Abstract
Background
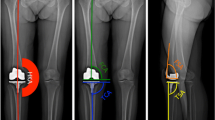
Patient-specific cutting blocks have been touted as a more efficient and reliable means of achieving neutral mechanical alignment during TKA with the proposed downstream effect of improved clinical outcomes. However, it is not clear to what degree published studies support these assumptions.
Questions/purposes
We asked: (1) Do patient-specific cutting blocks achieve neutral mechanical alignment more reliably during TKA when compared with conventional methods? (2) Does patient-specific instrumentation (PSI) provide financial benefit through improved surgical efficiency? (3) Does the use of patient-specific cutting blocks translate to improved clinical results after TKA when compared with conventional instrumentation?
Methods
We performed a systematic review in accordance with Cochrane guidelines of controlled studies (prospective and retrospective) in MEDLINE® and EMBASE® with respect to patient-specific cutting blocks and their effect on alignment, cost, operative time, clinical outcome scores, complications, and survivorship. Sixteen studies (Level I–III on the levels of evidence rubric) were identified and used in addressing the first question, 13 (Level I–III) for the second question, and two (Level III) for the third question. Qualitative assessment of the selected Level I studies was performed using the modified Jadad score; Level II and III studies were rated based on the Newcastle-Ottawa scoring system.
Results
The majority of studies did not show an improvement in overall limb alignment when PSI was compared with standard instrumentation. Mixed results were seen across studies with regard to the prevalence of alignment outliers when PSI was compared with conventional cutting blocks with some studies demonstrating no difference, some showing an improvement with PSI, and a single study showing worse results with PSI. The studies demonstrated mixed results regarding the influence of PSI on operative times. Decreased operative times were not uniformly observed, and when noted, they were found to be of minimal clinical or financial significance. PSI did reliably reduce the number of instrument trays required for processing perioperatively. The accuracy of the preoperative plan, generated by the PSI manufacturers, was found lacking, often leading to multiple intraoperative changes, thereby disrupting the flow of the operation and negatively impacting efficiency. Limited data exist with regard to the effect of PSI on postoperative function, improvement in pain, and patient satisfaction. Neither of the two studies we identified provided strong evidence to support an advantage favoring the use of PSI. No identified studies addressed survivorship of components placed with PSI compared with those placed with standard instrumentation.
Conclusions
PSI for TKA has not reliably demonstrated improvement of postoperative limb or component alignment when compared with standard instrumentation. Although decisive evidence exists to support that PSI requires fewer surgical trays, PSI has not clearly been shown to improve overall surgical efficiency or the cost-effectiveness of TKA. Mid- and long-term data regarding PSI’s effect on functional outcomes and component survivorship do not exist and short-term data are scarce. Limited available literature does not clearly support any improvement of postoperative pain, activity, function, or ROM when PSI is compared with traditional instrumentation.
Similar content being viewed by others
References
Barke S, Musanhu E, Busch C, Stafford G, Field R. Patient-matched total knee arthroplasty: does it offer any clinical advantages? Acta Orthop Belg. 2013;79:307–311.
Barrack RL, Ruh EL, Williams BM, Ford AD, Foreman K, Nunley RM. Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94(Suppl A):95–99.
Barrett W, Hoeffel D, Dalury D, Mason JB, Murphy J, Himden S. In-vivo alignment comparing patient specific instrumentation with both conventional and computer assisted surgery (CAS) instrumentation in total knee arthroplasty. J Arthroplasty. 2014;29:343–347.
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34.
Boonen B, Schotanus MG, Kort NP. Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop. 2012;83:387–393.
Burnett RS, Barrack RL. Computer-assisted total knee arthroplasty is currently of no proven clinical benefit: a systematic review. Clin Orthop Relat Res. 2013;471:264–276.
Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J. 2013;95:354–359.
Chen JY, Yeo SJ, Yew AK, Tay DK, Chia SL, Lo NN, Chin PL. The radiological outcomes of patient-specific instrumentation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:630–635.
Confalonieri N, Manzotti A, Pullen C, Ragone V. Computer-assisted technique versus intramedullary and extramedullary alignment systems in total knee replacement: a radiological comparison. Acta Orthop Belg. 2005;71:703–709.
Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A. Evaluation of the accuracy of a patient-specific instrumentation by navigation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2194–2199.
Daniilidis K, Tibesku CO. A comparison of conventional and patient-specific instruments in total knee arthroplasty. Int Orthop. 2014;38:503–508.
Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(Suppl):39–43.
Hamilton WG, Parks NL, Saxena A. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty. 2013;28(Suppl):96–100.
Heyse TJ, Tibesku CO. Improved femoral component rotation in TKA using patient-specific instrumentation. Knee. 2014;21:268–271.
Issa K, Rifai A, McGrath MS, Callaghan JJ, Wright C, Malkani AL, Mont MA, McInerney VK. Reliability of templating with patient-specific instrumentation in total knee arthroplasty. J Knee Surg. 2013;26:429–433.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17:1–12.
Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22:1097–1106.
Meding JB, Berend ME, Ritter MA, Galley MR, Malinzak RA. Intramedullary vs extramedullary femoral alignment guides: a 15-year follow-up of survivorship. J Arthroplasty. 2011;26:591–595.
Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV Jr. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107.
Noble JW Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27:153–155.
Nunley RM, Ellison BS, Ruh EL, Williams BM, Foreman K, Ford AD, Barrack RL. Are patient-specific cutting blocks cost-effective for total knee arthroplasty? Clin Orthop Relat Res. 2012;470:889–894.
Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res. 2012;470:895–902.
Ottawa Hospital Research Institute. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed June 1, 2014.
Pang CH, Chan WL, Yen CH, Cheng SC, Woo SB, Choi ST, Hui WK, Mak KH. Comparison of total knee arthroplasty using computer-assisted navigation versus conventional guiding systems: a prospective study. J Orthop Surg (Hong Kong). 2009;17:170–173.
Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2213–2219.
Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149.
Pietsch M, Djahani O, Hochegger M, Plattner F, Hofmann S. Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc. 2013;21:2220–2226.
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93:1588–1596.
Scholes C, Sahni V, Lustig S, Parker DA, Coolican MR. Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc. 2014;22:660–665.
Silva A, Sampaio R, Pinto E. Patient-specific instrumentation improves tibial component rotation in TKA. Knee Surg Sports Traumatol Arthrosc. 2014;22:636–642.
Stronach BM, Pelt CE, Erickson J, Peters CL. Patient-specific total knee arthroplasty required frequent surgeon-directed changes. Clin Orthop Relat Res. 2013;471:169–174.
Vundelinckx BJ, Bruckers L, De Mulder K, De Schepper J, Van Esbroeck G. Functional and radiographic short-term outcome evaluation of the Visionaire system, a patient-matched instrumentation system for total knee arthroplasty. J Arthroplasty. 2013;28:964–970.
Yaffe M, Luo M, Goyal N, Chan P, Patel A, Cayo M, Stulberg SD. Clinical, functional, and radiographic outcomes following total knee arthroplasty with patient-specific instrumentation, computer-assisted surgery, and manual instrumentation: a short-term follow-up study. Int J Comput Assist Radiol Surg. 2013 Dec 13 [Epub ahead of print].
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors certifies that he (RN) has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Smith & Nephew, Inc (Memphis, TN, USA), an amount of less than USD 10,000 from Wright Medical Technology, Inc (Memphis, TN, USA), an amount of less than USD 10,000 from Medtronic (Minneapolis, MN, USA), an amount of less than USD 10,000 from CardioMEMS (Atlanta, GA, USA), and an amount of less than USD 10,000 from Integra LifeSciences (Plainsboro, NJ, USA). One of the authors certifies that he (RB) has or may receive payments or benefits, during the study period, an amount of more than USD 1,000,001 from Smith & Nephew, Inc, and an amount of more than USD 1,000,001 from Stryker Orthopaedics.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
About this article
Cite this article
Sassoon, A., Nam, D., Nunley, R. et al. Systematic Review of Patient-specific Instrumentation in Total Knee Arthroplasty: New but Not Improved. Clin Orthop Relat Res 473, 151–158 (2015). https://doi.org/10.1007/s11999-014-3804-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3804-6