Abstract
Background
Normal findings of cardiac scintigraphy predict good outcomes. However, a paucity of the data exists for elderly patients 85 years or older. In the present study, we aimed to demonstrate the association between the abnormal findings of cardiac scintigraphy and the risk of all cause death in patients 85 years or older.
Methods
We enrolled 143 consecutive patients 85 years or older with known or suspected coronary artery disease who underwent stress scintigraphy under adenosine or an exercise test and a 99mTechnetium (Tc)-labeled tracer or thallium 201 (201Tl), dual tracer rest scintigraphy using 201Tl and 123I-β-methyl iodophenyl pentadecanoic acid (123I-BMIPP), or 123I-BMIPP single tracer scintigraphy. Ischemia was defined by an induced perfusion abnormality according to a provocation test with recovery at rest or decreased uptake of 123I-BMIPP despite normal perfusion at rest. Infarction was defined by perfusion abnormalities assessed by images at rest on 201Tl or 99mTc-labeled tracer. We defined these findings as abnormal when at least one of these aforementioned characteristics was observed.
Results
Patients in the abnormal findings group (N = 62) were more likely to have undergone prior coronary angiography and to have decreased ejection fraction than those in the normal findings group (N = 81). The median follow-up duration was 797 days (interquartile range, 635–1045 days), with follow-up rates of 90% at 1 year and 73% at 2 years. The 2-year mortality rate were significantly higher in the abnormal findings group than in the normal findings group (26.8% vs. 10.9%; p = 0.01). The risk of abnormal findings relative to normal findings remained significant for the mortality (adjusted hazard ratio, 5.99; 95% CI, 1.37–42.8; P = 0.015).
Conclusion
Abnormal myocardial scintigraphy findings were associated with the increased risk for mortality, even for patients 85 years or older.
Similar content being viewed by others
Background
In developed countries, the population is aging [1]. It is estimated that the prevalence of people 65 years or older will triple from 2010 to 2050, and the oldest age group (85 years or older) will account for up to 17% of the elderly population [1]. However, in Japan, the oldest age group already reached 15% in 2017. Furthermore, due to the progress of medical therapies and revascularization techniques, the life expectancy of patients with acute coronary syndrome has improved [2]. Therefore, it is important to evaluate the ability of diagnostic testing to convey meaningful information in this group of patients. Although the significance of the normal myocardial perfusion imaging for patients 75 years or older was reported for those who were scheduled to undergo non-cardiac surgery [3, 4], there is a paucity of data for patients of more advanced age in Japan. In the present study, we aimed to evaluate the prognostic value of abnormal (or normal) scintigraphy findings for patients aged 85 years or older, which is a terminal age category of current public health [5].
Methods
Study population
We retrospectively analyzed 143 consecutive patients aged 85 years or older with known or suspected coronary artery disease who underwent stress scintigraphy under adenosine or an exercise test and 99mTechnetium (Tc)-labeled tracer or thallium-201 (201Tl), dual tracer rest scintigraphy using 201Tl and 123I-β-methyl iodophenyl pentadecanoic acid (123I-BMIPP), or 123I-BMIPP scintigraphy with normal electrocardiogram (ECG) results, at Kitano hospital from 2010 to 2013. We investigated comorbidities, the presence of typical exertional chest pain, and prior coronary angiography results, scintigraphy findings, and outcomes from their medical records. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the institutional review board of Kitano hospital. Informed consent was waived because this was a retrospective study. We disclosed the details of the present study to the public as an opt-out method and the notice clearly informed patients of their right to refuse enrollment. Follow-up data were collected by reviewing hospital charts, by contacting the referring physicians by mail, or by contacting the patients or relative. When contacted for follow-up visit, no patients refused to participate in the study viewing the opt-out statement. Patient records and information were anonymized prior to analysis.
Methods of nuclear imaging
Myocardial perfusion study using 99mTc-tetrofosmin, 99mTc-sestamibi, or 201Tl
A myocardial perfusion study was conducted using 99mTc-tetrofosmin or 99mTc-sestamibi with 259–300 MBq for the stress study and 740 MBq for the rest study, or 201Tl with 111 MBq [6]. The stress type was symptom-limited or > 85% of the maximum heart-rate exercise using a bicycle ergometer (n = 8) and pharmacological administration of adenosine (n = 88). A dual-headed single-photon emission computed tomography (SPECT) system equipped with low-energy collimators (Cannon Medical Systems Ltd., Tochigi, Japan) was used for data acquisition with a 360-degree acquisition. ECG-Gated SPECT was performed using a division of 16-frames per cardiac cycle at least at rest. We reconstructed standard short-axis and long-axis images using Butterworth and ramp filters, without scatter correction or attenuation correction. Quantitative-gated SPECT software was used to calculate left ventricular functional parameters.
