Abstract
Background
Joint salvage surgery for patients with juxtaarticular osteosarcoma remains challenging, especially when the tumor invades the epiphysis. Because patients are surviving longer with current chemotherapy regimens, it is advantageous to retain native joints if possible, especially in young patients. However, the results using joint-preserving tumor resections in this context have not been well characterized.
Questions/purposes
(1) What are the functional outcomes after limb salvage surgery at a minimum of 3 years? (2) What are the oncologic outcomes? (3) Is joint salvage surgery for epiphyseal tumors associated with an increased risk of local recurrence compared with metaphyseal tumors not invading the epiphysis? (4) What are the complications associated with joint salvage surgery?
Methods
Between 2004 and 2013, we treated 117 patients with juxtaarticular osteosarcoma; of those, 43 (38%) were treated with joint salvage surgery, and 41 (95%) of the 43 patients are included in our study. The other two (5%) were lost to followup before 3 years (mean, 4.4 years; range, 3–11 years,). During the period in question, we generally performed joint salvage surgery in these patients when they had a favorable response to chemotherapy, did not have a pathologic fracture or extrusion of the tumor into the joint, and did not have a whole-epiphyseal osteolytic lesion, a large mass, or obvious neurovascular involvement. This report is a followup of an earlier study; the current study includes an additional nine patients, and additional followup of a mean of 19 months for the patients included in the earlier report. We ascertained overall survival and survival free from local recurrence which was estimated using the Kaplan-Meier method, functional status of the limb which was evaluated using the Musculoskeletal Tumor Society (MSTS)-93 scoring system, and recorded reconstructive complications including infection, fracture, skin necrosis, and nonunion. We compared oncologic and functional outcomes between patients with (n = 28) and without tumor extension to epiphysis (n =13). We also compared oncologic and functional outcomes among patients with different adjuvant treatments including microwave ablation (n = 11), cryoablation (n = 12), and navigation-assisted osteotomy (n = 5). Complications were tallied using records from our institutional database.
Results
The overall Kaplan-Mayer survival rate was 82% (95% CI, 104–128 months) at 5 years. The overall Kaplan-Meier survivorship from local recurrence was 91% at 5 years (95% CI, 115–133 months). Three patients had a local recurrence, but none had local recurrence in or close to the remaining epiphysis. The MSTS scores ranged from 22 to 30 points, with a median of 28. There were no differences in survival rate, local recurrence, or MSTS scores between patients with a tumor that did not invade the epiphysis and those in whom the tumor did invade the epiphysis. There were differences in MSTS scores among patients with epiphyseal tumor extension in which different adjuvant techniques, including microwave ablation, cryoablation, and navigation-assisted osteotomy, were used. Additional surgical procedures were recorded for 10 patients (24%). Osteonecrosis of the residual epiphysis was detected 13 patients (31%).
Conclusions
Our findings suggest it is possible to salvage joints in selected patients with juxtaarticular osteosarcoma around the knee. The patients who have a favorable response to chemotherapy are the best candidates for this approach. Future studies might explore the role of adjuvant techniques of microwave ablation and cryoablation, particularly when the tumor invades the epiphysis, and whether resections can be facilitated with navigation.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Introduction
Osteosarcoma often appears in the metaphyseal region of long bones, with approximately 60% of the cases occurring around the knee [17, 18, 29, 33]. Previous studies have shown that the prevalence of transepiphyseal spread of the tumor in metaphyseal osteosarcomas is approximately 80% [37, 39]. Despite controversies, some authors believe that the end of the joint should be resected along with the tumor when the tumor invades the epiphysis for the safety of local tumor control [29, 32, 45]. Amputation or complete excision of the tumor along with the joint followed by endoprosthetic reconstruction offers the best chance for local control, but endoprostheses present subsequent reconstructive complications. The reported survival rates of endoprostheses range from 50% to 70% [7, 20, 34, 37, 41]. In addition, epiphyseal resection in growing children presents the unique challenge of maintaining equal limb length throughout the child’s growth. Although expandable endoprostheses have been developed to address limb length discrepancy, approximately 25% to 80% of expandable endoprostheses are revised during the first 5 years, and the overall risk of at least one complication developing is as much as 82% at 10 years [9, 12, 36, 38, 40].
