Abstract
Purpose of Review
Species of the Microsporum and Nannizzia complexes are some of the etiological agents of dermatophytosis, an important cutaneous infection that affects humans and other mammals and whose incidence is increasing worldwide. This article aims to review the pertinent knowledge about dermatophytosis, specifically with these etiological agents.
Recent Findings
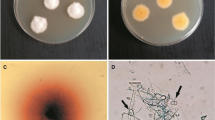
The immunological mechanisms involved in the prevention and control of these infections are not fully understood. Many reports suggest that the mammalian immune system evolved with the interaction of these pathogens, and the infection depends directly on the virulence of the strain, geographic location, and environmental resources. As virulence factors, thermotolerance, melanin production, and cell wall components stand out. Treatment for dermatophytosis includes the use of topical or systemic drugs.
Summary
These fungi present an increasing risk in human health care; studies in physiology, genetics and biochemistry, pathology of dermatophytosis, and immune response are essential for the development of new diagnostic measures, treatment protocols, and prevention strategies.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dahdah MJ, Scher RK. Dermatophytes. Curr Fungal Infect Rep. 2008;2:81–6. https://doi.org/10.1007/s12281-008-0013-3.
de Hoog S, Monod M, Dawson T, Boekhout T, Mayser P, Gräser Y. Skin fungi from colonization to infection. Microbiol Spectr. 2017;5. https://doi.org/10.1128/microbiolspec.funk-0049-2016.
• Gnat S, Łagowski D, Nowakiewicz A. Major challenges and perspectives in the diagnostics and treatment of dermatophyte infections. J Appl Microbiol 2020:jam.14611. https://doi.org/10.1111/jam.14611. This review focuses on the main problems in the diagnosis of infections caused by dermatophytes and indicates strategies and future perspectives for new identification approaches and new drugs for the control of dermatophytosis.
Begum J, Mir NA, Lingaraju MC, Buyamayum B, Dev K. Recent advances in the diagnosis of dermatophytosis. J Basic Microbiol. 2020;60:293–303. https://doi.org/10.1002/jobm.201900675 This study provides a description of the importance of rapid and accurate diagnosis of dermatophytosis, as well as the limitations of conventional methods.
Elavarashi E, Kindo AJ, Rangarajan S. Enzymatic and non-enzymatic virulence activities of dermatophytes on solid media. J Clin Diagn Res. 2017;11:DC23. https://doi.org/10.7860/JCDR/2017/23147.9410.
Flores D, Lana D, Gerardon Batista B, Alves SH, Meneghello FA. Dermatophytoses: etiologic agents, clinical forms, therapy and new perspectives of treatment. Clin Biomed Res. 2016;36:230–41. https://doi.org/10.4322/2357-9730.68880.
Hay RJ. How do dermatophytes survive in the epidermis? Curr Opin Infect Dis. 2006;19:125–6. https://doi.org/10.1097/01.qco.0000216621.98197.b4.
Leung AKC, Hon KL, Leong KF, Barankin B, Lam JM. Tinea capitis: an updated review. Recent Patents Inflamm Allergy Drug Discov. 2020;14:58–68. https://doi.org/10.2174/1872213x14666200106145624.
Al Aboud AM, Crane JS. Tinea capitis. StatPearls Publishing; 2020.
Hay RJ. Tinea Capitis: Current status. Mycopathologia. 2017;182:87–93. https://doi.org/10.1007/s11046-016-0058-8.
Mayser P, Nenoff P, Reinel D, Abeck D, Brasch J, Daeschlein G, et al. S1 guidelines: Tinea capitis. JDDG J Der Dtsch Dermatologischen Gesellschaft. 2020;18:161–79. https://doi.org/10.1111/ddg.14026.
Degreef H. Clinical forms of dermatophytosis (ringworm infection). Mycopathologia. 2008;166:257–65. https://doi.org/10.1007/s11046-008-9101-8.