Metabolic imaging using 123I-BMIP
We used 148 MBq of 123I-BMIPP. Myocardial perfusion SPECT proceeded simultaneously using 111 MBq of 201Tl (n = 16). With normal ECG findings, 123I-BMIPP without perfusion imaging was used for diagnosis (n = 31) based on the discretion of attending physicians. When using dual tracers, two separate 20% windows were centered with one on the 123I photopeak (159 KeV). and the other on the 201Tl photopeak (75 KeV). We did not apply cross-talk correction between 201Tl and 123I-BMIPP.
Definitions
Ischemia was defined by an induced perfusion abnormality according to a provocation test with recovery at rest or decreased uptake of 123I-BMIPP despite normal perfusion at rest or without information regarding perfusion but with normal electrocardiogram results. Infarction was defined by perfusion abnormalities assessed by images at rest on 201Tl or 99mTc-labeled tracer. We defined findings as normal when none of these aforementioned characteristics was observed. The defects measurements were performed by experienced one radiologist and one nuclear cardiologist. If one’s judgement is different from the other’s, the final judgement has been made after discussion. Ejection fraction according to quantitative gating was obtained when available. The presence or absence of comorbidities was based on the assessment of the attending physicians. The diagnostic modalities were selected based on the discretion of attending physicians. The primary endpoints were all-cause death. Every death was placed into one of the 2 categories: 1) cardiovascular deaths, which consist of heart failure (HF), myocardial infarction, sudden death, stroke, renal failure, aortic/peripheral vascular disease, and other cardiac cause; and 2) non-cardiovascular deaths, which include malignancy, infection, respiratory failure, liver failure, renal failure, bleeding, and trauma, and undetermined causes. Sudden death was defined as unexplained death in a previously stable patient. Undetermined cause of death was defined as non-sudden death subsequent with severe illness with undetermined etiology.
Availability of data
The datasets generated and analyzed during the current study are not publicly available due to the policy of the institutional review board of our hospital, but are available from the corresponding author on reasonable request.
Statistical analysis
Categorical variables were expressed as numbers and percentages. Continuous variables were expressed as means ± standard deviation (SD) or medians and interquartile range (IQR). Based on their distributions, the continuous variables were compared using the Student’s t-test or the Wilcoxon rank sum test between two groups.
The cumulative incidences of clinical events were estimated using the Kaplan-Meier method, and differences were assessed using the log-rank test. Multivariable Cox proportional hazards models were used to estimate the risk of abnormal findings relative to normal findings of primary outcomes. The results were expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). We selected clinically relevant risk-adjusting variables (age 90 years or older, male, the presence of chest pain, diabetes mellitus, atrial fibrillation or flutter, and ejection fraction below 60%) as the primary outcome measures. Sensitivity and specificity for all-cause mortality using myocardial scintigraphy were determined using the receiver-operating characteristic (ROC) curve method after classifying patients into four groups: grade 0 (normal findings), group 1 (ischemia), group 2 (infarction), and group 3 (ischemia plus infarction).
All statistical analyses were performed by two physicians (T.K. and M.O.) using JMP 14 (SAS Institute Inc., Cary, NC). All probability values were two-tailed, and the level of statistical significance was set at P < 0.05.
Results
Baseline clinical and imaging characteristics: normal findings group versus abnormal findings group
Patients in the abnormal findings group were less likely to be 90 years or older and more likely to have undergone coronary angiography and to have decreased ejection fraction at rest than those in the normal findings group (Table 1). Scintigraphy methods were not different between the two groups.
Clinical outcomes: normal findings group versus abnormal findings group
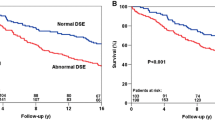
The median follow-up duration was 797 days (IQR, 635–1045 days), with follow-up rates of 90% at 1 year and 73% at 2 years. The cumulative 2-year incidences of the primary endpoints were significantly lower in the normal findings group than in the abnormal findings group (10.9% vs. 26.8%; p = 0.01) (Fig. 1). The unadjusted risk of abnormal findings relative to normal findings was 2.46 (95%CI: 1.20–5.46: P = 0.013). After adjusting for confounders, the risk of abnormal findings relative to normal findings remained significant for the primary outcome measure (HR, 5.99; 95% CI, 1.37–42.8; P = 0.015) (Table 2). Detailed information regarding the cause of mortality is provided in Table 3. Sensitivity and specificity for all-cause mortality using myocardial scintigraphy indicated that when we classified patients into four groups (grade 0, grade 1, grade 2, and grade 3), the area under the ROC curve was 0.69 (Fig. 2).
