Abstract
Information on cost-effectiveness of multiple-risk-factor lifestyle interventions for Latinas with diabetes is lacking. The aim of this paper is to evaluate costs and cost-effectiveness for ¡Viva Bien!, a randomized trial targeting Latinas with type 2 diabetes. We estimated 6-month costs; calculated incremental costs per behavioral, biologic, and quality-of-life change; and performed sensitivity analyses from health plan and participant perspectives. Recruitment, intervention, and participant costs were estimated at $45,896, $432,433, and $179,697, respectively. This translates to $4,634 in intervention costs per ¡Viva Bien! participant; $7,723 in both per unit reduction in hemoglobin A1c and per unit reduction in body mass index. Although costs may be higher than interventions that address one risk factor, potential risks for longer-term health-care costs are high for this at-risk group. Given the benefits of ¡Viva Bien!, cost reductions are recommended to enhance its efficiency, adoption, and long-term maintenance without diluting its effectiveness.
Similar content being viewed by others
References
Ritzwoller, D. P., Toobert, D., Sukhanova, A., & Glasgow, R. E. (2006). Economic analysis of the Mediterranean Lifestyle Program for postmenopausal women with diabetes. The Diabetes Educator, 32, 761–769. PMID 16971709.
der Bruggen MA, Jacobs-van, van Baal, P. H., Hoogenveen, R. T., et al. (2009). Cost-effectiveness of lifestyle modification in diabetic patients. Diabetes Care, 32, 1453–1458.
Narayan, K. M. V., D'Agostino, R. B., Kirk, J. K., et al. (2008). Disparities in A1c levels between Hispanic and non-Hispanic white adults with diabetes. Diabetes Care, 31, 240–246.
Emanuele, N., Moritz, T., Klein, R., et al. (2009). Ethnicity, race, and clinically significant macular edema in the Veterans Affairs Diabetes Trial (VADT). Diabetes Research and Clinical Practice, 86, 104–110.
McWilliams, J. M., Meara, E., Zaslavsky, A. M., & Ayanian, J. Z. (2009). Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Annals of Internal Medicine, 150, 505–515.
Lloyd-Jones, D., Adams, R., Carnethon, M., et al. (2009). Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation, 119, 480–486.
Pandey, D. K., Labarthe, D. R., Goff, D. C., Jr., Chan, W., & Nichaman, M. Z. (2001). Community-wide coronary heart disease mortality in Mexican Americans equals or exceeds that in non-Hispanic Whites: the Corpus Christi Heart Project. The American Journal of Medicine, 10, 87.
Hunt, K. J., Williams, K., Resendez, R. G., et al. (2002). All-cause and cardiovascular mortality among diabetic participants in the San Antonio Heart Study: evidence against the "Hispanic Paradox". Diabetes Care, 25, 1557–1563.
Slater, J., Selzer, F., Dorbala, S., et al. (2003). Ethnic differences in the presentation, treatment strategy, and outcomes of percutaneous coronary intervention (a report from the National Heart, Lung, and Blood Institute Dynamic Registry). The American Journal of Cardiology, 92, 773–778.
Flegal, K. M., Carroll, M. D., Ogden, C. L., & Johnson, C. L. (2002). Prevalence and trends in obesity among US adults, 1999–2000. JAMA, 288, 1723–1727.
Maskarinec, G., Grandinetti, A., Matsuura, G., et al. (2009). Diabetes prevalence and body mass index differ by ethnicity: the Multiethnic Cohort. Ethnicity & Disease, 19, 49–55.
Oster, N. V., Welch, V., Schild, L., et al. (2006). Differences in self-management behaviors and use of preventive services among diabetes management enrollees by race and ethnicity. Disease Management, 9, 167–175.
Melloni, C., Berger, J. S., Wang, T. Y., et al. (2010). Representation of women in randomized clinical trials of cardiovascular disease prevention. Circulation: Cardiovascular Quality and Outcomes, 3, 135–142.