Kirsten H, Haiduk J, Nenoff P, Uhrlaß S, Ziemer M, Simon JC. Tinea barbae profunda due to Trichophyton mentagrophytes : Case report and review. Hautarzt. 2019;70:601–11. https://doi.org/10.1007/s00105-019-4407-7.
Xavier MH, Torturella DM, Rehfeldt FV, Alvariño CR, Gaspar NN, Rochael MC, et al. Sycosiform tinea barbae caused by Trichophyton rubrum. Dermatol Online J. 2008;14:10.
Sahoo A, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7:77. https://doi.org/10.4103/2229-5178.178099.
Gürtler TGR, Diniz LM, Nicchio L. Microepidemia de tinha do couro cabeludo por Microsporum canis em creche de Vitória - Espírito Santo (Brasil). An Bras Dermatol. 2005;80:267–72. https://doi.org/10.1590/s0365-05962005000300007.
Gava T, Gürtler R, Martins Diniz L, Nicchio L. Microepidemia de tinha do couro cabeludo por Microsporum canis em creche de Vitória-Espírito Santo (Brasil) * Tinea capitis micro-epidemic by Microsporum canis in a day care center of Vitória-Espírito Santo (Brazil) * Caso Clínico 267. vol. 80. 2005.
Gupta AK, Mays RR, Versteeg SG, Piraccini BM, Shear NH, Piguet V, et al. Tinea capitis in children: a systematic review of management. J Eur Acad Dermatol Venereol. 2018;32:2264–74. https://doi.org/10.1111/jdv.15088.
Shy R. Tinea Corporis and Tinea Capitis. Pediatr Rev. 2007;28:164–74. https://doi.org/10.1542/pir.28-5-164.
Denk L, Tinea corporis. Pediatr. Clin Advis. 2007:562–3. https://doi.org/10.1016/B978-032303506-4.10327-X.
Kakurai M, Harada K, Maeda T, Hiruma J, Kano R, Demitsu T. Case of tinea corporis due to terbinafine-resistant Trichophyton interdigitale. J Dermatol. 2020;47:e104–5. https://doi.org/10.1111/1346-8138.15243.
Sahu P, Dayal S, Mawlong P, Punia P, Sen R. Tinea corporis bullosa secondary to trichophyton verrucosum: A newer etiological agent with literature review. Indian J Dermatol. 2020;65:76–8. https://doi.org/10.4103/ijd.IJD_483_19.
Licata G, Gambardella A, De Rosa A, Alfano R, Argenziano G. A case of tinea corporis by Epidermophyton floccosum mimicking Herpes zoster. G Ital Dermatol Venereol. 2020. https://doi.org/10.23736/S0392-0488.19.06435-6.
Saxena V, Shenoy M, Devrari J, Pai V, Agrawal V. A mycological study of tinea corporis: A changing epidemiological trend from Trichophyton rubrum to Trichophyton mentagrophytes in India. Indian J Dermatol Venereol Leprol. 2020;0:0. https://doi.org/10.4103/ijdvl.ijdvl_766_17.
Gupta AK, Chaudhry M, Elewski B. Tinea corporis, tinea cruris, tinea nigra, and piedra. Dermatol Clin. 2003;21:395–400. https://doi.org/10.1016/S0733-8635(03)00031-7.
Pippin MM, Madden ML. Tinea Cruris. 2020.
Hazlianda C, Muis K, Lubis I. A comparative study of polymerase chain reaction-restriction fragment length polymorphism and fungal culture for the evaluation of fungal species in patients with Tinea Cruris. Open Access Maced J Med Sci. 2017;5:844–7. https://doi.org/10.3889/oamjms.2017.197.
Otero L, Palacio V, Vázquez F. Tinea cruris in female prostitutes. Mycopathologia. 2002;153:29–31. https://doi.org/10.1023/A:1015257320824.
Alkeswani A, Duncan JR, Theos A. Tinea faciei starting at day two of life. Pediatr Dermatol. 2018;36:pde.13724. https://doi.org/10.1111/pde.13724.