The ROC curves. Sensitivity and specificity for all-cause mortality using myocardial scintigraphy indicated that when we classified patients into four groups (grade 0: normal findings, grade 1: ischemia, grade 2: infarction, and grade 3: ischemia plus infarction), the area under the ROC curve was 0.69
Discussion
The main finding of the present study is that abnormal SPECT findings were associated with increased risk for patients 85 years or older with known or suspected coronary artery disease.
The negative predictive value of normal myocardial scintigraphy results was high in various prospective studies [7, 8]. Matsuo et al. reported that normal scintigraphy results represented a lower cardiac risk [8]. However, more than half of patients enrolled in these studies were younger than 70 years [7, 8], and patients 70 years or older were at higher risk for cardiac events compared to those younger than 70 years [8]. The novel finding in the present study is that, in the oldest patients in Japan, abnormal SPECT findings were still associated with increased risk and vice versa.
The prognostic value of SPECT has been evaluated in several studies to determine its ability to indicate abnormal findings that predict survival for elderly patients [8,9,10,11,12], and it was clearly reviewed by Patel et al. [13]. These studies comprised patients 70 years or older, 75 years or older, and 80 years or older, but not stratified by 85 years or older. Consistent with our data, the proportion who underwent stress imaging, especially exercise stress imaging, decreased with age [13]. Although coronary intervention has been shown to improve the survival of older patients with acute coronary syndromes [14], the trade-off between the risks and benefits was considered when making decisions regarding stable patients. Our data may provide useful information regarding the prognostic value of normal/abnormal findings of SPECT in patients aged 85 years or more, a terminal age category in public health, in Japan. This was consistent with the results of reports using positron emission tomographic imaging for patients 85 years or older in US and Europe [15]. Although further large-scale studies are required to provide stronger evidence, these findings will help practicing clinicians to make a diagnosis and treatment in the rapidly aging population in Japan.
We did not analyze the cardiovascular (CV) and non-CV death separately. Since the cause of death could not be clearly distinguished and the trends of normal and abnormal findings across the CV and non-CV death were consistent, we only analyzed the association of all cause death with scintigraphy findings. Non-cardiac causes of death are increasing in causes of death in older patients with CV disease [16,17,18]. An endpoint of the all cause-death may be reasonable considering the oldest patients with suspected or known CAD, as well as the those with heart failure [19]. In the present study, SPECT findings were still associated with all-cause death in oldest population, consistently with other reports in Japanese younger population [20].
There were several limitations to the present study. The main limitation of the present study was its retrospective design; therefore, selection bias may have occurred. Due to the retrospective fashion, there were no prespecified criteria for scintigraphy indications for patients with known or suspected coronary artery disease. Decisions regarding the use or non-use of diagnostic imaging and the type of diagnostic imaging used were based on the discretion of the physician. However, the physicians were experienced cardiologists who generally performed all procedures according to the guidelines for diagnosis and management of coronary artery disease. In addition, this is a single center study and there may be a classification bias about the modality selection for ischemic heart disease. Second, the tracer in the present study consisted of perfusion tracers and a metabolic tracer. Although a metabolic tracer is useful for detecting ischemia [21,22,23], we did not evaluate these modalities separately due to the small number of patients and events analyzed, the statistical power was limited. Third, we selected limited covariates for adjustment based on clinical relevance and avoidance of multi-collinearity. We have acknowledged that dyslipidemia, smoking, alcohol, diet, body mass index, and hypertension may have prognostic impacts [24, 25]; however, there was only solid evidence indicating that diabetes had a prognostic impact on patients 85 years or older [26]. Therefore, we included diabetes in the analysis. We did not include previous coronary angiography because it would have shown multi-collinearity with abnormal scintigraphy findings. Finally, due to the old age and limited numbers of individuals in the populations analyzed, the follow-up rate was relatively low despite the intensive effort. There might be some subjects who died in other hospitals, as a result we might overlook some of deaths.
