutations and phenotypic drug resistance in Mycobacterium tuberculosis. Eur Respir J. 2017;50(6):1701354.
Farhat MR, Sultana R, Iartchouk O, et al. Genetic determinants of drug resistance in Mycobacterium tuberculosis and their diagnostic value. Am J Respir Crit Care Med. 2016;194(5):621–30.
Tan YJ, Hu ZQ, Zhang TY, et al. Role of pncA and rpsA gene sequencing in detection of pyrazinamide resistance in Mycobacterium tuberculosis isolates from southern China. J Clin Microbiol. 2014;52(1):291–7.
Alexander DC, Ma JH, Guthrie JL, et al. Gene sequencing for routine verification of pyrazinamide resistance in Mycobacterium tuberculosis: a role for pncA but not rpsA. J Clin Microbiol. 2012;50(11):3726–8.
Zimic M, Loli S, Gilman RH, et al. A new approach for pyrazinamide susceptibility testing in Mycobacterium tuberculosis. Microb Drug Resist. 2012;18(4):372–5.
Zimic M, Fuentes P, Gilman RH, et al. Pyrazinoic acid efflux rate in Mycobacterium tuberculosis is a better proxy of pyrazinamide resistance. Tuberculosis (Edinb). 2012;92(1):84–91.
CRyPTIC Consortium and the 100,000 Genomes Project, Allix-Béguec C, Arandjelovic I, et al. Prediction of Susceptibility to First-Line Tuberculosis Drugs by DNA Sequencing. N Engl J Med. 2018;379(15):1403–15.
Willby MJ, Wijkander M, Havumaki J, et al. Detection of Mycobacterium tuberculosis pncA mutations by the Nipro Genoscholar PZA-TB II assay compared to conventional sequencing. Antimicrob Agents Chemother. 2017;62(1):e01871–17.
Acknowledgements
We are grateful to all staffs of National Tuberculosis Reference Laboratory at Chinese Center for Disease Control and Prevention for their cooperation and technical help.
Funding
This work was funded by the National Science and Technology Major Project (2014ZX10003002), National Science and Technology Major Project (2015ZX10003003) and China CDC Balance funds project (2013ZX10003–004). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
YLZ designed the study, HX, SVH, FC developed the methodology, HX YZ BZ conducted the experiments, SFW collected the clinical data, HX performed the analysis and wrote the original draft, SVH, FC, YLZ reviewed and edited the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval of this study was waived by the Ethical Committees of the Chinese Center for Disease Control and Prevention. The 2007 national drug resistance survey was approved by the Tuberculosis Research Ethics Review Committee of the Chinese Center for Disease Control and Prevention and written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Database for Univariable and multivariable analysis of risk factors for phenotypic and genotypic pyrazinamide resistance.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xia, H., van den Hof, S., Cobelens, F. et al. Value of pyrazinamide for composition of new treatment regimens for multidrug-resistant Mycobacterium tuberculosis in China. BMC Infect Dis 20, 19 (2020). https://doi.org/10.1186/s12879-020-4758-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-4758-9