Zimel et al. [45] reported joint-sparing intercalary resection combined with appropriate biologic reconstruction had better durability compared with endoprosthetic reconstruction. In addition, there have been attempts to improve contiguous joint function by means of intercalary resection after physeal distraction [5, 6], transepiphyseal resection [13, 30, 32], or multiplanar osteotomy [4], preserving the entire or part of the articular surface. We have tried multiple adjuvant techniques including navigation [25, 27], microwave ablation [23], and argon-based ablation [24] to aid joint-sparing tumor resection, with the goal of exploring a surgical strategy to maximize the chance of joint preservation with full consideration of a safe resection margin, important structures such as the ACL and PCL, articular cartilage, and subchondral bone reservation, and preservation of the joint. We previously reported the preliminary outcomes of these joint salvage procedures [23–27]; the current evaluation provides a larger patient group and a longer followup period. In this study, we sought to ascertain whether our surgical strategy allows native joint salvage with acceptable limb function without compromising the oncologic outcomes. To address this issue, we asked the following questions: (1) What are the functional outcomes after limb salvage surgery at a minimum of 3 years? (2) What are the oncologic outcomes? (3) Is joint salvage surgery for epiphyseal tumors associated with an increased risk of local recurrence compared with metaphyseal tumors not invading the epiphysis? (4) What are the complications associated with joint salvage surgery?
Patients and Methods
Between January 2004 and May 2013, 117 patients with high-grade osteosarcomas of the knee were treated at our institution. Of those, 15 patients who had Stage III tumors, 11 with pathologic fractures, seven with tumor breach into the joint, 12 with whole-epiphyseal osteolytic lesions, 11 with large masses and/or obvious neurovascular involvement, and 18 with an unfavorable response to chemotherapy were excluded, leaving 43 patients in the current study. Of those, two (5%) were lost to followup before a minimum of 3 years (mean, 4.4 years; range, 3-11 years). Favorable chemotherapeutic response consisted of at least one of the following: good margination of the tumor or shrinkage of the tumor observed on MRI; the decrease of abnormal radionuclide uptake on bone scan; or pain or mass reduction on clinical physical examination. Eighteen patients were excluded purely on the basis of having an unfavorable response. We offered the 43 patients the option of an epiphyseal-sparing procedure. Approval for the study was obtained from the institutional review board.
Twenty male patients and 21 female patients were included in this study. Their mean age was 13 years (range, 8–24 years). Thirty-nine patients were diagnosed with Musculoskeletal Tumor Society (MSTS) Stage IIB osteosarcoma and two with Stage IIA osteosarcoma after an imaging workup followed by biopsy. The tumors were located in the femur in 14 patients and the tibia in 27 patients. All patients received neoadjuvant chemotherapy. The current study is a followup of earlier studies [23–27] and includes an additional nine patients and additional followup of a mean of 19 months for the patients included in the earlier studies.
Surgical Strategy
Reconstructive options after epiphyseal preserved intercalary resection included allograft or frozen tumor-bearing bone in combination with or without a vascularized fibula flap for all but five patients. An osteoarticular allograft with a half-condyle or plateau in combination with a vascularized fibula flap was used for reconstruction for these five patients.
Oncologic Evaluation
All patients were followed up at 1 month, 3 months, every 3 months for 2 years, every 6 months until 3 years, and annually thereafter. Local recurrence was screened according to symptomatology, plain radiographs, or bone scans. Metastasis was determined by routine plain chest radiography, CT, and bone scan.
Radiographic Analysis and Functional Evaluation
Radiographs were evaluated for bone healing and joint degeneration. The radiographic evaluation of degenerative severity was performed using the Kellgren-Lawrence classification, which includes four grades [21]. In our study, the Kellgren-Lawrence classification was summarized into three groups: no degeneration, mild degeneration (Grades 1 and 2), and severe degeneration (Grades 3 and 4). SPECT-CT was used to assess osteonecrosis of the residual epiphysis at 3 months. The MSTS score [10] was used to assess functional outcome. Active ROM of the knee was measured and recorded as the percentage of the contralateral side. All patients were followed up by the chief surgeon (JL). Reconstructive complications include infection, fracture, skin necrosis, and nonunion. Complications were tallied from the records in our institutional database.
