Abstract
Sensorineural hearing loss is a common deficit and mainly occurs due to genetic factors. Recently, copy number variants (CNVs) in the STRC gene have also been recognized as a major cause of genetic hearing loss. We investigated the frequency of STRC deletions in the Japanese population and the characteristics of associated hearing loss. For CNV analysis, we employed a specialized method of Ion AmpliSeqTM sequencing, and confirmed the CNV results via custom array comparative genomic hybridization. We identified 17 probands with STRC homozygous deletions. The prevalence of STRC homozygous deletions was 1.7% in the hearing loss population overall, and 4.3% among mild-to-moderate hearing loss patients. A 2.63% carrier deletion rate was identified in both the hearing loss and the control population with normal hearing. In conclusion, our results show that STRC deletions are the second most common cause of mild-to-moderate hearing loss after the GJB2 gene, which accounts for the majority of genetic hearing loss. The phenotype of hearing loss is congenital and appears to be moderate, and is most likely to be stable without deterioration even after the age of 50. The present study highlights the importance of the STRC gene as a major cause of mild-to-moderate hearing loss.
Similar content being viewed by others
Introduction
Sensorineural hearing loss (SNHL) is common deficit at birth, affecting approximately 2 in 1,000 births1. Genetic factors account for 50–70% of SNHL. The major form of inheritance is autosomal recessive, which accounts for 75% of cases. Approximately 100 genes have been recognized as causative factors for SNHL, with the majority of causative alterations in the genes being single nucleotide variants (SNVs) or small insertions/deletions (indels). Recently, copy number variants (CNVs) have also been found to play an important role in many human diseases including neural developmental disorders2,3. CNVs; i.e., alterations through the deletion, insertion, or duplication of approximately 1 kb or more of a gene, are thought to affect gene expression, variation in phenotype, and adaptation via gene disruption, which may impact disease traits. More recently, CNVs have been recognized as a major cause of SNHL. Shearer et al. reported that CNVs were identified in 16 of 89 hearing loss-associated genes, with the STRC gene being the most common cause of SNHL4.
The STRC gene is a known deafness-associated gene causing mild-to-moderate hearing loss, and is a part of a large deletion in chromosome 15q15.3 at the DFNB16 locus. The incidence of STRC deletions has been estimated to be between 1% and 5% in deaf populations in previous reports4,5,6,7,8. However, there have been only a few reports on hearing loss resulting from CNVs including those in the STRC gene. The interpretation of sequence data of the STRC gene is challenging due to the existence of the pseudo-STRC gene (pSTRC), which has 98% homology to the functional STRC gene. The pSTRC arose in a segmental duplication with other genes (e.g., CATSPER2 located 100 kb downstream in chromosome 15q15.3); therefore, it is thought to be difficult to detect SNVs or CNVs in this region. Further, the clinical importance of the chromosomal deletion in the region harboring STRC to CATSPER2 is associated with not only hearing loss but also infertility in males, referred to as deafness infertility syndrome, due to the fact that CATSPER2 plays essential roles in sperm motility9,10,11.
Currently, massively parallel next generation sequencing (NGS) is being widely applied to genetic testing in clinical settings, and is able to allow precise diagnosis through data annotation with specific bioinformatics pipelines. In Japan, genetic testing for SNHL using NGS has been approved for coverage by social health insurance, and is currently being performed in clinical settings12. However, CNV analysis with the NGS dataset remains challenging, and it is thought to be difficult to detect CNVs accurately, especially in case of targeted NGS for hearing loss genes alone.
In the present study, we used the NGS platform to analyze CNVs in the STRC gene, and confirmed their existence via high-resolution array genomic hybridization (aCGH) analysis of the entire STRC genomic region. The aims of the study were to estimate the prevalence of CNVs in the STRC region in a Japanese deaf population, and obtain a more precise characterization of the clinical features.
Subjects and Methods
Ethics approval
All procedures were approved by the Shinshu University Ethical Committee as well as the respective ethical committees of the other participating institutions (Approval number: 576). All methods were in accordance with the Shinshu University Ethical Committee for Human Genetic Research guidelines and regulations. Informed consent was obtained from all subjects or parents of the proband for participation in the study.