Yamada A, Noguchi H, Sakae H, Ogawa Y, Hiruma M. Tinea faciei caused by Trichophyton verrucosum in a 20-month-old female: Case report and summary of reported cases in Japan. J Dermatol. 2012;39:667–9. https://doi.org/10.1111/j.1346-8138.2011.01369.x.
Kobayashi H. Tinea corporis and tinea pedis. Jpn J Med Mycol. 2011;52:177–81. https://doi.org/10.3314/mmj.52.177.
Veraldi S, Schianchi R, Benzecry V, Gorani A. Tinea manuum: A report of 18 cases observed in the metropolitan area of Milan and review of the literature. Mycoses. 2019;62:604–8. https://doi.org/10.1111/myc.12914.
Drira I, Neji S, Hadrich I, Sellami H, Makni F, Ayadi A. Tinea manuum due to Trichophyton erinacei from Tunisia. J Mycol Med. 2015;25:200–3. https://doi.org/10.1016/j.mycmed.2015.05.001.
Choi E, Huang J, Chew KL, Jaffar H, Tan C. Pustular tinea manuum from Trichophyton erinacei infection. JAAD Case Reports. 2018;4:518–20. https://doi.org/10.1016/j.jdcr.2018.01.019.
Asz-Sigall D, Tosti A, Arenas R. Tinea Unguium: Diagnosis and Treatment in Practice. Mycopathologia. 2017;182:95–100. https://doi.org/10.1007/s11046-016-0078-4.
Leung AKC, Leong KF, Lam JM. Tinea imbricata: an overview. Curr Pediatr Rev. 2019;15:170–4. https://doi.org/10.2174/1573396315666190207151941.
Teo TSP, Crawford LC, Pilch WT, Carney B, Solanki N, Kidd SE, et al. Mycetoma caused by Microsporum canis in a patient with renal transplant: a case report and review of the literature. Transpl Infect Dis. 2021;23:e13516. https://doi.org/10.1111/TID.13516.
Kwon-Chung KJ, Bennett JE. Medical mycology. Rev Inst Med Trop Sao Paulo. 1992;34:504–4. https://doi.org/10.1590/S0036-46651992000600018.
Sybren G, Karolina H, Michel D, Ann M, Dirk P, Marijke S, et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 2017;182:5–31. https://doi.org/10.1007/s11046-016-0073-9.
Enoch DA, Yang H, Aliyu SH, Micallef C. The changing epidemiology of invasive fungal infections. Methods Mol. Biol., vol. 1508, Humana Press Inc.; 2017, p. 17–65. https://doi.org/10.1007/978-1-4939-6515-1_2.
Martínez E, Ameen M, Tejada D, Arenas R. Microsporum spp. onychomycosis: disease presentation, risk factors and treatment responses in an urban population. Brazilian. J Infect Dis. 2014;18:181–6. https://doi.org/10.1016/j.bjid.2013.08.005.
da Cunha MM, Capote-Bonato F, Capoci IRG, Bonato DV, Ghizzi LG, Paiva-Lima P, et al. Epidemiological investigation and molecular typing of dermatophytosis caused by Microsporum canis in dogs and cats. Prev Vet Med. 2019;167:39–45. https://doi.org/10.1016/j.prevetmed.2019.03.019.
Gnat S, Łagowski D, Nowakiewicz A, Zięba P. Tinea corporis by Microsporum canis in mycological laboratory staff: unexpected results of epidemiological investigation. Mycoses. 2018;61:945–53. https://doi.org/10.1111/myc.12832.
Yu J, Wan Z, Chen W, Wang W, Li R. Molecular typing study of the Microsporum canis strains isolated from an outbreak of tinea capitis in a school. Mycopathologia. 2004;157:37–41. https://doi.org/10.1023/b:myco.0000012221.66851.68.