Cotreatments
If the tumor is located within 1 to 2 cm of the growth plate, intraoperative navigation is used to identify the tumor edge and to optimize the likelihood that a limited wide margin would be achieved while saving the growth plate. If the osteoblastic tumor is located within 0 to 10 mm from the growth plate, physeal separation by external fixator distraction is used. After that, a diaphyseal osteotomy can be performed and the tumor can be removed en bloc with a limited wide margin.
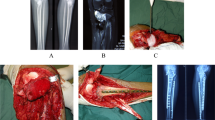
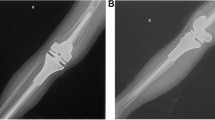
If the tumors invade the epiphysis, a different adjuvant technique is used. When the tumor is more than 1 cm from the articular cartilage and cruciate ligaments, microwave ablation is used to ablate the tumor edge, and a transepiphyseal osteotomy is performed through the edge of the tumor to preserve more than 1 cm thickness of the epiphysis [23]. The resection margin is necrotic and the residual epiphysis is viable. If the distance between the tumor edge and cruciate ligament is less than 10 mm, three cycles of in situ argon-based cryoablation is used to sterilize the epiphyseal tumor. Then a transepiphyseal osteotomy is made to preserve the necrotic epiphysis (Fig. 1). If the osteolytic tumor occupying less than half of the plateau or condyle is at least 1 cm from the cruciate ligaments, an irregular osteotomy under navigation guidance allows half of the epiphysis and its attached cruciate ligament to be saved (Fig. 2).
A 10-year-old boy had an osteosarcoma of the distal femur. He underwent transepiphyseal resection of an epiphyseal osteosarcoma after adjuvant cryoablation. (A) The radiograph shows an osteosarcoma in the patient’s distal femur. (B) His MR image shows the tumor invading the medial condyle of the femur. Intraoperative photographs show (C) cryoablation of the medial condyle, and (D) the epiphysis as preserved after transepiphyseal osteotomy. (E) An AP radiograph shows reconstruction by liquid nitrogen devitalized tumor-bearing autograft in combination with vascularized fibula flap. (F) The SPECT-CT shows osteonecrosis of the medial condyle and normal viability of the lateral condyle (right side of the knee). (G) An AP radiograph obtained 4 years postoperatively shows normal joint space of the knee. This patient has a Musculoskeletal Tumor Society score of 29.
A 14-year-old boy had a high-grade osteosarcoma of the proximal tibia. He underwent irregular osteotomy with aid of intraoperative navigation and half of his medial plateau was preserved. (A) This radiograph shows the tumor located at the lateral portion of the proximal tibia. (B) The MR image shows the tumor invading the lateral plateau. (C) The medial plateau and its attached cruciate ligament, meniscus, and medial cruciate ligament were preserved after navigation-assisted irregular tumor resection. (D) The defect was reconstructed with an ipsilateral pedicled fibula flap and osteoarticular allograft and the fibular defect after graft harvesting was repaired with another allograft. Normal knee space was maintained at 5 years followup. The patient’s Musculoskeletal Tumor Society score is 30.
Statistics Analysis
Overall survival rates were estimated using the Kaplan-Meier method. One-way ANOVA with Bonferroni post hoc comparison was performed unless otherwise indicated. The Kruskal-Wallis test was used to determine differences between groups for nonnormally distributed continuous data. Post hoc comparisons for the nonnormally distributed continuous data were performed using the Mann-Whitney test. The Pearson chi-square test was used to compare the frequency distribution of categorical variables between groups. Post hoc comparisons for categorical data were performed using the Pearson chi-square test. All analyses were two-sided, and the α level was set to 0.05. All calculations were performed using SPSS Version 17.0 statistical software (SPSS Inc, Chicago, IL, USA).
To determine whether tumor invading the epiphysis has an influence on overall oncologic and functional outcomes, we compared the survival rate, local recurrence, MSTS score, and ROM of the knee between patients who had a tumor without epiphyseal involvement (n = 13) and those with a tumor with epiphyseal extension (n = 28). We also compared MSTS scores, severity of the degenerative alteration, and ROM of the knee among patients who had epiphyseal tumor extension with cotreatment of microablation (n = 11), cryoablation (n = 12), and navigation-assisted irregular osteotomy (n = 5).