Subjects
One thousand twenty-five (1,025) Japanese subjects (age range, 0–70 years; mean, 11.8 years) from unrelated and non-consanguineous families were identified from 67 otolaryngology clinics in 28 prefectures across Japan between February 2012 and October 2015. All subjects had presumed non-syndromic bilateral SNHL. Clinical information and blood samples were obtained for each proband and for all consenting affected and unaffected relatives. Collected data included (1) pure-tone audiograms, and behavioral audiometry or auditory brain stem responses (ABR); (2) medical history, including onset of hearing loss, and progression of hearing loss; and 3) temporal bone imaging (computed tomography and/or magnetic resonance) if done. Hearing levels were classified based on the better hearing ear as normal, <20 dB; mild hearing loss, 21–40 dB; moderate hearing loss, 41–70 dB; severe hearing loss, 71–95 dB; and profound hearing loss, >95 dB. To clarify the prevalence of STRC deletions in the normal hearing population, we examined 152 normal control individuals using the same CNV analysis with the NGS dataset as used for the hearing loss subjects. The age range of each individual was 20–30 years. Ear examination and pure-tone audiometry were performed and showed normal results.
Methods
Amplicon resequencing with NGS
Amplicon libraries were prepared using an Ion AmpliSeqTM Custom Panel (Applied Biosystems, Life Technologies), per with the manufacturer’s instructions, for 68 genes reported to cause non-syndromic hereditary HL (the list of genes is shown in Supplementary Table S1). The detailed sample preparation protocol has been described elsewhere13. We analyzed 45 samples in one Ion AmpliSeqTM sequencing reaction to set 45 samples as a one-batch reaction. Sequencing was performed following the manufacturer’s instructions. NGS was performed with an Ion Torrent Personal Genome Machine system using an Ion PGMTM 200 Sequencing Kit and an Ion 318TM Chip (Life Technologies). The sequence data were mapped against the human genome sequence (build GRCh37/ hg19) with a Torrent Mapping Alignment Program. After sequence mapping, the DNA variant regions were piled up using the Torrent Variant Caller plug-in software. After variant detection, their effects were analyzed using ANNOVAR software.
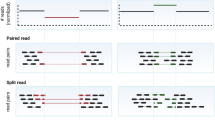
Copy number analysis in the NGS dataset
We employed our recently published specialized method for Ion AmpliSeqTM sequencing that utilizes multiplex PCR-based targeted genome enrichment14. The depth of coverage information for each amplicon included in the barcode/amplicon coverage matrix file was used for copy number analysis. Normalization of coverage data depth was performed after considering the relative value of each amplicon. After normalization and removal of outlier data, the normalized relative read depths of amplicons were sorted based on chromosome position order and separated based on chromosome and gene identity, which were then plotted as a graph using conventional spread sheet software (Microsoft ExcelTM) (Supplementary Fig. S1). All CNVs in the STRC region were curated through manual inspection from the graph.
Copy number analysis via custom array-CGH
The commercial whole-genome array-CGH provided only one probe for every 3,000–8,000 bp, and only a few probes lay across the STRC genomic region (Supplementary Fig. S2). Therefore, we designed the custom aCGH for 68 known deafness-associated genes using the Agilent database (Agilent SureDesign, Agilent Technologies, Santa Clara, CA), and the probes which lay across specific chromosomal regions of those genes at 150–200 bp intervals as a design-setting on the Agilent 8 × 60 K platform (Agilent Technologies, Santa Clara, CA)15. There were 535 probes laid across the STRC and CATSPER2 region (chr15:43600000–44330000), and probe intervals varied depend on the design platform due to highly homology of pseudogenes. We used the same DNA samples as used for amplicon resequencing, and quality assessment was also performed. Ten microliters of genomic DNA solution (0.5 µg of DNA) were fragmented, labeled with cyanine-3 for reference DNA samples and cyanine-5 for subjects, and then hybridized. Scanning of the array was carried out per the manufacturer’s recommended protocols. Scanned aCGH data were analyzed using CytoGenomics software version 3.0.6.6 (Agilent Technologies) (Supplementary Fig. S1).
Ethics approval and consent to participate
All procedures were approved by the Shinshu University Ethical Committee as well as the respective ethical committees of the other participating institutions. Informed consent was obtained from all subjects or parents of the proband for participation in this study, which was approved by the human subjects’ ethical committee of each institution.
