Abstract
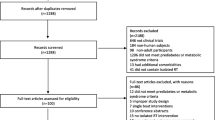
Effectively preventing and treating chronic diseases through health behavior changes often require intensive theory- and evidence-based intervention including long-term maintenance components. We assessed the efficacy of theory-based maintenance approaches varying by dose for persistently performing resistance training (RT) with the hypothesis that a higher-dose social cognitive theory (SCT) approach would produce greater RT adherence than lower-dose Standard. The Resist-Diabetes study first established 2×/week resistance training (RT) in a 3-month supervised intervention in older (50–69 years, N = 170), overweight to obese (BMI 25–39.9 kg/m2) previously inactive adults who fit prediabetes criteria (fasting glucose concentration = 95–125 mg/dl; oral glucose tolerance test 2-h glucose concentration = 140–199 mg/dl or both). After the supervised phase, participants (N = 159) were then randomly assigned to one of two conditions for transition (3 weeks) and then RT alone in community settings for extended contact, maintenance (6 months), and then no contact (6 months). SCT featured continued tailored, interactive personal, and web-based check-ups focused on RT, self-regulation, and a barrier/strategies approach. Standard involved low-dose, generic personal, and web-based check-ups within the same theoretical approach. SCT and Standard both resulted in similar RT, 2×/week adherence during maintenance (74.4 %) and no-contact phases (53.1 %). Cost analysis indicated the Standard intervention for transition and maintenance was inexpensive ($160). Standard can be translated into practice with the potential for continuous contact and persistence in RT beyond the typical program maintenance phase.
Similar content being viewed by others
References
Spring B. Translational behavior medicine: a pathway to better health. Transl Behav Med. 2011; 1: 1-3.
Healthy People 2020. Improving the Lives of Americans. www.healthypeople.gov.
Diabetes Prevention Research Group. 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program outcome study. Lancet. 2009; 374: 1677-1686.
Ford ES, Bergmann MM, Kroger J, et al. Healthy living is the best revenge: findings from the European Prospective Investigation into Cancer and Nutrition-Potsdam study. Arch Intern Med. 2009; 169: 1355-1362.
Pahor M. Consideration of insurance reimbursement for physical activity and exercise programs. JAMA. 2011; 305: 1808-1809.
Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev. 2012; 13: 509-517.
The Look AHEAD Research Group. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010; 170: 1566-1575.
The Look AHEAD Study Group. Cardiovascular effects of intensive lifestyle intervention in Type 2 diabetes. NEJM. 2013; 369: 145-154.
Ritzwoller D, Sukhanova AS, Glasgow RE, et al. Intervention costs and cost effectiveness for a multiple-risk-factor self-management trial for Latinas. Economic analysis of iViva Bien! Transl Behav Med. 2011; 1: 427-435.
Jensen MD, Ryan DH, Apovian CM, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014; 63(25 Pt B): 2985-3023.
Kiernan M, Brown SD, Schoffman DE, et al. Promoting healthy weight with “stability skills first”: a randomized trial. J Consult Clin Psychol. 2013; 81: 336-346.
Jakicic JM, Tate DF, Lang W, et al. Effect of a stepped-care intervention approach on weight loss in adults: a randomized clinical trial. JAMA. 2012; 307: 2617-2626.
Marinik EL, Kelleher S, Savla JT, et al. The Resist Diabetes trial: rationale, design, and methods of a hybrid efficacy/effectiveness intervention trial for resistance training maintenance to improve glucose homeostasis in older prediabetic adults. Control Clin Trials. 2014; 37: 19-42.
ACSM’s Guidelines for Exercise Testing and Prescription. Ninth Edition. Philadelphia. Lippincott, Williams & Wilkins. 2013.
Tabak AG, Herder C, Rathmann U, et al. Prediabetes: a high-risk state for developing diabetes. Lancet. 2012; 379: 2279-2290.
Roberts CK, Little JP, Thyfault JP. Modification of insulin sensitivity and glycemic control by activity and exercise. Med Sci Sports Exerc. 2013; 45: 1868-1877.
Dunstan DW, Daly RM, Owen N, et al. Home-based resistance training is not sufficient to maintain improved glycemic control following supervised training in older individuals with type 2 diabetes. Diabetes Care. 2005; 28: 3-9.
Sigal RJ, Kenny GP, Boule NG, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann of Intern Med. 2007; 147: 357-369.
Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A 1c levels in patients with Type 2 diabetes: a randomized controlled trial. JAMA. 2010; 304: 2253-2262.
Strasser B, Steindorf K, Wiskemann J, et al. Impact of resistance training in cancer survivors: a meta-analysis. Med Sci Sports Exerc. 2013; 45: 2080-2090.
Winett RA, Williams DM, Davy BM. Initiating and maintaining resistance training in older adults: a social cognitive theory-based approach. Br J Sports Med. 2009; 43: 114-119.
