Abstract
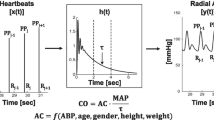
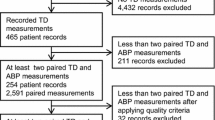
We compared the similarity of cardiac-output (CO) estimates between available bolus thermodilution pulmonary-artery catheters (PAC), arterial pulse-contour analysis (LiDCOplus™, FloTrac™ and PiCCOplus™), and bioreactance (NICOM™). Repetitive simultaneous estimates of CO obtained from the above devices were compared in 21 cardiac-surgery patients during the first 2 h post-surgery. Mean and absolute values for CO across the devices were compared by ANOVA, Bland–Altman, Pearson moment, and linear-regression analyses. Twenty-one simultaneous CO measurements were made before and after therapeutic interventions. Mean PAC CO (5.7 ± 1.5 L min) was similar to LiDCO™, FloTrac™, PiCCO™, and NICOM™ CO (6.0 ± 1.9, 5.9 ± 1.0, 5.7 ± 1.8, 5.3 ± 1.0 L min, respectively). Mean CO bias between each paired method was −0.10 (PAC–LiDCO), 0.18 (PAC–PiCCO), −0.40 (PAC–FloTrac), −0.71 (PAC–NICOM), 0.28 (LiDCO–PiCCO), 0.39 (LiDCO–FloTrac), −0.97 (NICOM–LiDCO), 0.61 (PiCCO–FloTrac), −1.0 (NICOM–FloTrac), −0.73 (NICOM–PiCCO) L/min, with limits of agreement (1.96 SD, ±95% CI) of ± 2.01, ±2.35, ±2.27, ±2.70, ±1.97, ±2.17, ±3.51, ±2.87, ±2.40, and ± 3.14 L min, respectively, and the percentage error for each of the paired devices was 35, 41, 40, 47, 33, 36, 59, 50, 42, and 55%, respectively. From Pearson moment analysis, dynamic changes in CO, estimated by each device, showed good cross-correlations. Although all devices studied recorded similar mean CO values, which dynamically changed in similar directions, they have markedly different bias and precision values relative to each other. Thus, results from prior studies that have used one device to estimate CO cannot be used to validate others devices.





Similar content being viewed by others
Abbreviations
- CO:
-
Cardiac output
- ICU:
-
Intensive-care unit
- PAC:
-
Pulmonary-artery catheter
References
Swan HJ, Ganz W, Forrester J, Marcus H, Diamond G, Chonette D. Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med. 1970;283:447–51.
Gomez CM, Palazzo MG. Pulmonary artery catheterization in anesthesia and intensive care. Br J Anesth. 1998;81:945–56.
Rapoport J, Teres D, Steingrub J, Higgins T, McGee W, Lemeshow S. Patient characteristics and ICU organizational factors that influence frequency of pulmonary artery catheterization. JAMA. 2000;283:2559–67.
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA. 1996;276:889–97.
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, Laporta DP, Viner S, Asserini L, Devitt H, Kirby A, Jacka M. Canadian Critical Care Clinical Trials Group. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5–14.
Harvey S, Harrison DA, Singer M, Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K; PAC-Man study collaboration. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomized controlled trial. Lancet. 2005;366:472–7.
National Heart, Lung, and Blood Institute ARDS. Clinical Trials Network. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354:2213–24.
Hadian M, Pinsky MR. Evidence based of the use of the pulmonary artery catheter: impact data and complications. Crit Care. 2006;10(suppl 3):S11–8.
Wiener RS, Welch HG. Trends in the Use of the Pulmonary Artery Catheter in the United States, 1993–2004. JAMA. 2007;298:423–9.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaesche R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A. Consensus on Circulatory Shock and Hemodynamic Monitoring, Task Force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;49:1795–815.
Hadian M, Kim H, Severyn DA, Pinsky MR. Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care. 2010;14:R212.
Wesseling KH, de Witt B, Weber JAP. A simple device for continuous measurement of cardiac output. Adv Cardiovasc Phys. 1983;5:16–52.
Tannenbaum GA, Mathews D, Weissman C. Pulse contour cardiac output in surgical intensive care unit patients. J Clin Anesth. 1993;5:471–8.
Su NY, Huang CJ, Tsai P, Hsu YW, Hung YC, Cheng CR. Cardiac output measurement during cardiac surgery: esophageal Doppler versus pulmonary artery catheter. Acta Anaesth. 2002;40:127–33.