Results
Functional Outcome
The overall MSTS scores for our study patients ranged from 22 to 30, with a median of 28. With the numbers of patients we had, we found no difference in the MSTS scores between patients with and without epiphyseal extension (p = 0.384) (Table 1). Patients without epiphyseal extension had greater ROM of the knee compared with patients with epiphyseal extension (p < 0.001) (Table 2). Among groups with epiphyseal extension, patients with cotreatment with cryoablation had lower MSTS scores compared with those with microwave ablation and with navigation-aided resection (p = 0.001; p = 0.001); with the numbers we had we could observe no difference in MSTS scores between patients with cotreatment with microwave ablation and with navigation-aided resection (p = 0.094) (Table 3). With respect to ROM of the knee, in the group with epiphyseal extension, patients with cotreatment with microwave ablation and cryoablation had greater ROM compared with patients with navigation-aided resection (p < 0.001; p < 0.001, respectively); by contrast, with the numbers we had, there was no difference in ROM between patients with cotreatment with microwave ablation and cryoablation (p = 1.000) (Table 4).
Oncologic Outcome
The overall Kaplan-Meier survival for our study population was 82% at 5 years (95% CI, 104–128 months). The survival rate of the reconstructed limb was 93%. At the final followup, 31 patients continued to be disease-free, one was alive with disease, three had no evidence of disease, and six had died of disease with the cause of death being lung metastasis in all. Mean time of death was 30 months after diagnosis.
Local Recurrence
The overall Kaplan-Meier survivorship from local recurrence was 91% at 5 years (95% CI, 115–133 months). Three patients had local recurrence. These local recurrences were seen at 18, 27, and 34 months after surgery, respectively. The recurrences were located in soft tissue and were away from the joint-side osteotomy line (7 cm, 10 cm, and 11 cm). Two of the relapsed tumors encased the femoral vessel or posterior tibial vessel and one was around the posterior tibial nerve. One patient with concurrent pulmonary metastasis died of the disease 38 months after surgery. In the two patients who underwent amputation, one died of lung metastasis 15 months after amputation and the other patient had no evidence of disease at the final followup 43 months after relapse. With the numbers available, we found no differences between patients with tumors of the metaphysis and those with tumors involving the epiphysis in terms of local recurrence (p = 0.950) and survival rate (p = 0.924) (Table 5).
Complications
There were five complications, consisting of one allograft nonunion (in a patient without epiphyseal extension), skin necrosis (one patient with epiphyseal extension and one patient without epiphyseal extension), and two deep infections (one patient with epiphyseal extension and one without epiphyseal extension). Nonunion of the host allograft junction was found in one patient. Eventually the allograft was removed and the defect was reconstructed with vascularized fibula graft in combination with another allograft. The two patients with skin necrosis were treated with débridement and rotational full-thickness skin and subcutaneous flap transplantation. One infection in a 12-year-old boy persisted for 18 months until the hardware was removed. The other infection was in an 8-year-old boy. He had a deep infection 15 months postoperatively. Because the infection could not be controlled, he underwent mid-thigh amputation. Osteonecrosis of the remaining epiphysis was seen in all 12 patients with cotreatment of cryoablation and one patient with cotreatment of microwave ablation. Kellgren-Lawrence scores from 1 to 4 were more prevalent in patients with cotreatment with cryoablation and navigation-assisted osteotomy than in those with microwave ablation (p = 0.005) (Table 6). By the end of followup, three patients did not reach skeletal maturity (closed physis). Limb-length discrepancy ranging from 1 to 3.5 cm was observed in 12 patients and no patient underwent surgical treatment for this discrepancy. Additional surgical procedures, such as bone grafting or amputation, were recorded for 10 patients (24%).
Discussion
Despite functionally appealing in maintaining the native knee, the transepiphyseal intercalary resection may be associated with a higher risk of tumor relapse. Some authors believe one basic criterion for epiphyseal-sparing tumor resection is that the distance between the articular joint cartilage and the tumor as assessed by MRI should be 2 cm or more, to obtain a bone width margin at least of 1 cm [3, 32, 45]. We previously reported that cotreatments of cryoablation, microwave ablation, and navigation-assisted osteotomy could make entire or partial epiphyseal-sparing resection possible even when a tumor invades the epiphysis [23–27]. However, whether joint-sparing resection for patients with an epiphyseal tumor compromises the oncologic outcomes is unknown. To our knowledge, this issue has not been addressed in any publication. Our study showed no difference between patients with a tumor in the metaphysis and those with a tumor in the epiphysis with respect to local relapse, distant metastasis, and overall survival. A limb survival rate of 93% for our study patients is similar to rates reported with other techniques [15, 19, 22].