Ali S, Gajjala S, Raj A. Study of prevalence of dermatophytes among human immunodeficiency virus/AIDS patients in Shadan Institute of Medical Sciences and Teaching Hospital and Research Centre, Hyderabad, Telangana, India. Indian J Sex Transm Dis AIDS. 2018;39:98. https://doi.org/10.4103/ijstd.ijstd_103_16.
Skerlev M, Miklić P. The changing face of Microsporum spp infections. Clin Dermatol. 2010;28:146–50. https://doi.org/10.1016/j.clindermatol.2009.12.007.
García-Martos P, Ruiz-Aragón J, García-Agudo L, Linares M. Dermatophytoses due to Microsporum gypseum: report of eight cases and literature review. Rev Iberoam Micol. 2004;21:147–9.
Luque A, Biasoli M, Sortino M, Lupo S, Bussy R. Atypical tinea corporis caused by Microsporum gypseum in a subject with acquired immune deficiency syndrome. J Eur Acad Dermatol Venereol. 2001;15:374–5. https://doi.org/10.1046/j.0926-9959.2001.00294-14.x.
Giudice MC, Szeszs MW, Scarpini RL, Ninomyia A, Trifilio MO, Pinto WP, et al. Clinical and epidemiological study in an AIDS patient with Microsporum gypseum infection. Rev Iberoam Micol. 1997;14:184–7.
Singh I, Dixit AK, Kushwaha RKS. Antagonism of Microsporum species by soil fungi. Mycoses. 2010;53:32–9. https://doi.org/10.1111/j.1439-0507.2008.01656.x.
Soankasina AH, Rakotozandrindrainy N, Andrianteloasy S, Zafindraibe NJ, Rasamoelina T, Rafalimanana C, et al. Dermatophyte infection caused by Nannizzia gypsea: A rare case report from Madagascar. Med Mycol Case Rep. 2018;20:7–9. https://doi.org/10.1016/j.mmcr.2017.12.001.
Martinez-Rossi NM, Peres NTA, Rossi A. Antifungal resistance mechanisms in dermatophytes. Mycopathologia. 2008;166:369–83. https://doi.org/10.1007/s11046-008-9110-7.
Martinez-Rossi NM, Peres NTA, Rossi A. Pathogenesis of dermatophytosis: sensing the host tissue. Mycopathologia. 2017;182:215–27. https://doi.org/10.1007/s11046-016-0057-9.
de la Calle-Rodríguez N, Santa-Vélez C, Cardona-Castro N. Factores de virulencia para la infección de tejidos queratinizados por Candida albicans y hongos dermatofitos. Rev CES Med. 2012;26:43–55.
Muszewska A, Piłsyk S, Perlí nska-Lenart U, Kruszewska JS. Diversity of cell wall related proteins in human pathogenic fungi 2017. https://doi.org/10.3390/jof4010006.
Fisher MC, Gurr SJ, Cuomo CA, Blehert DS, Jin H, Stukenbrock EH, et al. Threats posed by the fungal kingdom to humans, wildlife, and agriculture downloaded from 2020. https://doi.org/10.1128/mBio.
Mercer DK, Stewart CS. Keratin hydrolysis by dermatophytes. Med Mycol. 2019;57:13–22. https://doi.org/10.1093/MMY/MYX160.
Cesar Viani F, Regina Cazares Viani P, Nelly Gutierrez Rivera I, Gonçalves da Silva É, Rodrigues Paula C, Gambale W. Extracellular proteolytic activity and molecular analysis of Microsporum canis strains isolated from symptomatic and asymptomatic cats. vol. 24. 2007.
Cole MF. Unifying microbial mechanisms. Garland. Science. 2019. https://doi.org/10.1201/9780429262777.
Hamaguchi T, Morishita N, Usui R, Takiuchi I. Characterization of an extracellular keratinase from Microsporum canis. Nippon Ishinkin Gakkai Zasshi. 2000;41:257–62. https://doi.org/10.3314/JJMM.41.257.