Glasgow, R. E., Klesges, L. M., Dzewaltowski, D. A., Bull, S. S., & Estabrooks, P. (2004). The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Annals of Behavioral Medicine, 27, 3–12. PMID 14979358.
The Diabetes Prevention Program Research Group. (2005). Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the Diabetes Prevention Program. Diabetes Care, 28, 888–894.
Knowler, W. C., Fowler, S. E., Hamman, R. F., et al. (2009). 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet, 374, 1677–1686.
The Diabetes Prevention Program Research Group. (2003). Costs associated with the primary prevention of type 2 diabetes mellitus in the Diabetes Prevention Program. Diabetes Care, 26, 36–47.
Toobert, D. J., Glasgow, R., Strycker, L. A., et al. (2003). Biologic and quality of life outcomes from the Mediterranean Lifestyle Program: a randomized clinical trial. Diabetes Care, 26, 2288–2293.
Toobert, D. J., Glasgow, R. E., & Radcliffe, J. L. (2000). Physiologic and quality of life outcomes from the Women's Lifestyle Heart Trial. Annals of Behavioral Medicine, 22, 1–9.
Toobert, D. J., Glasgow, R. E., Nettekoven, L., & Brown, J. E. (1997). Behavioral and psychosocial effects of intensive lifestyle management for women with coronary heart disease. Patient Education and Counseling, 35, 177–188.
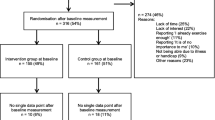
Toobert, D. J., Strycker, L. A., Glasgow, R. E., et al. (2010). Viva bien!: overcoming recruitment challenges in a multiple-risk-factor diabetes trial. American Journal of Health Behavior, 34, 432–441.
Osuna, D., Barrera, M. Jr., Strycker, L.A., et al. (2009). Methods for the cultural adaptation of a diabetes lifestyle intervention for latinas: an illustrative project. Health Promotion Practice [Epub ahead of print]
Ritzwoller, D. P., Sukhanova, A., Gaglio, B., & Glasgow, R. E. (2009). Costing behavioral interventions: a practical guide to enhance translation. Annals of Behavioral Medicine, 37, 218–227.
Sukhanova, A., Ritzwoller, D. P., Alexander, G., et al. (2009). Cost analyses of a web-based behavioral intervention to enhance fruit and vegetable consumption. International Journal of Behavioral Nutrition and Physical Activity, 6, 92.
United States Department of Labor. Bureau of Labor Statistics (BLS). Retrieved October 7, 2010, from http://www.bls.gov.
Renaud, S., de Lorgeril, M., Delaye, J., et al. (1995). Cretan Mediterranean diet for prevention of coronary heart disease. The American Journal of Clinical Nutrition, 61, 1360S–1367S.
Sharma, A., Jofre-Bonet, M., Panca, M., Lawrenson, J. G., & Murdoch, I. (2010). Hospital-based glaucoma clinics: what are the costs to patients? Eye (London, England), 24, 999–1005.
Nguyen, H. Q., Maciejewski, M. L., Gao, S., et al. (2008). Health care use and costs associated with use of a health club membership benefit in older adults with diabetes. Diabetes Care, 31, 1562–1567.
Ball, S., & Golhofner, A. (2008). Comparison of a commercial weight loss program to a fitness center. Journal of Exercise Physiology, 11, 1–12. Retrieved February 23, 2011, from http://faculty.css.edu/tboone2/asep/BallJEPonlineJune2008.pdf.
Center for Medical Technology Policy. Patient-Centered Outcomes Research Institute. Retrieved October 7, 2010, from http://www.cmtpnet.org/comparative-effectiveness/overview-of-the-patient-centered-outcomes-research-institute.
Institute of Medicine, Committee on Quality Health Care in America. (2003). Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press.