Phillips SM, Winett RA. Uncomplicated resistance training and health-related outcomes: evidence for a public health mandate. Curr Sports Med Rep. 2010; 9: 208-213.
Loustalot F, Carlson SA, Kruger J, et al. Muscle-strengthening activities and participation among adults in the United States. Res Q Exerc Sport. 2013; 84: 30-38.
Tanimoto M, Sanada K, Yamamoto K, et al. Effects of whole-body low-intensity resistance training with slow movement and tonic force generation on muscular size and strength in young men. J Strength Cond Res. 2008; 22(6): 1926-1938.
Carpinelli RN. The size principle and a critical analysis of the unsubstantiated heavier-is-better recommendation for resistance training. J Exerc Sci Fit. 2008; 6: 67-85.
Mitchell CJ, Churchward-Venn TA, West DDW, et al. Resistance exercise load does not determine training-mediated hypertrophic gains in young men. J Appl Physio. 2012; 113: 71-77.
Winett RA, Anderson ES, Wojcik JR, et al. Guide to health: a randomized controlled trial of the effects of a completely web-based intervention on physical activity, fruit and vegetable consumption, and body weight. Transl Behav Med. 2011; 1: 165-174.
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004; 31: 143-164.
Eikenberg JD, Savla J, Marinik EL., Pownall J, Baugh ME, Flack KD, Winett RA, Davy BM. Prediabtes phenotype influences improvements in glycemia with resistance training. Paper presented at the annual meeting of The Obesity Society, November, 2013, Atlanta, GA.
Winett RA, Davy BM, Savla JT, et al. Using response variation to develop more effective, personalized behavioral medicine?: evidence from the Resist-Diabetes study. Transl Behav Med. 2014; 4: 333-338.
Resnick B, Inguuito P, Owrig D, et al. Treatment fidelity in behavior change research. Nurs Res. 2005; 54: 139-143.
Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Publ Health Dent. 2011; 71: S52-S63.
Prestwich A, Sniehotta FF, Whittington C, et al. Does theory influence the effectiveness of health behavior interventions? Meta Anal Health Psych. 2014; 33: 465-474.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982; 14: 377-381.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ & Allen J, eds. Measuring alcohol consumption: Psychosocial and biological methods (pp. 41–72). Totowa, NJ: Humana Press.
Ritzwoller DP, Sukhanova A, Gaglio B, et al. Costing behavioral interventions: a practical guide to enhance translation. Ann Behav Med. 2009; 37: 218-227.
Glasgow RE, Fisher L, Strycker LA, et al. Minimal intervention needed to change: definition, use, and value for improving health and health research. Transl Behav Med. 2014; 4: 26-33.
Diabetes Prevention Program Research Group. Costs assessments with the primary prevention of Type 2 diabetes mellitus in the Diabetes Prevention Program. Diabetes Care. 2003; 26: 36-47.
Acknowledgments
This study was funded by National Institute of Diabetes, Digestive, and Kidney Diseases, grant R01 DK082383. We wish to acknowledge the dedication and valuable contributions of John Pownall, RN, MPH, Mary Elizabeth Baugh, MS, RD, Kyle Flack, Ph.D., Nabil Boutagy, Ph.D., Daniel Gochenour, BS, Adrianne Clark, MS, RD, Valisa Hedrick, Ph.D., RD., Chad Blake, BS, Rachel Cornet, MS, RD, Soheir Boshra, MD, Joshua Eikenberg, MPH, and the staff of the area’s health clubs who agreed to work with us on this project.
Disclosure
The contractual arrangements with Sheila G. Winett, MS, have been approved by Virginia Polytechnic Institute and State University.
Adherence to ethical standards
The research protocol was reviewed and approved by the Virginia Tech IRB before research was initiated. Review determined that the proposed activities were in compliance with the University’s Federal-wide Assurance, the Belmont Report principles, 45CFR46, and in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice Implications: Theory and evidence-based, lower-cost maintenance approaches for behavior change should be used within a continual care model for treatment of chronic diseases.
Policy Implications: Health care policies for prevention and treatment of chronic disease through behavior changes need to support theory and evidence-based initial interventions and, critically, also theory and evidence-based, lower-cost maintenance approaches.
Research Implications: A research focus needs to be on lower-cost, theory-based approaches to maintaining health behavior changes for preventing and treating chronic diseases within a continual care model.
About this article
Cite this article
Winett, R.A., Davy, B.M., Savla, J. et al. Theory-based approach for maintaining resistance training in older adults with prediabetes: adherence, barriers, self-regulation strategies, treatment fidelity, costs. Behav. Med. Pract. Policy Res. 5, 149–159 (2015). https://doi.org/10.1007/s13142-015-0304-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-015-0304-5