Abstract
Pharmacovigilance is concerned with the detection, assessment, understanding, and prevention of adverse reactions to medicines. It is helpful to prevent undesired harm sustained by the patient due to inappropriate or unsafe use of medicinal agents. As the use of drugs and polypharmacy increase in prevalence, pharmacovigilance gains relevance and momentum. Practice-based research networks have the potential to enhance health research by promoting earlier detection of adverse events at a decreased level of cost. This article explores the recent evidence of an improved benefit of administering non-steroidal antiinflammatory drugs (NSAIDs) in the fasting state, and authors propose that an improved pharmacovigilance system is both needed and feasible provided records are adapted to a nationwide integration of pharmacoepidemiology data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The concern for quality of care and sustainability of the health system has been one of the top priorities for health policy during the last decade. The relevance of primary health care in a health system is now unquestionable and its pivotal role indisputable. The Patient-Centered Medical Home initiative is one recent example of this [1]. However, its importance is not restricted to clinical care, but should also be extended to clinical research [2]. As it is well known, research is needed to improve the quality of care provided, both in the present (Are we delivering state-of-the-art care?) and into the future (How can we improve state-of-the-art clinical practice?). Indeed, quality of care is more about implementing an operative learning system inside an institution than implementing someone else’s lessons [3].
Therefore, the focus on quality care requires promoting research, as current standards of care are far from optimal. One example of this comes from a recent systematic review comparing oral analgesics in fed and fasting states [4]. The fed state reduced maximum plasma concentration of acetylsalicylic acid, ibuprofen, diclofenac, and acetaminophen (paracetamol) from 15 to 56 % of the corresponding fasting maximum concentration. Accordingly, time to maximum plasma concentration was also increased in the fed state (from 1.30 to 2.80 times longer than in the fasting state) for those same analgesic drugs. These pharmacokinetic differences are expected to impact therapeutic efficacy. If high-quality large-scale evidence were available on the efficiency of analgesic drugs for patients taking them in different conditions (namely fasted and fed states), this could have been suspected and investigated earlier.
Pharmacological relief of pain is one of the most illustrative examples of how medicine as a discipline came to improve human suffering. Empathy to those in pain and the inquisitive spirit have been the founding stones for the building of knowledge on the physiological phenomena underlying pain sensation and its pharmacological control. This (so far unfinished) body of expertise is responsible for one of the most important contributions of medicine to human existence: the relief of painful experiences. Since the public demonstration of analgesia in a medical context (at the Ether Dome, Massachusetts General Hospital, Boston) in 1846 by William T.G. Morton with diethyl ether, innumerous other substances have been developed and used in the control of painful sensations. Whether it is in the trauma context, in the operating room, or during the exacerbation of chronic back pain, just to name a few, pharmacological pain control is mandatory and its absence is carelessness. Not surprisingly, analgesics are the most prescribed categories of drugs by far [5]. There have been international guidelines for several decades and the analgesic ladder is deeply rooted in the prescribing rationale of every practitioner [6].
Despite all this evolution, current knowledge has been insufficient to assure immutability to certain practices. Moore et al. have proposed that nonsteroidal anti-inflammatory drugs (NSAIDs) be given in the fasting state owing to its improved pharmacokinetic advantage [4]. Even though this is in accordance to what has been known for ages in pharmacokinetic terms, it does not correspond to what has been proposed for gastroduodenal adverse effects’ sake—it is generally accepted that NSAIDs should be administered in the fed state. If an increase in efficiency is paralleled with a reduction in dosing and this latter fact means a reduced risk of gastrointestinal issues, then NSAIDs administration in the fasting state ought to be seriously considered.
This simple shift in paradigm comes to exemplify the major importance of being attentive to the outcomes of our practice, which should make us strive for integration of each and every single piece of clinical information. Whether patient A coped well with drug X, patient B had no improvement with drug Y or patient C reported certain side effects with drug Z, all these individual pieces of information should be compiled into some common database of medical records where these variables can be collectively appreciated. Furthermore, a tool to estimate the probability of an adverse drug reaction like the ten-item algorithm from Naranjo et al. [7] should also be incorporated. Such a data repository can derive from practice-based research networks, which can indeed provide invaluable pharmacoepidemiological information [2, 8]. In order to comply with principles of good clinical practice, such data repository must not include individual pieces of information that could identify patients (e.g., name, detailed address, identification card number, etc.). Only variables of medical interest, including those that may be of help in spotting protective or risk features for treatment response or complications, are warranted. The development of such record at a nationwide level would compete with large-scale observational studies at incredibly lower costs. The infrastructure of practice-based research networks would also be advantageous to both patients and pharmaceutical companies as it would accelerate the detection of safety issuesunidentified at earlier stages of development as well as anticipate assessment of efficacy in a relatively controlled environment.