Results
Clinical characteristics of hearing loss patients and detected CNVs
As shown in Table 1, of the 1,025 subjects (age range, 0–70 years, mean age, 11.8 years), the distribution of SNHL inheritance mode was 264, 723, and 38 for segregating autosomal dominant, autosomal recessive or sporadic, and unknown, respectively. When classified based on age of onset as congenital–6 years, 7–18 years, adulthood (>18 years old), or unknown, most of the subjects with a causative STRC deletion were diagnosed with SNHL by adolescence. We found causative homozygous STRC deletions in 14 of the 723 cases categorized as segregating autosomal recessive or sporadic (1.94%), and in 3 of the 264 cases with autosomal dominant inheritance (1.14%). We identified duplications (3 copies) of STRC in 19 subjects (1.85%). It was unclear whether the 3 STRC copies were pathogenic or had any impact on phenotypes. We also found 27 subjects with STRC heterozygous deletions defined as carrier deletions. The frequency of carrier STRC deletions was 2.63% (27/1,025) in the hearing loss cohort, which was identical (2.63%, 4/152) to that in the normal hearing controls.
Prevalence of CNVs in STRC among the subjects diagnosed with genetic hearing loss
As shown in Fig. 1, of the 1,025 subjects, the genetic causes of SNHLs were identified in 395 probands (diagnosis rate, 38%), with SNVs in GJB2 being the most commonly identified (39%) among all subjects across all forms of inheritance. CNVs implicated in homozygous deletions (2 copies) in STRC accounted for 5% (17/395) of all subjects (Fig. 1a), whereas when classified based on hearing level as mild-to-moderate or severe-to-profound, the prevalence of causative STRC deletions was 12% (17/140) in the subjects with mild-to-moderate SNHL (Fig. 1b). Consequently, CNVs in STRC were the second most common cause of mild-to-moderate SNHL after SNVs in GJB2. None of the subjects with severe-to-profound or asymmetric SNHL had disease-causing CNVs in STRC (Table 1).
Prevalence of CNVs in STRC. Among the 1,025 subjects, we identified genetic causes in 395 probands (diagnosis rate, 38%), with variants in GJB2 being the most commonly identified (39%). CNVs implicated in STRC homozygous deletions (2 copies) accounted for 5% (17/395) of all subjects (a). Prevalence of STRC homozygous deletions was 12% (17/140) in subjects with mild-to-moderate SNHL (b).
Clinical features of STRC homozygous deletions
As shown in Table 2, of the 17 subjects with STRC homozygous deletions, 7 individuals had undergone newborn hearing screening (NHS) and all had failed. Among the other individuals, hearing loss was identified at wellness checkups during elementary school years, or they became aware of hearing loss around the ages of 6 to 12. A distortion product otoacoustic emission (DPOAE, a tool for assessing cochlear status, specifically hair cell function) test has been undertaken by several individuals, and showed an absence of response indicating SNHL. The average hearing levels ranged from 28.8 to 60.8 dB, although the age at which the audiogram was taken varied (Fig. 2). Therefore, we assessed the deterioration of hearing in each individual by means of serial audiograms that were obtained every year for nine patients (Fig. 3). Figure 3 shows that hearing loss among these patients appeared to remain around the mild-to-moderate level, even in their fifties, and appeared not to deteriorate. The hearing levels showed a slight decline (y = 0.12x) and hearing deterioration was likely age-related, suggesting that it was not affected by the STRC deletion alone.
Confirmation of the STRC genomic region via array CGH
We performed array CGH for 17 probands in whom homozygous deletions in the STRC region were detected using NGS data. Fifteen cases had homozygous long deletions containing both STRC and CATSPER2 genes. Two cases (AG6087 and AH5185) showed homozygous deletions in the STRC gene, not including the CATSPER2 gene.
Supplementary Fig. S1 shows an enlarged view of the homozygous STRC and CATSPER2 deletions detected using array CGH analysis.