We acknowledge limitations of this retrospective study. First, the number of patients is small as with many orthopaedic oncology studies. There was no control group, and it remains to be seen whether epiphyseal-sparing intercalary resection achieves safe local control and better functional results compared with those of wide resection of the entire end of the joint. However, to our knowledge, there is no published study that specifically looked at the role of different cotreatments in joint salvage surgery; we report its functional and oncologic outcomes and compare these data with previously reported data regarding joint-sacrificing resection. Second, we did not evaluate necrosis rate and there was no direct histologic evidence supporting complete devitalization of the tumor after adjuvant cryoablation or microwave ablation, especially in a preserved epiphysis. However, the absence of any local recurrence in or close to the preserved epiphysis during the minimum 3-year followup indicates that the surgical margin close to the transepiphyseal resection site was adequate even after intralesional resection after cotreatment of cryoablation or microwave ablation. Third, the indications for different cotreatments are based on clinical experience and are somewhat arbitrary; however, the native joint was preserved with these cotreatments, otherwise it would have been sacrificed along with the tumor. This may be an advantage and shows the evolution in the joint salvage surgery. Fourth, the followup is short and not all patients reached the end of growth. This study however, focuses on preservation of the native joint rather than saving the growth plate. We suspect limb discrepancy or joint deformation is inevitable if an open physis is ablated along with the tumor.
With the numbers we had, we could not show a difference in MSTS scores between patients with a tumor that did not invade the epiphysis and those in whom the tumor did invade the epiphysis. However, we did find a difference in ROM of the knee in patients with an epiphyseal tumor compared with those who only had a metaphyseal tumor. It could be assumed that resections close to a joint could result in scarring and loss of motion. The average MSTS score of 91% of this series was comparable or better than scores in previous reports of prosthetic reconstruction after resections of the entire end of the joint [7, 20, 34, 41].
The overall 5-year survival rate of patients in this study was 82%, which was comparable to or better than rates in other studies [1, 45]. This is likely because patients in our series have favorable characteristics such as a good response to chemotherapy and lack of a massive soft tissue mass. Based on this, we believe joint salvage surgery did not appear to increase adverse oncologic outcomes in this selected patient population.
In previous studies of the epiphyseal-sparing procedure, in which a wide surgical margin was achieved, the local recurrence rates ranged from 7.7% to 18% [3, 32, 45]. Three of our patients (7%) experienced local recurrence, which was comparable to a mean local recurrence of 6.9% (range, 0%–18%) reported in series of limb salvage procedures [13, 19, 22, 30, 45]. The three recurrences were located away from the joint-end osteotomy site; two of the relapsed tumors encased a major vessel (femoral vessels and posterior tibia vessels), and one is near the posterior tibial nerve. This leads us to suspect that the local recurrences in our patients were attributable to an inadequate resection margin around the major neurovascular bundle rather than from a transepiphyseal intraosseous margin, but there is no way to be sure of that and that the closer bony margins did not contribute to the local recurrences in some way. Therefore, we caution others to be vigilant in selecting patients for these types of resections. Although intercalary resection through the epiphysiometaphyseal area has been attempted, there is no consensus regarding what constitutes a safe margin for local tumor control [2]. In our study, limited wide and necrotic margins at the transepiphyseal osteotomy were identified and no patient had local recurrence in or close to the preserved epiphysis. Meanwhile, with the numbers available, we did not find a difference in local recurrence between patients with tumors of the metaphysis and those involving the epiphysis. Aponte-Tinao et al. [3] reported that a minimum negative margin of 10 mm in bone did not lead to tumor relapse in the remaining epiphysis. Hayashi et al. [14] suggested a marginal margin associated with caffeine-potentiated chemotherapy did not give rise to an increased risk of local recurrence. With more accuracy of MRI in delineating tumors [16], closer margins are being used allowing more joint- or physeal-sparing tumor resections [8]. CT or MRI-based navigation enables the surgeon to identify the tumor edge and perform a precise osteotomy with narrower healthy bone surrounding the tumor, maximizing the tissue preservation [26, 44]. Technically, a “limited wide” margin was achieved when we used navigation-assisted osteotomy. For patients with a tumor invading less than half of the epiphysis, a precise irregular osteotomy, with the aid of navigation, makes half-joint structure preservation possible; otherwise, it would be resected along with the tumor. When the tumor transgresses the physes with no hope of growth-plate preservation, the surgical goal should be retaining as much epiphysis as possible. Microwave and argon-based ablations are tools that have been widely used for primary and metastatic malignancy [11, 31, 43]. Both methods could devitalize a tumor in situ through an antenna. When compared with cryoablation that provides an extensive obscure ablation area [35], microwave ablation tends to produce a more-limited ablation zone as small as 1 cm in diameter [28]. Therefore, if the distance between the tumor and the articular cartilage is more than 1 cm, we prefer using microwave to ablate the tumor edge. After that, the designed osteotomy goes through the necrotic area, which not only appears to provide a safe margin, but preserves as much viable epiphysis as possible. This might explain the majority of the residual epiphyses that were viable after microwave ablation.