This central data repository should not receive inputs only from health professionals. Electronic health records (EHR) are an opportunity to put into practice a proactive approach to medical information collection, not only reminding doctors to assess the effects of prescriptions at a later appointment but also by acquiring data directly at the patient level, promoting empowerment and responsibility among patients and carers [9]. This would truly be a person-centric approach to health care and research [2].
Practice-based research networks can bring further advantage by promoting detection and reporting of medical errors. Medical incidents and adverse events in primary care/general practice are erroneously at a very low level [10]. This is probably a consequence of both ineffective reporting mechanisms and fragmented levels of information. Without a major focus on quality assessment and safety incidents reporting, the opportunity to improve practices will be postponed until key messages are made clear by other sources of evidence. The amount of time we are willing to wait for these feedback mechanisms to be fully operational depends entirely on us, health care professionals. Indeed, a considerable amount of effort has been dedicated to patient safety for decades now. However, we believe that further individual adherence to incident reporting will only be achieved with promotion of an effective nationwide EHR. We should urge national and international health authorities to put forward legal requirements on feedback mechanisms of medical practice.
Despite scientific reasoning, nature reaffirms its complexity by proving medical knowledge imperfect once again. Against all odds, and after such a long experience with its prescription, we are close to changing the paradigm of NSAIDs’ prescription. This should engage the medical community in a nationwide project of integrating clinical practice data for epidemiological purposes. Such an effort of reporting would be of substantial relevance to both patient safety and clinical governance issues. And not only would current use drugs benefit from an improved surveillance system, but also brand new medicines, biological products, and medical devices in general. Indeed, the Sentinel Initiative by the United States’ Food and Drug Administration was established with this same goal. This programme was devised after the foundation of FDA’s Critical Path Initiative in 2004 with the publication of the landmark report Innovation/Stagnation: Challenge and Opportunity on the Critical Path to New Medical Products, which raised concerns and proposed solutions for the growing crisis in moving basic discoveries to the market [11]. This document was followed by the Critical Path Opportunities List, which identified specific activities that could improve the accuracy of tests that predict the safety and efficacy of potential medical products [12].
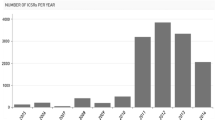
Such initiatives and supporting technologies are making it possible to implement cutting-edge information systems critical to fostering public health safety. An example of this is the Mini-Sentinel safety pilot program, the pioneer project towards a nationwide rapid-response electronic safety surveillance system for drugs and other medical products [13]. As of the first trimester of 2014, it already included over 30 collaborating healthcare institutions, nearly 100 million patients, 2.4 billion medical encounters, and 2.9 billion prescription drug dispensings [14]. An endeavor of such magnitude will be retrieving precious information from everyday clinical data that will complement existing systems already in place to track reports of adverse events linked to the use of regulated products. However, stakeholders ought not to be shortsighted and it is imperative that long-run projects are devised. Nationwide electronic health records and updated metrics for health outcomes must be put in place so that practitioners are captivated to use them. According to each type of prescription made or diagnosis coded, a pop-up menu should allow the physician (or the patient him/herself) to introduce data such as an international prostate symptom score in men with low-urinary tract symptoms, a modified medical research council score for dyspnea in chronic obstructive pulmonary disease patients, a score for any of the available pain assessment scales for patients with pain, a patient health questionnaire score for depressive mood patients or several other state-of-the-art metrics. This could be driven by an intrinsic clinical utility deriving from several different aspects: prescription guidelines often use quantified data that can be integrated and analyzed by input data and used to create alerts and recommendations. There are innumerous examples of these advantages, and we elaborate further on only two: low-density lipoprotein cholesterol levels can be easily calculated from inputted total cholesterol, high-density lipoprotein and triglyceride levels, as well as a cardiovascular risk score estimated, and both used for sorting an adequate pharmacologic treatment option. Several electronic health systems allow for input of data, calculation of risk and suggesting treatment options, but none of them propose treatment options based on the comparison of individual features (like age, gender, weight, height, previous response to other drugs) to a real-time collecting data system. Another example can be derived from sleep complaints. The several therapeutic options can be daunting and a more sound decision can be made if a clue to the tolerability to trazodone, mirtazapine or melatonin, for example, can be anticipated (which is intimately dependent on the liver microsomal metabolic profile). Therefore, clinical usefulness would be by itself the major driving force for incorporating individual tolerability data into the already busy clinical workflow. The aim for the extra effort needed for this task must come from the direct and indirect clinical utility of the information, and research gains are derived from a better-informed medical practice.