Ramos MLM, Coelho RA, Brito-Santos F, Guimarães D, Premazzi M, Zancopé-Oliveira RM, et al. Comparative analysis of putative virulence-associated factors of Microsporum canis isolates from human and animal patients. Mycopathologia. 2020;185:665–73. https://doi.org/10.1007/s11046-020-00470-9.
Kibbler CC, Barton R, Gow NAR, Howell S, Maccallum DM, Manuel RJ. Fungal cell structure and organization. 2018. https://doi.org/10.1093/med/9780198755388.001.0001.
Nosanchuk JD, Casadevall A. The contribution of melanin to microbial pathogenesis. Cell Microbiol. 2003;5:203–23. https://doi.org/10.1046/j.1462-5814.2003.00268.x.
Eisenman HC, Casadevall A. Synthesis and assembly of fungal melanin. Appl Microbiol Biotechnol. 2012;93:931–40. https://doi.org/10.1007/s00253-011-3777-2.
Eisenman HC, Frases S, Nicola AM, Rodrigues ML, Casadevall A. Vesicle-associated melanization in Cryptococcus neoformans. Microbiology. 2009;155:3860–7. https://doi.org/10.1099/mic.0.032854-0.
Youngchim S, Hay RJ, Hamilton AJ. Melanization of Penicillium marneffei in vitro and in vivo. Microbiology. 2005;151:291–9. https://doi.org/10.1099/mic.0.27433-0.
Romero-Martinez R, Wheeler M, Guerrero-Plata A, Rico G, Torres-Guerrero H. Biosynthesis and functions of melanin in Sporothrix schenckii. Infect Immun. 2000;68:3696–703. https://doi.org/10.1128/IAI.68.6.3696-3703.2000.
Nosanchuk JD, Gómez BL, Youngchim S, Díez S, Aisen P, Zancopé-Oliveira RM, et al. Histoplasma capsulatum synthesizes melanin-like pigments in vitro and during mammalian infection. Infect Immun. 2002;70:5124–31. https://doi.org/10.1128/IAI.70.9.5124-5131.2002.
Youngchim S, Pornsuwan S, Nosanchuk JD, Dankai W, Vanittanakom N. Melanogenesis in dermatophyte species in vitro and during infection. 2011;157:2348–56. https://doi.org/10.1099/mic.0.047928-0.
Malavazi I, Goldman GH, Brown NA. The importance of connections between the cell wall integrity pathway and the unfolded protein response in filamentous fungi. Br Funct Genomics. 2014;13:456.
Osherov N, Yarden O. The cell wall of filamentous fungi. Cell Mol Biol. 2014:224–37. https://doi.org/10.1128/9781555816636.ch17.
Rashid Achterman R, White TC. Dermatophyte virulence factors: identifying and analyzing genes that may contribute to chronic or acute skin infections. Int. J Microbiol. 2012;2012. https://doi.org/10.1155/2012/358305.
Kurokawa CS, Sugizaki MF, Peraçoli MTS. Virulence factors in fungi of systemic mycoses. Rev Inst Med Trop Sao Paulo. 1998;40:125–35. https://doi.org/10.1590/s0036-46651998000300001.
Percival SL, Emanuel C, Cutting KF, Williams DW. Microbiology of the skin and the role of biofilms in infection. Int Wound J. 2012;9:14–32. https://doi.org/10.1111/j.1742-481X.2011.00836.x.
Flemming HC, Wingender J. The biofilm matrix. Nat Rev Microbiol. 2010;8:623–33. https://doi.org/10.1038/nrmicro2415.
Ramage G, Rajendran R, Sherry L, Williams C. Fungal biofilm resistance. Int. J Microbiol. 2012;2012:14. https://doi.org/10.1155/2012/528521.
Danielli LJ, Lopes W, Vainstein MH, Fuentefria AM, Apel MA. Biofilm formation by Microsporum canis. Clin Microbiol Infect. 2017;23:941–2. https://doi.org/10.1016/j.cmi.2017.06.006.