We noted several complications in our patients that also have been reported by others. There is a paucity of research regarding the approach of retaining the native joint when a tumor is very close to the joint surface. In an attempt to preserve the intact knee in this tough situation, Tsuchiya et al. [42] described a technique, which includes making a one-end osteotomy and rotating the tumor-bearing bone along with its attached end of the joint in liquid nitrogen to sterilize tumor-bearing bone. Different from a pedicle technique, we used argon-based cryoablation producing a necrotic epiphysis before transepiphyseal resection. It enabled us to not only sterilize the tumor in the epiphysis without side effects like devitalization of the other end of the joint, but also to keep the knee intact. Despite its merit, osteonecrosis occurred at variable degrees in all residual epiphyses after cryosurgery. Fortunately, the patients had reasonable clinical outcomes. It suggests that osteonecrosis may be better tolerated by the young population. Degenerative changes are more evident in patients who underwent cryoablation and half condyle-plateau resection procedures as opposed to those with microwave ablation. We surmised that osteonecrosis and subsequent microcollapse and joint instability may cause joint degeneration. Despite that degenerative alteration is asymptomatic and did not jeopardize functional outcomes at recent followup, we suspect it may become severe in some patients, and revision surgery is inevitable at long-term followup. The infection rate of 5% was comparable or better than reported rates of 6% and 22% [3, 45]. The nonunion rate of 2% was lower than a previously reported rate of 9% [3]; we surmise that use of vascularized fibula for reconstruction decreased the risk of the nonunion.
This joint-preserving surgical strategy might allow retention of the epiphysis and limits the reconstruction to the intercalary segment. Although we did not have a comparison group, this approach seems to offer a risk of local recurrence and complication rate comparable to rates reported for other types of resection [7, 20, 29, 34, 41], and we found comparable functional results [3, 17, 32]. We believe the potential advantage of this approach is that it saves native articular surfaces and joints, which may increase the longevity of these reconstructions. Future studies might explore the role of adjuvant techniques of microwave ablation and cryoablation, particularly when a tumor invades the epiphysis, and whether resections can be facilitated with navigation.
References
Ando K, Heymann MF, Stresing V, Mori K, Rédini F, Heymann D. Current therapeutic strategies and novel approaches in osteosarcoma. Cancers (Basel). 2013;5:591–616.
Andreou D, Bielack SS, Carrle D, Kevric M, Kotz R, Winkelmann W, Jundt G, Werner M, Fehlberg S, Kager L, Kühne T, Lang S, Dominkus M, Exner GU, Hardes J, Hillmann A, Ewerbeck V, Heise U, Reichardt P, Tunn PU. The influence of tumor- and treatment-related factors on the development of local recurrence in osteosarcoma after adequate surgery: an analysis of 1355 patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. Ann Oncol. 2011;22:1228–1235.
Aponte-Tinao L, Ayerza MA, Muscolo DL, Farfalli GL. Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res. 2015;473:1789–1796.
Avedian RS, Haydon RC, Peabody TD. Multiplanar osteotomy with limited wide margins: a tissue preserving surgical technique for high-grade bone sarcomas. Clin Orthop Relat Res. 2010;468:2754–2764.