Glasgow, R. E., Strycker, L. A., Kurz, D., et al. (2010). Recruitment for an internet-based diabetes self-management program: scientific and ethical implications. Annals of Behavioral Medicine, 40, 40–48.
Finkelstein, E. A., Troped, P. J., Will, J. C., & Palombo, R. (2002). Cost-effectiveness of a cardiovascular disease risk reduction program aimed at financially vulnerable women: the Massachusetts WISEWOMAN project. Journal of Women’s Health and Gender-Based Medicine, 11, 519–526.
Bennett, G. G., & Glasgow, R. E. (2009). The delivery of public health interventions via the Internet: actualizing their potential. Annual Review of Public Health, 30, 273–292.
Mechael, P., Batavia, H., Kaonga, N., et al. (2010). Barriers and gaps affecting mHealth in low and middle income countries: policy white paper datasheet. Report/White Paper. The Earth Institute Columbia University, mHealth Alliance.
Kennedy, A., Reeves, D., Bower, P., et al. (2007). The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomised controlled trial. Journal of Epidemiology and Community Health, 61, 254–261.
Ayala, G. X., Vaz, L., Earp, J. A., Elder, J. P., & Cherrington, A. (2010). Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Education Research, 25, 815–840.
Sterman, J. (2006). Learning from evidence in a complex world. American Journal of Public Health, 96, 505–514.
National Cancer Institute. Cancer Intervention and Surveillance Modeling Network. Retrieved October 7, 2010, from http://cisnet.cancer.gov.
Meenan, R. T., Stevens, V. J., Hornbrook, M. C., et al. (1998). Cost-effectiveness of a hospital-based smoking cessation intervention. Medical Care, 36, 670–678.
Tunis, S. R., Stryer, D. B., & Clancey, C. M. (2003). Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA, 290, 1624–1632. PMID 14506122.
Glasgow, R. E., Magid, D. J., Beck, A., Ritzwoller, D., & Estabrooks, P. A. (2005). Practical clinical trials for translating research to practice: design and measurement recommendations. Medical Care, 43, 551–557. PMID 15908849.
Medical Research Council. Leading science for better health. Retrieved February 23, 2011, from http://www.mrc.ac.uk/index.htm.
Kessler, R., & Glasgow, R.E. (2010) A proposal to speed translation of healthcare intervention research into practice: dramatic change is needed. American Journal of Preventive Medicine (in press).
Wing, R. R., & Hill, J. O. (2001). Successful weight loss maintenance. Annual Review of Nutrition, 21, 323–341.
Ornish, D., Brown, S. E., Scherwitz, L. W., et al. (1990). Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet, 336, 129–133.
Acknowledgments
Funding for this project was provided by the National Heart, Lung, and Blood Institute, grant #HL076151-01.
Dr. Glasgow is now Deputy Director for Dissemination and Implementation Science, Division of Cancer Control and Population Sciences, National Cancer Institute. The opinions in this article do not necessarily represent those of the National Cancer Institute or any other body.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: While resource intensive interventions may be needed to produce lasting changes in complex multiple lifestyle behaviors, healthcare organizations should explore the use of a variety of technologies that could enhance efficiency and adoption these interventions.
Policy: The transparent reporting of recruitment and interventions costs are crucial requirements for the dissemination and implementation of successful behavioral interventions into non-academic settings.
Research: Future economic analyses associated with behavioral interventions should be directed towards understanding the resources needed to implement an intervention, in a variety of settings, given the expected outcome.
About this article
Cite this article
Ritzwoller, D.P., Sukhanova, A.S., Glasgow, R.E. et al. Intervention costs and cost-effectiveness for a multiple-risk-factor diabetes self-management trial for Latinas: economic analysis of ¡Viva Bien!. Behav. Med. Pract. Policy Res. 1, 427–435 (2011). https://doi.org/10.1007/s13142-011-0037-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-011-0037-z