Abstract
Background
Salivary secretion in patients with proton-pump inhibitor (PPI)-resistant severe reflux esophagitis has not been examined. In this study, saliva secretion and salivary epidermal growth factor (EGF) in patients with PPI-resistant severe reflux esophagitis were investigated.
Methods
We recruited 22 PPI-resistant and 22 PPI-responsive severe reflux esophagitis patients who were not infected with Helicobacter pylori. Saliva secretion testing and esophageal manometry using high-resolution manometry were performed. Saliva secretion was assessed as follows: each patient chewed sugar-free gum for 3 min prior to endoscopy and the amount and pH of saliva as well as the pH of saliva after acid loading as an index of the acid-buffering capacity were measured. The salivary EGF concentration was assessed by ELISA.
Results
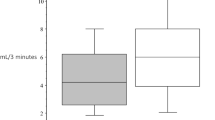
The amount of saliva secreted was significantly lower in the PPI-resistant group than in the PPI-responsive group, with medians (25th-75th percentile) of 3.7 (2.2–6.8) and 4.9 (4.0–7.8) mL, respectively (p = 0.029). Salivary pH was significantly lower in the PPI-resistant group [6.9 (6.7–7.2)] than in the PPI-responsive group [7.2 (7.1–7.4), p = 0.001]. Salivary pH after acid loading was significantly lower in the PPI-resistant group [5.6 (5.3–5.9)] than in the PPI-responsive group [6.4 (6.1–6.5), p = 0.002]. The salivary EGF concentration was significantly higher in the PPI-resistant group [3211.5 (1865.0–4121.5)] than in the PPI-responsive group [1816.0 (1123.5–2792.3), p = 0.041]. No significant differences were observed in the proportion of esophageal motility abnormalities.
Conclusion
Stimulated saliva secretion was reduced in PPI-resistant severe reflux esophagitis patients.





Similar content being viewed by others
References
Iwakiri K, Kinoshita Y, Habu Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51:751–67.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Kahrilas PJ, Dodds WJ, Hogan WJ, et al. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986;91:897–904.
Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988;94:73–80.
Helm JF, Dodds WJ, Riedel DR, et al. Determinants of esophageal acid clearance in normal subjects. Gastroenterology. 1983;85:607–12.
Helm JF, Dodds WJ, Pelc LR, et al. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med. 1984;31:284–8.
Mizuno H, Matsuhashi N, Sakaguchi M, et al. Recent effectiveness of proton pump inhibitors for severe reflux esophagitis: the first multicenter prospective study in Japan. J Clin Biochem Nutr. 2015;57:233–8.
Fujimoto K, Hongo M. Risk factors for relapse of erosive GERD during long-term maintenance treatment with proton pump inhibitor: a prospective multicenter study in Japan. J Gastroenterol. 2010;45:1193–200.
Furuta T, Shimatani T, Sugimoto M, et al. Investigation of pretreatment prediction of proton pump inhibitor (PPI)-resistant patients with gastroesophageal reflux disease and the dose escalation challenge of PPIs-TORNADO study: a multicenter prospective study by the acid-related symptom research group in Japan. J Gastroenterol. 2011;46:1273–83.
Sugiura T, Iwakiri K, Kotoyori M, et al. Relationship between severity of reflux esophagitis according to the Los Angeles classification and esophageal motility. J Gastroenterol. 2001;36:226–30.
Kao CH, Ho YJ, ChangLai SP, et al. Evidence for decreased salivary function in patients with reflux esophagitis. Digestion. 1999;60:191–5.
Orr WC, Chen CL, Sloan S. The role of age and salivation in acid clearance in symptomatic patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2001;15:1385–8.
Shafik A, El-Sibai O, Shafik AA, et al. Effect of topical esophageal acidification on salivary secretion: identification of the mechanism of action. J Gastroenterol Hepatol. 2005;20:1935–9.
Fujinami H, Kudo T, Miyazaki T, et al. The modified glucose clearance test: a novel non-invasive method for differentiating non-erosive reflux disease and erosive oesophagitis. Aliment Pharmacol Ther. 2008;28:1259–64.
Manabe N, Haruma K, Kusunoki H, et al. Differences in salivary secretory function between patients with erosive esophagitis and those with nonerosive reflux disease. J Gastroenterol Hepatol. 2018;33:807–13.
Sonnenberg A, Steinkamp U, Weise A, et al. Salivary secretion in reflux esophagitis. Gastroenterology. 1982;83:889–95.
Sarosiek J, Scheurich CJ, Marcinkiewicz M, et al. Enhancement of salivary esophagoprotection: Rationale for a physiological approach to gastroesophageal reflux disease. Gastroenterology. 1996;110:675–81.
Hoshino S, Kawami N, Takenouchi N, et al. Efficacy of vonoprazan for proton pump inhibitor-resistant reflux esophagitis. Digestion. 2017;95:156–61.
Tanabe T, Hoshino S, Kawami N, et al. Efficacy of long term maintenance therapy with 10-mg vonoprazan for proton-pump inhibitor-resistant reflux esophagitis. Esophagus. 2019;16:377–81.