Betz M, Dumont CE, Fuchs B, Exner GU. Physeal distraction for joint preservation in malignant metaphyseal bone tumors in children. Clin Orthop Relat Res. 2012;470:1749–1754.
Cañadell J, Forriol F, Cara JA. Removal of metaphyseal bone tumours with preservation of the epiphysis: physeal distraction before excision. J Bone Joint Surg Br. 1994;76:127–132.
Capanna R, Scoccianti G, Frenos F, Vilardi A, Beltrami G, Campanacci DA. What was the survival of megaprostheses in lower limb reconstructions after tumor resections? Clin Orthop Relat Res. 2015;473:820–830.
Cho HS, Oh JH, Han I, Kim HS. Joint-preserving limb salvage surgery under navigation guidance. J Surg Oncol. 2009;100:227–232.
Cipriano CA, Gruzinova IS, Frank RM, Gitelis S, Virkus WW. Frequent complications and severe bone loss associated with the epiphysis expandable distal femoral prosthesis. Clin Orthop Relat Res. 2015;473:831–838.
Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246.
Fan QY, Ma BA, Zhou Y, Zhang MH, Hao XB. Bone tumors of the extremities or pelvis treated by microwave-induced hyperthermia. Clin Orthop Relat Res. 2003;406:165–175.
Gupta A, Meswania J, Pollock R, Cannon SR, Briggs TW, Taylor S, Blunn G. Non-invasive distal femoral expandable endoprosthesis for limb-salvage surgery in paediatric tumours. J Bone Joint Surg Br. 2006;88:649–654.
Hamed Kassem Abdelaal A, Yamamoto N, Hayashi K, Takeuchi A, Miwa S, Tsuchiya H. Epiphyseal sparing and reconstruction by frozen bone autograft after malignant bone tumor resection in children. Sarcoma. 2015;2015:892141.
Hayashi K, Tsuchiya H, Yamamoto N, Takeuchi A, Tomita K. Functional outcome in patients with osteosarcoma around the knee joint treated by minimised surgery. Int Orthop. 2008;32:63–68.
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, Hornicek FJ, Temple HT, Ruggieri P, Letson GD. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93:418–429.
Hoffer FA, Nikanorov AY, Reddick WE, Bodner SM, Xiong X, Jones-Wallace D, Gronemeyer SA, Rao BN, Kauffman WM, Laor T. Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol. 2000;30:289–298.
Jaffe N, Puri A, Gelderblom H. Osteosarcoma: evolution of treatment paradigms. Sarcoma. 2013;2013:203531.
Jeys L, Grimer R. The long-term risks of infection and amputation with limb salvage surgery using endoprostheses. Recent Results Cancer Res. 2009;179:75–84.
Jeys LM, Kulkarni A, Grimer RJ, Carter SR, Tillman RM, Abudu A. Endoprosthetic reconstruction for the treatment of musculoskeletal tumors of the appendicular skeleton and pelvis. J Bone Joint Surg Am. 2008;90:1265–1271.
Kawai A, Lin PP, Boland PJ, Athanasian EA, Healey JH. Relationship between magnitude of resection, complication, and prosthetic survival after prosthetic knee reconstructions for distal femoral tumors. J Surg Oncol. 1999;70:109–115.
Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Kumta SM, Chow TC, Griffith J, Li CK, Kew J, Leung PC. Classifying the location of osteosarcoma with reference to the epiphyseal plate helps determine the optimal skeletal resection in limb salvage procedure. Arch Orthop Trauma Surg. 1999;119:327–331.
Li J, Guo Z, Wang Z, Fan H, Fu J. Does microwave ablation of the tumor edge allow for joint-sparing surgery in patients with osteosarcoma of the proximal tibia? Clin Orthop Relat Res. 2015;473:3204–3211.
Li J, Guo Z, Yang Q, Ji C, Wang Z. Adjuvant argon-based cryoablation for joint-preserving tumor resection in patients with juxta-articular osteosarcoma around the knee. Cryobiology. 2015;71:236–243.
Li J, Shi L, Chen GJ. Image navigation assisted joint-saving surgery for treatment of bone sarcoma around knee in skeletally immature patients. Surg Oncol. 2014;23:132–139.
Li J, Wang Z, Guo Z, Chen GJ, Yang M, Pei GX. Irregular osteotomy in limb salvage for juxta-articular osteosarcoma under computer-assisted navigation. J Surg Oncol. 2012;106:411–416.