Dark PM, Singer M. The validity of trans-esophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Intensive Care Med. 2004;30:2060–6.
Barin E, Haryadi D, Schookin S, Westenskow D, Zubenko V, Beliaev K, Morozov A. Evaluation of a thoracic bioimpedance cardiac output monitor during cardiac catheterization. Crit Care Med. 2000;28:698–702.
Engoren M, Barbee D. Comparison of cardiac output determined by bioimpedance, thermodilution, and the Fick method. Am J Crit Care. 2005;4:40–5.
Hamilton WF, Remington W. The measurement of the stroke volume from the pressure pulse. Am J Physiol. 1947;148:14–24.
Hamilton TT, Huber LM, Jessen ME, Pulse CO. a less-invasive method to monitor cardiac output from arterial pressure after cardiac surgery. Ann Thorac Surg. 2002;74:S1408–12.
Pittman J, Bar-Yosef S, SumPing J, Sherwood M, Mark J. Continuous cardiac output monitoring with pulse contour analysis: A comparison with lithium indicator dilution cardiac output measurement. Crit Care Med. 2005;33:2015–2021.
Felbinger TW, Reuter DA, Eltzschig HK, Bayerlein J, Goetz AE. Cardiac index measurement during rapid preload changes: a comparison of pulmonary artery thermodilution with arterial pulse contour analysis. J Clin Anesth. 2005;17:241–8.
Manecke GR. Edwards FloTrac™ sensor and Vigileo™ monitor: easy, accurate, reliable cardiac output assessment using the arterial pulse wave. Expert Rev Med Devices. 2005;2:523–7.
McGee WT, Horswell JL, Calderon J, Janvier G, Van Severen T, Van den Berghe G, Kozikowski L. Validation of a continuous, arterial pressure-based cardiac output measurement: a multicenter, prospective clinical trial. Crit Care. 2007;11:R105.
Opdam HI, Wan L, Bellomo R. A pilot assessment of the FloTrac™ cardiac output monitoring system. Intensive Care Med. 2007;33:344–9.
Mayer J, Boldt J, Schöllhorn T, Röhm KD, Mengistu AM, Suttner S. Semi-invasive monitoring of cardiac output by a new device using arterial pressure waveform analysis: a comparison with intermittent pulmonary artery thermodilution in patients undergoing cardiac surgery. Br J Anaesth. 2007;98:176–82.
Bernstein DP. Continuous noninvasive real-time monitoring of stroke volume and cardiac output by thoracic electrical bioimpedance. Crit Care Med. 1986;14:898–901.
Spiess B, Patel M, Soltow L, Wright I. Comparison of bioimpedance versus thermodilution cardiac output during cardiac surgery: evaluation of a second generation bioimpedance device. J Cardiothorac Vasc Anesth. 2001;15:567–73.
Leslien S, McKee S, Newby D, Webb D, Denvir M. Non-invasive measurement of cardiac output in patients with chronic heart failure. Blood Press Monit. 2004;9:277–80.
Raval NY, Squara P, Cleman M, Yalamanchili K, Winklmaier M, Burkhoff D. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22:113–9.
Squara P, Denjean D, Estagnasie P, Brusset A, Dib JC, Dubois C. Noninvasive cardiac output monitoring (NICOM): a clinical validation. Intensive Care Med. 2007;33:1191–4.
Keren H, Burkhoff D, Squara P. Evaluation of a noninvasive continuous cardiac output monitoring system based on thoracic bioreactance. Am J Physiol. 2007;293:H583–H589.
Marqué S, Cariou A, Chiche JD, Squara P. Comparison between FloTrac-Vigileo and Bioreactance, a totally noninvasive method for cardiac output monitoring. Crit Care. 2009;13:R73.
Myers J, Gujja P, Neelagaru S, Burkhoff D. Cardiac output and cardiopulmonary responses to exercise in heart failure: application of a new bio-reactance device. J Card Fail. 2007;13:629–36.
Maurer MM, Burkhoff D, Maybaum S, Franco V, Vittorio TJ, Williams P, White L, Kamalakkannan G, Myers J, Mancini DM. A multicenter study of noninvasive cardiac output by bioreactance during symptom-limited exercise. J Card Fail. 2009;15:689–99.
Squara P, Cecconi M, Rhodes A, Singer M, Chiche JD. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med. 2009;35:1801–8.
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies–with specific reference to the measurement of cardiac output. Crit Care. 2009;13:201.