Costa-Orlandi CB, Sardi JCO, Santos CT, Fusco-Almeida AM, Mendes M. In vitro characterization of Trichophyton rubrum and T. mentagrophytes biofilms. Biofouling. 2014;30:719–27. https://doi.org/10.1080/08927014.2014.919282.
Brilhante RSN, Aguiar L de, Sales JA, Araújo G dos S, Pereira VS, Pereira-Neto W de A, et al. Ex vivo biofilm-forming ability of dermatophytes using dog and cat hair: an ethically viable approach for an infection model. Biofouling 2019;35:392–400. https://doi.org/10.1080/08927014.2019.1599361.
Chen B, Sun Y, Zhang J, Chen R, Zhong X, Wu X, et al. In vitro evaluation of photodynamic effects against biofilms of dermatophytes involved in onychomycosis. Front Microbiol. 2019;10. https://doi.org/10.3389/fmicb.2019.01228.
Nogueira Brilhante RS, Correia EEM, De Melo Guedes GM, Pereira VS, De Oliveira JS, Bandeira SP, et al. Quantitative and structural analyses of the in vitro and ex vivo biofilm-forming ability of dermatophytes. J Med Microbiol. 2017;66:1045–52. https://doi.org/10.1099/jmm.0.000528.
Brilhante RSN, Correia EEM, Guedes GM de M, de Oliveira JS, Castelo-Branco D de SCM, Cordeiro R de A, et al. In vitro activity of azole derivatives and griseofulvin against planktonic and biofilm growth of clinical isolates of dermatophytes. Mycoses 2018;61:449–454. https://doi.org/10.1111/myc.12763.
•• Celestrino GA, Veasey JV, Benard G, Sousa MGT. Host immune responses in dermatophytes infection. Mycoses 2021;64:477–83. https://doi.org/10.1111/MYC.13246. This review describes the main findings about the immune response against dermatophytes and points out gaps in this knowledge.
Gnat S, Łagowski D, Nowakiewicz A, Zięba P. Phenotypic characterization of enzymatic activity of clinical dermatophyte isolates from animals with and without skin lesions and humans. J Appl Microbiol. 2018;125:700–9. https://doi.org/10.1111/jam.13921.
Chinnapun D. Virulence factors involved in pathogenicity of dermatophytes. vol. 12. 2015.
Khurana A, Sardana K, Chowdhary A. Antifungal resistance in dermatophytes: recent trends and therapeutic implications, vol. 132: Academic Press Inc.; 2019. https://doi.org/10.1016/j.fgb.2019.103255.
Kaul S, Yadav S, Dogra S. Treatment of dermatophytosis in elderly, children, and pregnant women. Indian Dermatol Online J. 2017;8:310. https://doi.org/10.4103/idoj.idoj_169_17.
Filho ST, Cucé LC, Foss NT, Marques SA, Santamaria JR. Efficacy, safety and tolerability of terbinafine for Tinea capitis in children: Brazilian multicentric study with daily oral tablets for 1, 2 and 4 weeks. J Eur Acad Dermatol Venereol. 1998;11:141–6. https://doi.org/10.1111/j.1468-3083.1998.tb00767.x.
Bar J, Samuelov L, Sprecher E, Mashiah J. Griseofulvin vs terbinafine for paediatric tinea capitis: when and for how long. Mycoses. 2019;62:949–53. https://doi.org/10.1111/myc.12970.
Calles Monar PS, Juárez MA. Eyelid tinea with blepharitis due to Microsporum canis. Arch Soc Esp Oftalmol. 2018;93:491–3. https://doi.org/10.1016/j.oftal.2018.04.005.
Gupta AK, Dlova N, Taborda P, Morar N, Taborda V, Lynde CW, et al. Once weekly fluconazole is effective in children in the treatment of tinea capitis: a prospective, multicentre study. Br J Dermatol. 2000;142:965–8. https://doi.org/10.1046/j.1365-2133.2000.03479.x.