Conclusion
Abnormal myocardial scintigraphy findings were associated with increased risk, even for patients 85 years or older.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 123I-BMIPP:
-
123I-β-methyl iodophenyl pentadecanoic acid
- CI:
-
Confidence interval
- ECG:
-
Electrocardiogram
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- SPECT:
-
Single-photon emission computed tomography
- Tc:
-
Technetium
- Tl:
-
Thallium
References
National Institute of Aging. Global Aging. https://www.nia.nih.gov/sites/default/files/2017-06/global_health_aging.pdf. Accessed 2 Aug 2019.
Ezekowitz JA, Kaul P, Bakal JA, Armstrong PW, Welsh RC, McAlister FA. Declining in-hospital mortality and increasing heart failure incidence in elderly patients with first myocardial infarction. J Am Coll Cardiol. 2009;53:13–20.
Bai J, Hashimoto J, Nakahara T, Suzuki T, Kubo A. Influence of ageing on perioperative cardiac risk in non-cardiac surgery. Age Ageing. 2007;36:68–72.
Koh AS, Flores JL, Keng FY, Tan RS, Chua T. Correlation between clinical outcomes and appropriateness grading for referral to myocardial perfusion imaging for preoperative evaluation prior to non-cardiac surgery. J Nucl Cardiol. 2012;19:277–84.
Boscoe FP. Subdividing the age group of 85 years and older to improve US disease reporting. Am J Public Health. 2008;98:1167–70.
JCS Joint Working Group. Guidelines for clinical use of cardiac nuclear medicine (JCS2010) - digest version. Circ J. 2012;76:761–7.
Nishimura T, Nakajima K, Kusuoka H, Yamashina A, Nishimura S. Prognostic study of risk stratification among Japanese patients with ischemic heart disease using gated myocardial perfusion SPECT: J-ACCESS study. Eur J Nucl Med Mol Imaging. 2008;35:319–28.
Matsuo S, Nakajima K, Horie M, Nakae I, Nishimura T. Prognostic value of normal stress myocardial perfusion imaging in Japanese population. Circ J. 2008;72:611–7.
Hachamovitch R, Kang X, Amanullah AM, et al. Prognostic implications of myocardial perfusion single-photon emission computed tomography in the elderly. Circulation. 2009;120:2197–206.
Nair SU, Ahlberg AW, Mathur S, Katten DM, Polk DM, Heller GV. The clinical value of single photon emission computed tomography myocardial perfusion imaging in cardiac risk stratification of very elderly patients (≥80 years) with suspected coronary artery disease. J Nucl Cardiol. 2012;19:244–55.
Yao Z, Zhu H, Li W, et al. Adenosine triphosphate stress myocardial perfusion imaging for risk stratification of patients aged 70 years and older with suspected coronary artery disease. J Nucl Cardiol. 2017;24:429–33.
Valeti US, Miller TD, Hodge DO, Gibbons RJ. Exercise single-photon emission computed tomography provides effective risk stratification of elderly men and elderly women. Circulation. 2005;111:1771–6.
Thompson RC, Patel KK. Prognosticating in the very elderly. Circ Cardiovasc Imaging. 2018;11:e008062.
Tegn N, Abdelnoor M, Aaberge L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (after eighty study): an open-label randomised controlled trial. Lancet. 2016;387:1057–65.
Erthal F, Houssain A, Dorbala S, et al. Is there an age when myocardial perfusion imaging may no longer be prognostically useful? Circ Cardiovasc Imaging. 2018;11:e007322.
Minamino-Muta E, Kato T, Morimoto T, Taniguchi T, Shiomi H, Nakatsuma K, Shirai S, Ando K, Kanamori N, Murata K, Kitai T, Kawase Y, Miyake M, Izumi C, Mitsuoka H, Kato M, Hirano Y, Matsuda S, Nagao K, Inada T, Murakami T, Takeuchi Y, Yamane K, Toyofuku M, Ishii M, Inoko M, Ikeda T, Komasa A, Tada E, Ishii K, Hotta K, Higashitani N, Jinnai T, Kato Y, Inuzuka Y, Maeda C, Morikami Y, Saito N, Sakata R, Minatoya K, Kimura T. Causes of death in patients with severe aortic stenosis: an observational study. Sci Rep. 2017;7(1):14723.