Monnet X, Anguel N, Naudin B, Jabot J, Richard C, Teboul JL. Arterial pressure-based cardiac output in septic patients: different accuracy of pulse contour and uncalibrated pressure waveform devices. Crit Care. 2010;14:R109.
Squara P, Rotcajg D, Denjean D, Estagnasie P, Brusset A. Comparison of monitoring performance of Bioreactance vs. pulse contour during lung recruitment maneuvers. Crit Care. 2009;13:R125.
Benomar B, Ouattara A, Estagnasie P, Brusset A, Squara P. Fluid responsiveness predicted by noninvasive bioreactance-based passive leg raise test. Intensive Care Med. 2010;36:1875–81.
Pratt B, Roteluik L, Hatib F, Frazier J, Wallen RD. Calculating arterial pressure-based cardiac output using a novel measurement and analysis method. Biomed Instrument Technol. 2007;41:403–11.
WinDaq Acquisition and Playback Software In-Depth Presentation. 2007. http://www.dataq.com/applicat/index.htm.
Bland JM, Altman DG. Statistical method for assessing agreement between two methods of clinical measurements. Lancet. 1986;1:307–10.
Critchley LAH, Critchley JAJH. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Nguyen HB, Corbett SW, Steele R, Banta J, Clark RT, Hayes SR, Edwards J, Cho TW, Wittlake WA. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med. 2007;35:1105–12.
Donati A, Loggi S, Preiser JC, Orsetti G, Münch C, Gabbanelli V, Pelaia P, Pietropaoli P. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest. 2007;132:1817–24.
Kapoor PM, Kakani M, Chowdhury U, Choudhury M, Lakshmy, Kiran U. Early goal-directed therapy in moderate to high-risk cardiac surgery patients. Ann Card Anaesth. 2008;11:27–34.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial. Crit Care. 2005;9:R687–R693.
Mayer J, Boldt J, Mengistu AM, Röhm KD, Suttner S. Goal-directed intraoperative therapy based on autocalibrated arterial pressure waveform analysis reduces hospital stay in high-risk surgical patients: a randomized, controlled trial. Crit Care. 2010;14:R18.
Cecconi M, Fasano N, Langiano N, Divella M, Costa MG, Rhodes A, Rocca DG. Goal-directed haemodynamic therapy during elective total hip arthroplasty under regional anaesthesia. Crit Care. 2011;15:R132.
Monnet X, Teboul JL. Passive leg raising. Intensive Care Med. 2008;34:659–63.
Marquez J, McCurry K, Severyn DA, Pinsky MR. Ability of pulse power, esophageal Doppler, and arterial pulse pressure to estimate rapid changes in stroke volume in humans. Crit Care Med. 2008;36:3001–7.
Binder JC, Parkin WG. Non-invasive cardiac output determination: comparison of a new partial-rebreathing technique with thermodilution. Anaesth Intensive Care. 2001;29:19–23.
Mahutte CK, Jaffe MB, Chen PA, Sasse SA, Wong DH, Sassoon CS. Oxygen Fick and modified carbon dioxide Fick cardiac outputs. Crit Care Med. 1994;22:86–95.
Johansson A, Chew M. Reliability of continuous pulse contour cardiac output measurement during hemodynamic instability. J Clin Monit Comput. 2007;21:237–42.
Acknowledgements
The authors wish to thank the Cardio thoracic Intensive Care Unit nursing staff at Presbyterian University Hospital, UPMC, for their support in conducting this study. We also appreciate Edwards Life Sciences (Irvine, CA, USA), Pulsion (Munich, Germany), Cheetah Medical (Vancouver, WA, USA), and LiDCO (London, UK) for providing us with the devices, the supplies, and training for this study. This work was supported in part by NIH grants HL67181 and HL073198.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bouchra Lamia, Hyung Kook Kim, Don Severyn: none declared. Michael R. Pinsky is a member of the medical advisory boards for LiDCO Ltd and Edwards LifeSciences, Inc. He has stock options with LiDCO Ltd and Cheetah Medical. He has received honoraria for lectures from Edwards LifeSciences, LiDCO, and Cheetah Medical. He has received financial support to conduct laboratory research from Pulsion Ltd.
Research involving human participants and informed consent
Our Institutional Review Board approved the study and all subjects signed their informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lamia, B., Kim, H.K., Severyn, D.A. et al. Cross-comparisons of trending accuracies of continuous cardiac-output measurements: pulse contour analysis, bioreactance, and pulmonary-artery catheter. J Clin Monit Comput 32, 33–43 (2018). https://doi.org/10.1007/s10877-017-9983-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-017-9983-4