Ginter-Hanselmayer G, Smolle J, Gupta A. Itraconazole in the treatment of tinea capitis caused by Microsporum canis: experience in a large cohort. Pediatr Dermatol. 2004;21:499–502. https://doi.org/10.1111/j.0736-8046.2004.21419.x.
Tanz RR, Hebert AA, Esterly NB. Treating tinea capitis: should ketoconazole replace griseofulvin? J Pediatr. 1988;112:987–91. https://doi.org/10.1016/S0022-3476(88)80232-4.
Moriello KA. In vitro efficacy of shampoos containing miconazole, ketoconazole, climbazole or accelerated hydrogen peroxide against Microsporum canis and Trichophyton species. J Feline Med Surg. 2017;19:370–4. https://doi.org/10.1177/1098612X15626197.
Dias M, Quaresma-Santos M, Bernardes-Filho F, Amorim A, Schechtman RC, Azulay DR. Update on therapy for superficial mycoses: review article part I. An Bras Dermatol. 2013;88:764–74. https://doi.org/10.1590/abd1806-4841.20131996.
Olson JM, Belgam Syed SY, Goyal A. Microtubule assembly inhibitors (Griseofulvin): StatPearls Publishing; 2020.
Scorzoni L, de Paula e Silva ACA, Marcos CM, Assato PA, de Melo WCMA, de Oliveira HC, et al. Antifungal therapy: new advances in the understanding and treatment of mycosis. Front Microbiol 2017;8:36. https://doi.org/10.3389/fmicb.2017.00036.
Yamada T, Maeda M, Alshahni MM, Tanaka R, Yaguchi T, Bontems O, et al. Terbinafine resistance of Trichophyton clinical isolates caused by specific point mutations in the squalene epoxidase gene. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/AAC.00115-17.
Majid I, Sheikh G, Kanth F, Hakak R. Relapse after oral terbinafine therapy in dermatophytosis: a clinical and mycological study. Indian J Dermatol. 2016;61:529. https://doi.org/10.4103/0019-5154.190120.
Martinez-Rossi NM, Bitencourt TA, Peres NTA, Lang EAS, Gomes EV, Quaresemin NR, et al. Dermatophyte resistance to antifungal drugs: mechanisms and prospectus. Front Microbiol. 2018;9. https://doi.org/10.3389/fmicb.2018.01108.
Abu El-Hamd M, Abd Elhameed MI, Shalaby MFM, Saleh R. In vitro antifungal susceptibility testing of fungi in patients with onychomycosis. Dermatol Ther. 2020;33. https://doi.org/10.1111/dth.13429.
Hsiao Y-HH, Chen C, Han HS, Kano R, Siew HANH, Kano R. The first report of terbinafine resistance Microsporum canis from a cat. Jpn Soc Vet Sci. 2018;80. https://doi.org/10.1292/jvms.17-0680.
Dogra S, Shaw D, Rudramurthy S. Antifungal drug susceptibility testing of dermatophytes: laboratory findings to clinical implications. Indian Dermatol Online J. 2019;10:225. https://doi.org/10.4103/idoj.idoj_146_19.
Brauer VS, Rezende CP, Pessoni AM, De Paula RG, Rangappa KS, Nayaka SC, et al. Antifungal agents in agriculture: friends and foes of public health. Biomolecules. 2019;9. https://doi.org/10.3390/biom9100521.
Fisher MC, Hawkins NJ, Sanglard D, Gurr SJ. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science. 2018;360:739–42. https://doi.org/10.1126/science.aap7999.
Funding
This work was supported by the Brazilian agencies Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tropical Mycoses
Rights and permissions
About this article
Cite this article
Junior, D.C., Ramos, M.L.M., Almeida-Paes, R. et al. New Insights in Dermatophytes: Microsporum spp. and Nannizzia spp.. Curr Trop Med Rep 9, 15–27 (2022). https://doi.org/10.1007/s40475-022-00252-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-022-00252-x