Li J, Wang Z, Guo Z, Chen GJ, Yang M, Pei GX. Precise resection and biological reconstruction under navigation guidance for young patients with juxta-articular bone sarcoma in lower extremity: preliminary report. J Pediatr Orthop. 2014;34:101–108.
Lubner MG, Brace CL, Hinshaw JL, Lee FT Jr. Microwave tumor ablation: mechanism of action, clinical results, and devices. J Vasc Interv Radiol. 2010;21(8 suppl):S192–203.
Malawer MM, Chou LB. Prosthetic survival and clinical results with use of large segmental replacements in the treatment of high grade bone sarcoma. J Bone Joint Surg Am. 1995;77:1154–1165.
Manfrini M, Gasbarrini A, Malaguti C, Ceruso M, Innocenti M, Bini S, Capanna R, Campanacci M. Intraepiphyseal resection of the proximal tibia and its impact on lower limb growth. Clin Orthop Relat Res. 1999;358:111–119.
Meller I, Weinbroum A, Bickels J, Dadia S, Nirkin A, Merimsky O, Issakov J, Flusser G, Marouani N, Cohen N, Kollender Y. Fifteen years of bone tumor cryosurgery: a single-center experience of 440 procedures and long-term follow-up. Eur J Surg Oncol. 2008;34:921–927
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am. 2005;87(suppl 1):226–236.
Ottaviani G, Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13.
Racano A, Pazionis T, Farrokhyar F, Deheshi B, Ghert M. High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: a systematic review. Clin Orthop Relat Res. 2013;471:2017–2027.
Robinson D, Yassin M, Nevo Z. Cryotherapy of musculoskeletal tumors: from basic science to clinical results. Technol Cancer Res Treat. 2004;3:371–375.
Ruggieri P, Mavrogenis AF, Pala E, Romantini M, Manfrini M, Mercuri M. Outcome of expandable prostheses in children. J Pediatr Orthop. 2013;33:244–253.
Saifuddin A. The accuracy of imaging in the local staging of appendicular osteosarcoma. Skeletal Radiol. 2002;31:191–201.
Saghieh S, Abboud MR, Muwakkit SA, Saab R, Rao B, Haidar R. Seven-year experience of using Repiphysis expandable prosthesis in children with bone tumors. Pediatr Blood Cancer. 2010;55:457–463.
San Julian M, Aquerreta JD, Benito A, Cañadell J. Indications for epiphyseal preservation in metaphyseal malignant bone tumors of children: relationship between image methods and histological findings. J Pediatr Orthop. 1999;19:543–548.
Schinhan M, Tiefenboeck T, Funovics P, Sevelda F, Kotz R, Windhager R. Extendible prostheses for children after resection of primary malignant bone tumor: twenty-seven years of experience. J Bone Joint Surg Am. 2015;97:1585–1591.
Shehadeh A, Noveau J, Malawer M, Henshaw R. Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res. 2010;468:2885–2295.
Tsuchiya H, Nishida H, Srisawat P, Shirai T, Hayashi K, Takeuchi A, Yamamoto N, Tomita K. Pedicle frozen autograft reconstruction in malignant bone tumors. J Orthop Sci. 2010;15:340–349.
Veth R, Schreuder B, van Beem H, Pruszczynski M, de Rooy J. Cryosurgery in aggressive, benign, and low-grade malignant bone tumours. Lancet Oncol. 2005;6:25–34.
Wong KC, Kumta SM, Chiu KH, Antonio GE, Unwin P, Leung KS. Precision tumour resection and reconstruction using image-guided computer navigation. J Bone Joint Surg Br. 2007;89:943–947.
Zimel MN, Cizik AM, Rapp TB, Weisstein JS, Conrad EU 3rd. Megaprosthesis versus condyle-sparing intercalary allograft: distal femoral sarcoma. Clin Orthop Relat Res. 2009;467:2813–2824.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Li, J., Wang, Z., Ji, C. et al. What are the Oncologic and Functional Outcomes After Joint Salvage Resections for Juxtaarticular Osteosarcoma About the Knee?. Clin Orthop Relat Res 475, 2095–2104 (2017). https://doi.org/10.1007/s11999-017-5356-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-017-5356-z