Yaku H, Ozasa N, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, Yoshikawa U, Kitai T, Taniguchi R, Iguchi M, Kato M, Takahashi M, Jinnai T, Ikeda T, Nagao K, Kawai T, Komasa A, Nishikawa R, Kawase Y, Morinaga T, Su K, Kawato M, Sasaki K, Toyofuku M, Furukawa Y, Nakagawa Y, Ando K, Kadota K, Shizuta S, Ono K, Sato Y, Kuwahara K, Kato T, Kimura T, on behalf of the KCHF Study Investigators. Demographics, management, and In-hospital outcomes of patients with hospitalized acute heart failure syndromes in the contemporary real clinical practice in Japan: Observations from the Prospective, Multicenter Kyoto Congestive Heart Failure (KCHF) registry. Circ J. 2018;82(11):2811–9.
Yamashita Y, Shiomi H, Morimoto T, Yaku H, Furukawa Y, Nakagawa Y, Ando K, Kadota K, Abe M, Nagao K, Shizuta S, Ono K, Kimura T. CREDO-Kyoto AMI Registry Investigators. Cardiac and Noncardiac Causes of Long-Term Mortality in ST-Segment-Elevation Acute Myocardial Infarction Patients Who Underwent Primary Percutaneous Coronary Intervention. Circ Cardiovasc Qual Outcomes. 2017;10(1). https://doi.org/10.1161/CIRCOUTCOMES.116.002790.
Yaku H, Kato T, Morimoto T, Inuzuka Y, Tamaki Y, Ozasa N, Yamamoto E, Yoshikawa Y, Kitai T, Taniguchi R, Iguchi M, Kato M, Takahashi M, Jinnai T, Ikeda T, Nagao K, Kawai T, Komasa A, Nishikawa R, Kawase Y, Morinaga T, Toyofuku M, Seko Y, Furukawa Y, Nakagawa Y, Ando K, Kadota K, Shizuta S, Ono K, Sato Y, Kuwahara K, Kimura T, KCHF Study Investigators. Association of Mineralocorticoid Receptor Antagonist Use by Patients Hospitalized for Acute Heart Failure With All-Cause Mortality and Heart Failure Readmission After Discharge. JAMA Netw Open. 2019;2(6):e195892.
Yoda S, Matsumoto N, Hirayama A. Clinical value of ischemia evaluation with nuclear cardiology to predict a risk of cardiovascular events: award from the 18th meeting of the Japanese Society of Nuclear Cardiology. Ann Nucl Cardiol. 2018;4:163–6.
Yoshinaga K, Matsuki T, Hashimoto A, Tsukamoto K, Nakata T, Tamaki N. Validation of automated quantitation of myocardial perfusion and fatty acid metabolism abnormalities on SPECT images. Circ J. 2011;75:2187–95.
Ohata J, Shibata S, Yoshinaga K. Fatty acid metabolism and perfusion mismatch in acute chest pain syndrome. Ann Nucl Cardiol. 2015;1:95–7.
Kato T, Izumi T, Sekihara T, Inoko M. Simultaneously-acquired myocardial perfusion, metabolism, and function after ACS. Intern Med. 2015;54:1945–6.
Shao H, Chen LQ, Xu J. Treatment of dyslipidemia in the elderly. J Geriatr Cardiol. 2011;8(1):55–64. https://doi.org/10.3724/SP.J.1263.2011.00055.
Jaul E, Barron J. Age-related diseases and clinical and public health implications for the 85 years old and over population. Front Public Health. 2017;5:335.
Odden MC, Shlipak MG, Whitson HE, Katz R, Kearney PM, defilippi C, Shastri S, Sarnak MJ, Siscovick DS, Cushman M, Psaty BM, Newman AB. Risk factors for cardiovascular disease across the spectrum of older age: the cardiovascular health study. Atherosclerosis. 2014;237(1):336–42.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
TK and MO have done the patient’s follow-up and drafted the manuscript. HY and MI have helped on the manuscript drafting and revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the institutional review board of Kitano hospital. Informed consent was waived because this was a retrospective study. We disclosed the details of the present study to the public as an opt-out method and the notice clearly informed patients of their right to refuse enrollment. The institutional review board of Kitano hospital approved the opt-out consent to participate. Follow-up data were collected by reviewing hospital charts, by contacting the referring physicians by mail, or by contacting the patients or relative. When contacted for follow-up visit, no patients refused to participate in the study by viewing the opt-out statement. We documented the opt-out consent/refusal in their medical records.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kato, T., Okano, M., Haruna, Y. et al. Association between abnormal myocardial scintigraphy findings and long-term outcomes for elderly patients 85 years or older: a retrospective cohort study. BMC Cardiovasc Disord 19, 246 (2019). https://doi.org/10.1186/s12872-019-1240-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1240-y