Discussion
In the present study, we identified homozygous deletions in the STRC genomic region leading to SNHL in 17 of 1,025 Japanese deafness cases (1.66%; 17/1,025), and heterozygous deletions in 27 subjects (2.63%), indicating that the frequency of CNVs in this region was 4.29% (44/1025). Francey et al. studied 659 probands with bilateral SNHL and identified 7 homozygous and 10 heterozygous deletions in the STRC region using SNP genotyping array; among 10 probands with heterozygous deletions, SNVs or interstitial deletions were identified on the trans-allele in 4 probands, which were defined as compound heterozygotes of CNV and SNV resulting in hearing loss5. Shearer et al. identified causative mutations in STRC including homozygous deletions, gene conversions, and heterozygous deletions in-trans leading to missense changes, in 37 out of 686 hearing loss patients (5.4%) through analysis of NGS read data in CNV detection4. Vona et al. also reported homozygous or heterozygous STRC deletions as a cause of hearing loss in 9 probands among 94 SNHL probands using whole-genome aCGH7; among 9 probands with heterozygous deletions, SNVs were identified on the trans-allele in 4 probands. In the present study, 17 out of 27 STRC deletion carriers exhibited mild-to-moderate hearing loss. We inferred that 17 carriers might have a causative SNV on the other allele in the STRC, suggesting the presence of SNV and CNV as a compound heterozygote. A limitation of our study was that we focused on identification of CNVs alone and detected gene gains or deletions in the STRC genomic region; indeed, it was likely to be more challenging to detect SNVs due to low reliability of NGS read data of the region with highly homologous pseudogenes.
The prevalence of CNVs in the STRC region might vary among different populations, or the results could be influenced by the different CNV detection methods used such as SNP array or NGS. In the present study, we undertook CNV analysis using NGS read data as a first screening step followed by confirmation with aCGH, which is thought to be a robust method for CNV detection. Whole-genome array CGH designs are based on principles described in several publications and cover targeted regions including individual disease-related genes. For the STRC gene and its surrounding region, only a few probes lay across the whole-genome CGH array. We therefore designed a custom array CGH with a high density of probes for deafness-associated genes including the STRC genomic region. We found a false-positive result in only one sample in which CNV analysis with NGS read data showed a homozygous deletion, while aCGH revealed a normal copy number. Therefore, our present findings regarding the frequency of CNVs in the STRC region in the largest cohort studied to-date, while preliminary, are thought likely to be accurate for subjects with SNHL. We were able to identify gene deletions or duplications in the STRC region, but could not detect gene conversions or balanced rearrangement. Thus, the frequency of STRC variations causing SNHL is expected to be much higher if conversions could be detected.
The frequency of carrier STRC deletions was 2.63% (4/152) in the normal hearing controls, which was identical (2.63%, 27/1,025) to that in the hearing loss cohort. The frequency of carrier mutations in the GJB2 gene, which is the most prevalent cause of autosomal recessive deafness, is reported to be approximately 2% in the normal hearing population16. Although the frequency of heterozygous GJB2 mutations is similar to that of heterozygous STRC deletions, the frequency of hearing loss due to homozygous STRC deletions is reported to be much lower than that due to homozygous/compound heterozygous GJB2 mutations. One possible reason for this discrepancy is that the detection method using NGS dataset and custom aCGH employed in this study was fundamentally challenging; however, the observed deletions were reliable. The basis for the relationship between carrier frequency and prevalence of hearing loss with STRC deletions is currently unclear.
Interestingly, we found causative homozygous STRC deletions in 3 probands (17.6%) with autosomal dominant-appearing inheritance among the 17 probands showing all forms of inheritance, indicating pseudodominant inheritance. As shown in Fig. 4, the proband AH6278 had homozygous deletions in STRC, and segregation analysis via aCGH showed that her father (YSU5044) had a homozygous deletion and that her mother (YSU5045) was a heterozygous carrier. Due to higher carrier frequency of deletions in the STRC region (2.63%; 27/1,025), it was possible to identify homozygous deletions in STRC even in families showing autosomal dominant inheritance. On the other hand, in our cohort, mutations in the GJB2 gene, which is the most prevalent cause of autosomal recessive deafness, were found to follow pseudodominant inheritance in 15 (10.1%) of 149 probands showing all forms of inheritance. The carrier frequency of the SNVs in GJB2 was previously reported to be 6.7% in Japanese bilateral SNHL populations16.
Results of custom array comparative genomic hybridization (aCGH) for the proband AH6278 and her parents. The upper panel shows a homozygous chromosomal deletion in the region containing STRC to CATSPER2 in AH6278 (proband) and YSU5044 (father), and a heterozygous deletion in the pSTRC region in YSU5045 (mother) identified using CytoGenomics software. The lower panel shows audiograms and the pedigree, indicating pseudodominant inheritance.