Konturek JW, Bielanski W, Konturek SJ, et al. Distribution and release of epidermal growth factor in man. Gut. 1989;30:1194–200.
Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;3:87–97.
Kitasako Y, Moritsuka M, Foxton RM, et al. Simplified and quantitative saliva buffer capacity test using a hand-held pH meter. Am J Dent. 2005;18:147–50.
Moritsuka M, Kitasako Y, Burrow MF, et al. The pH change after HCl titration into resting and stimulated saliva for a buffering capacity test. Aust Dent J. 2006;51:170–4.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74.
Kuribayashi S, Iwakiri K, Shinozaki T, et al. Clinical impact of different cut-off values in high-resolution manometry systems on diagnosing esophageal motility disorders. J Gastroenterol. 2019;54:1078–82.
Ariizumi K, Ohara S, Koike T, et al. Therapeutic effects of 10 mg/day rabeprazole administration on reflux esophagitis was not influenced by the CYP2C19 polymorphism. J Gastroenterol Hepatol. 2006;21:1428–34.
Ashida K, Sakurai Y, Hori T, et al. Randomised clinical trial: vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the healing of erosive oesophagitis. Aliment Pharmacol Ther. 2016;43:240–51.
Iijima K, Ohara S, Sekine H, et al. A new endoscopic method of gastric acid secretory testing. Am J Gastroenterol. 1998;93:2113–8.
Hanada Y, Hoshino S, Hoshikawa Y, et al. Endoscopic diagnosis of hiatus hernia under deep inspiration is not consistent with esophageal manometric diagnosis. J Gastroenterol. 2018;53:712–7.
Dawes C. Physiological factors affecting salivary flow rate, oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648–53.
Yandrapu H, Marcinkiewicz M, Poplawski C, et al. Role of Saliva in esophageal defense: implications in patients with nonerosive reflux disease. Am J Med Sci. 2015;349:385–91.
Brown GL, Nanney LB, Griffen J, et al. Enhancement of wound healing by topical treatment with epidermal growth factor. N Engl J Med. 1989;321:76–9.
Pedersen W, Schubert M, Izutsu K, et al. Age-dependent decreases in human submandibular gland flow rates as measured under resting and post stimulated conditions. J Dent Res. 1985;64:822–5.
Gandara BK, Izutsu KT, Truelove EL, et al. Age-related salivary flow rate changes in controls and patients with oral lichen planus. J Dent Res. 1985;64:1149–51.
Baum BJ. Evaluation of stimulated parotid saliva flow rate in different age groups. J Dent Res. 1985;60:1292–6.
Shalev A, Szargel R, Laor A, et al. The salivary flow rate and composition of whole and parotid resting and stimulated saliva in young and old healthy subjects. Biochem Med Metab Biol. 1986;36:260–5.
Inoue H, Ono K, Masuda W, et al. Gender difference in unstimulated whole saliva flow rate and salivary gland sizes. Arch Oral Biol. 2006;51:1055–60.
Rourk RM, Namiot Z, Edmunds MC, et al. Diminished luminal release of esophageal epidermal growth factor in patients with reflux esophagitis. Am J Gastroenterol. 1994;89:1177–84.
Benamouzig R, Ferrière F, Guettier C, et al. Role of salivary and seric epidermal growth factor in pathogenesis of reflux esophagitis in chronic alcoholics and nondrinkers. Dig Dis Sci. 1996;41:1595–9.
Gray MR, Donnelly RJ, Kingsnorth AN. Role of salivary epidermal growth factor in the pathogenesis of Barrett’s columnar lined oesophagus. Br J Surg. 1991;78:1461–6.
Noguchi S, Ohba Y, Oka T. Effect of salivary epidermal growth factor on wound healing of tongue in mice. Am J Physiol. 1991;260(4 Pt 1):E620–5.
Acknowledgements
The authors thank Ms. Satoko Nishimura for her administrative assistance.
Funding
This work was supported by JSPS KAKENHI Grant Number JP20K082973.
Author information
Authors and Affiliations
Contributions
TT: tanabe@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. MK: m-koeda@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. YK: kitaodnt@tmd.ac.jp: Cariology and Operative Dentistry, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University,1-5-45 Yushima, Bunkyo-ku, Tokyo, Japan. EM: eri-momma@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. YH: y-hoshikawa@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. SH: hoshino.tmhccm@rd5.so-net.ne.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. NK: s5038@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1–1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. MK: m-kaise@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan. KI: k-iwa@nms.ac.jp: Nippon Medical School, Graduate School of Medicine, 1-1-5, Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan.
Corresponding author
Ethics declarations
Ethical statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
Conflict of interest
Katsuhiko Iwakiri has received lecture fees from Takeda Pharmaceutical Co., Ltd. and Otsuka Pharmaceutical Co., Ltd. The remaining authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tanabe, T., Koeda, M., Kitasako, Y. et al. Stimulated saliva secretion is reduced in proton pump inhibitor-resistant severe reflux esophagitis patients. Esophagus 18, 676–683 (2021). https://doi.org/10.1007/s10388-021-00825-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00825-1