Moreover, even in the case of screening tools that are not evidence-based for clinical use, performing a clinical trial with such a reporting system in place would reduce costs and provide important clinical data in a much shorter time frame when compared to current research networks.
Nine active surveillance systems throughout the world have been described as aiming to generate post-marketing drug safety information [15]. Only one of these is active in the European Union and none is active in Portugal, at the present time. The European Union—Adverse Drug Reaction Alliance has emerged as a collaborative framework for drug safety studies, but is still far from using real-time data to provide therapeutic advice to practitioners. This should be the aim of congregated effort bridging political, health care and patient stakeholders, in the best of patient’s interests.
This kind of proposal exemplifies the type of value-based contribution that can only be made by physicians and that is the type of leadership and engagement that can be worthwhile and cost-saving and has the potential to transform health care delivery. Such a value-based system is to be grounded in three fundamental principles: (1) the goal is value for patients, (2) health care delivery is organized around medical conditions and care cycles, and (3) results are measured [16]. This is not to be found only in dreaming or wishful thinking but can be legitimately pursued and accomplished in less than a decade.
This article does not contain any new studies with human or animal subjects performed by any of the authors.
References
American Academy of Family Practice and Robert Graham Center. The patient centered medical home: history, seven core features, evidence and transformational change. Robert Graham Center: Washington, DC; 2007.
Curro FA, et al. Person-centric clinical trials: an opportunity for the good clinical practice (GCP)-practice-based research network. J Clin Pharmacol. 2013;53(10):1091–4.
Crabtree BF, et al. Summary of the national demonstration project and recommendations for the patient-centered medical home. Ann Fam Med. 2010;8:S80–90.
Moore A, et al. Effects of food on pharmacokinetics of immediate release oral formulations of aspirin, dipyrone, paracetamol, and NSAIDs—systematic review. Br J Clin Pharmacol. 2015;80(3):381–8.
Ambulatory and Hospital Care Statistics Branch. National Hospital Ambulatory Medical Care Survey: 2011 Outpatient Department Summary Tables. 2011 [cited 2015 December, 2015]. http://www.cdc.gov/nchs/fastats/drug-use-therapeutic.htm.
World Health Organization. Cancer Pain Relief. Geneva: WHO; 1996.
Naranjo CA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–45.
Moore RA, Derry S, Wiffen PJ, Straube S. Effects of food on pharmacokinetics of immediate release oral formulations of aspirin, dipyrone, paracetamol and NSAIDs—a systematic review. Br J Clin Pharmacol. 2015;80(3):381-8.
Wilkie P. A question of trust: the introduction of a national electronic patient record. Qual Prim Care. 2004;12:95–6.
Wise J. Less than 0.5% of safety incidents reported in 2008–9 came from general practice. Br Med J. 2010;340:c885.
FDA U.S. Department of Health and Human Services. Innovation/Stagnation: Challenge and Opportunity on the Critical Path to New Medical Products. 2004.
FDA U.S. Department of Health and Human Services. Stagnation/Innovation—Critical Path Opportunities List. 2006.
FDA U.S. Food and Drug Administration. Mini-Sentinel. 2014 [cited 2016 June 2016]. http://www.mini-sentinel.org/.
FDA U.S. Food and Drug Administration. Sentinel Program Interim Assessment (FY 15). 2015.
Huang YL, Moon J, Segal JB. A comparison of active adverse event surveillance systems worldwide. Drug Saf. 2014;37(8):581–96.
Porter ME, Teisberg EO. How physicians can change the future of health care. JAMA. 2007;297(10):1103–11.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Tiago Sousa Veloso has nothing to disclose.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/67E4F060201C5DBF.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sousa-Veloso, T. Practice-Based Research Networks: Integrating Clinical Data for Improved Pharmacoepidemiology. Pain Ther 5, 143–148 (2016). https://doi.org/10.1007/s40122-016-0054-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-016-0054-1