Approximately 70% of hereditary hearing loss patients exhibit autosomal recessive inheritance and are affected with severe-to-profound congenital SNHL. The major causative genes with recessive inheritance are GJB2, SLC26A4, and CDH23, which cause severe-to-profound congenital SNHL12,17. Most of the mutations in these genes are SNVs or small insertions/deletions (indels). The major genetic causes of mild-to-moderate SNHL in recessive inheritance remain unclear. We showed that homozygous deletions in the STRC region were identified in 17 of 398 (4.3%) mild-to-moderate SNHL subjects, and our results suggested that STRC deletions were the second most common cause of mild-to-moderate SNHL after SNVs in GJB2.
The STRC gene encodes the large extracellular structural protein stereocilin, which is expressed in the outer hair cells of the inner ear. Stereocilin is associated with the formation of tip link connectors between stereocilia and connections between outer hair cells and the tectorial membrane. Stereocilin-null mutant mice show progressive hearing loss, and their hair bundle stiffness appears decreased despite no apparent structural abnormalities18,19,20. In the present study, we observed that hearing loss did not progress to a severe level in the patients even after 50 years of age. SNHL appearing at birth is detectable via NHS; however, only 7 of 17 subjects were diagnosed with hearing loss through NHS. Indeed, NHS has been implemented since the year 2000 in Japan. NHS is not required by the law, and is provided based on the parents’ request. Therefore, we inferred that hearing loss could have been detected in all cases if NHS was universally applicable.
One region of chromosome 15q15.3 contains the STRC gene and the pseudo-STRC (pSTRC) gene, which has 98% homology to the functional STRC gene. The pSTRC gene arose in a segmental duplication with other genes (e.g., CATSPER2 located 100 kb downstream on chromosome 15q15.3). CATSPER2 is involved in sperm motility, and is responsible for driving the hyperactivated motility that is essential for fertilization10. Zhang et al. reported three unrelated Iranian families with SNHL and male infertility caused by a long deletion involving four genes (KIAA0377, CKMT1B, STRC, and CATSPER2) at chromosome 15q15.39. In the present study, we found a homozygous long deletion involving the STRC and CATSPER2 genes in 15 of 17 cases (88.2%). Consequently, patients with a STRC deletion might also possess a CATSPER2 deletion that could be involved in hearing loss and male infertility. This is important information that should be shared during genetic counseling.
In summary, we performed CNV analysis in STRC using NGS read data from the platform used for the current social health insurance-based genetic testing in Japan as a first screening step, followed by confirmation using custom aCGH. We clarified the prevalence of causative STRC deletions in a Japanese population, and our data indicate that these were the second most common cause of mild-to-moderate hearing loss, which was congenital and non-progressive in the population.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Morton, C. C. & Nance, W. E. Newborn hearing screening–a silent revolution. New England Journal of Medicine 354, 2151–2164 (2006).
Zhang, F., Gu, W., Hurles, M. E. & Lupski, J. R. Copy number variation in human health, disease, and evolution. Annual Review of Genomics and Human Genetics 10, 451–481 (2009).
Conrad, D. F. et al. Origins and functional impact of copy number variation in the human genome. Nature 464, 704–712 (2010).
Shearer, A. E. et al. Copy number variants are a common cause of non-syndromic hearing loss. Genome Medicine 6, 37 (2014).
Francey, L. J. et al. Genome-wide SNP genotyping identifies the Stereocilin (STRC) gene as a major contributor to pediatric bilateral sensorineural hearing impairment. American Journal of Medical Genetics part A. 158A, 298–308 (2012).
Hoppman, N. et al. Genetic testing for hearing loss in the United States should include deletion/duplication analysis for the deafness/infertility locus at 15q15.3. Molecular Cytogenetics 6, 19 (2013).
Vona, B. et al. DFNB16 is a frequent cause of congenital hearing impairment: implementation of STRC mutation analysis in routine diagnostics. Clinical Genetics 87, 49–55 (2015).
Plevova, P. et al. STRC deletion is a frequent cause of slight to moderate congenital hearing impairment in the Czech Republic. Otology Neurotology 38, e393–e400 (2017).
Zhang, Y. et al. Sensorineural deafness and male infertility: a contiguous gene deletion syndrome. Journal of Medical Genetics 44, 233–240 (2007).
Quill, T. A. et al. Hyperactivated sperm motility driven by CatSper2 is required for fertilization. Proceedings of the National Academy of Sciences 100, 14869–14874 (2003).
Jaiswal, D., Singh, V., Dwivedi, U. S., Trivedi, S. & Singh, K. Chromosome microarray analysis: a case report of infertile brothers with CATSPER gene deletion. Gene 542, 263–265 (2014).
Mori, K., Moteki, H., Miyagawa, M., Nishio, S. Y. & Usami, S. Social health insurance-based simultaneous screening for 154 mutations in 19 deafness genes efficiently identified causative mutations in Japanese hearing loss pPatients. PLoS One 11, e0162230 (2016).
Miyagawa et al. Massively parallel DNA sequencing successfully identifies new causative mutations in deafness genes in patients with cochlear implantation and EAS. PLoS One 8, e75793 (2013).
Nishio, S. Y., Moteki, H., Usami, S. I. Simple and efficient germline copy number variant visualization method for the Ion AmpliSeq custom panel. Molecular Genetics & Genomic Medicine. 1–9 (2018).
Moteki, H. et al. Detection and confirmation of deafness-causing copy number variations in the STRC gene by massively parallel sequencing and comparative genomic hybridization. Annals of Otology, Rhinology & Laryngology 125, 918–923 (2016).
Tsukada, K., Nishio, S. Y. & Usami, S. Deafness Gene Study Consortium. A large cohort study of GJB2 mutations in Japanese hearing loss patients. Clinical Genetics. 78, 464–470 (2010).
Miyagawa, M., Naito, T., Nishio, S. Y., Kamatani, N. & Usami, S. Targeted exon sequencing successfully discovers rare causative genes and clarifies the molecular epidemiology of Japanese deafness patients. PLoS One. 8, e71381 (2013).
Verpy, E. et al. Mutations in a new gene encoding a protein of the hair bundle cause non-syndromic deafness at the DFNB16 locus. Nature Genetics. 29, 345–349 (2001).
Verpy, E. et al. Stereocilin-deficient mice reveal the origin of cochlear waveform distortions. Nature 456, 255–258 (2008).
Verpy, E. et al. Stereocilin connects outer hair cell stereocilia to one another and to the tectorial membrane. Journal of Comparative Neurology. 519, 194–210 (2011).
Acknowledgements
We would like to express our gratitude to the probands and their family members who participated in this study. We thank the participants of the Deafness Gene Study Consortium for providing samples and clinical information [Nishio and Usami, 2015]. This study was aided by a Health and Labor Sciences Research Grant for Research on Rare and Intractable diseases and Comprehensive Research on Disability Health and Welfare from the Ministry of Health, Labor and Welfare of Japan (S.U. H29-Nanchitou(Nan)-Ippan-031), a Grant-in-Aid from Japan Agency for Medical Research and Development (AMED) (S.U. 16kk0205010h001, 15ek0109114h001), a Grant-in-Aid for Scientific Research (A) from the Ministry of Education, Science and Culture of Japan (S.U. 15H02565) and a Grant-in-Aid for Scientific Research (C) from the Ministry of Education, Science and Culture of Japan (H.M. 15K10747).
Author information
Authors and Affiliations
Contributions
Study conception & design: H.M. and S.U.; Acquisition of data: Y.Y., Y.K., H.M., K.O., R.M., S.A., K.K., M.T., H.S., N.U. and T.I.; Bioinformatics analysis: H.M. and S.N.; Array C.G.H. analysis: Y.Y., H.M., T.Y., K.W. and T.K.; Data analysis and interpretation: Y.Y. and H.M.; Writing of the manuscript: Y.Y. and H.M.; Study supervision: Y.F. and S.U. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yokota, Y., Moteki, H., Nishio, Sy. et al. Frequency and clinical features of hearing loss caused by STRC deletions. Sci Rep 9, 4408 (2019). https://doi.org/10.1038/s41598-019-40586-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40586-7
- Springer Nature Limited
This article is cited by
-
Genetic screening of a Chinese cohort of children with hearing loss using a next-generation sequencing panel
Human Genomics (2023)
-
Frequency of the STRC-CATSPER2 deletion in STRC-associated hearing loss patients
Scientific Reports (2022)
-
Genetic background in late-onset sensorineural hearing loss patients
Journal of Human Genetics (2022)
-
Evaluation of copy number variants for genetic hearing loss: a review of current approaches and recent findings
Human Genetics (2022)
-
Genetic etiology of non-syndromic hearing loss in Europe
Human Genetics (2022)