Abstract
Backgrounds
Some non-erosive reflux disease (NERD) and reflux esophagitis (RE) patients are unresponsive to a proton pump inhibitor (PPI) at standard dose. We investigated the predictive marker of the efficacy of PPI for GERD patients including NERD and RE treated with standard and increased doses of a PPI.
Methods
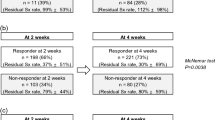
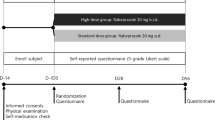
Patients with symptomatic gastroesophageal reflux disease (GERD) (NERD and RE) were treated with rabeprazole (RPZ) 10 mg once daily for 4 weeks. The RPZ dosage was increased to 10 mg twice daily for an additional 2 weeks and again to 20 mg twice daily for another 2 weeks if heartburn was not relieved. Baseline characteristics and efficacy of RPZ were assessed on the basis of a heartburn diary and frequency scale for symptoms of GERD (FSSG).
Results
Complete heartburn relief rates after 4 weeks were 42.5% (31/73) and 67.9% (19/28) in NERD and RE groups, respectively, which rose to 68.9 and 91.7% after dose escalation. Multivariate analysis revealed that parameters associated with resistance to RPZ 10 mg once daily were female, non-smoking, frequent heartburn, low score for question 4 (Q4) of the FSSG (subconsciously rubbing the chest), and high scores for Q3 (heavy stomach after meal) and Q7 (unusual sensation in the throat). Frequent heartburn and a high score for Q7 were associated with resistance to RPZ 20 mg twice daily. FSSG scores of patients resistant to RPZ were significantly higher in comparison with responders before and during treatment.
Conclusions
FSSG could predict response to a PPI for symptomatic GERD. Increase of RPZ dose is useful for treatment of GERD refractory to the standard dose of RPZ.





Similar content being viewed by others
References
Cloud ML, Enas N, Humphries TJ, Bassion S. Rabeprazole in treatment of acid peptic diseases: results of three placebo-controlled dose-response clinical trials in duodenal ulcer, gastric ulcer, and gastroesophageal reflux disease (GERD). Dig Dis Sci. 1998;43(5):993–1000.
Robinson M, Fitzgerald S, Hegedus R, Murthy A, Jokubaitis L, FAST Trial Investigators. Onset of symptom relief with rabeprazole: a community-based, open-label assessment of patients with erosive oesophagitis. Aliment Pharmacol Ther. 2002;16(3):445–54 (Erratum in: Aliment Pharmacol Ther. 2002;16(5):1035).
Miner P Jr, Orr W, Filippone J, Jokubaitis L, Sloan S. Rabeprazole in nonerosive gastroesophageal reflux disease: a randomized placebo-controlled trial. Am J Gastroenterol. 2002;97(6):1332–9.
Miwa H, Sasaki M, Furuta T, Koike T, Habu Y, Ito M, et al. Efficacy of rabeprazole on heartburn symptom resolution in patients with non-erosive and erosive gastro-oesophageal reflux disease: a multicenter study from Japan. Aliment Pharmacol Ther. 2007;26(1):69–77.
Miyamoto M, Haruma K, Takeuchi K, Kuwabara M. Frequency scale for symptoms of gastroesophageal reflux disease predicts the need for addition of prokinetics to proton pump inhibitor therapy. J Gastroenterol Hepatol. 2008;23(5):746–51.
Fass R. Proton pump inhibitor failure—what are the therapeutic options? Am J Gastroenterol. 2009;104(Suppl 2):S33–8.
Bredenoord AJ, Smout AJ. Refractory gastrooesophageal reflux disease. Eur J Gastroenterol Hepatol. 2008;20(3):217–23.
Hershcovici T, Fass R. Management of gastroesophageal reflux disease that does not respond well to proton pump inhibitors. Curr Opin Gastroenterol. 2010;26(4):367–78.
Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006;41(2):95–9.
Uemura N, Inokuchi H, Serizawa H, Chikama T, Yamauchi M, Tsuru T, et al. Efficacy and safety of omeprazole in Japanese patients with nonerosive reflux disease. J Gastroenterol. 2008;43(9):670–8.
Fujiwara Y, Higuchi K, Nebiki H, Chono S, Uno H, Kitada K, et al. Famotidine vs. omeprazole: a prospective randomized multicentre trial to determine efficacy in non-erosive gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2005;21(Suppl 2):10–8.
Furuta T, Shirai N, Watanabe F, Honda S, Takeuchi K, Iida T, et al. Effect of cytochrome P4502C19 genotypic differences on cure rates for gastroesophageal reflux disease by lansoprazole. Clin Pharmacol Ther. 2002;72(4):453–60.
Furuta T, Shirai N, Sugimoto M, Ohashi K, Ishizaki T. Pharmacogenomics of proton pump inhibitors. Pharmacogenomics. 2004;5(2):181–202.
Furuta T, Shirai N, Sugimoto M, Nakamura A, Hishida A, Ishizaki T. Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies. Drug Metab Pharmacokinet. 2005;20(3):153–67.
Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, et al. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39(9):888–91.
Kusano M, Shimoyama Y, Kawamura O, Maeda M, Kuribayashi S, Nagoshi A, et al. Proton pump inhibitors improve acid-related dyspepsia in gastroesophageal reflux disease patients. Dig Dis Sci. 2007;52(7):1673–7.
Bytzer P. Goals of therapy and guidelines for treatment success in symptomatic gastroesophageal reflux disease patients. Am J Gastroenterol. 2003;98(3 Suppl):S31–9.
Hatlebakk JG, Katz PO, Camacho-Lobato L, Castell DO. Proton pump inhibitors: better acid suppression when taken before a meal than without a meal. Aliment Pharmacol Ther. 2000;14(10):1267–72.
Shimatani T, Inoue M, Kuroiwa T, Horikawa Y. Rabeprazole 10 mg twice daily is superior to 20 mg once daily for night-time gastric acid suppression. Aliment Pharmacol Ther. 2004;19(1):113–22.
Shimatani T, Moriwaki M, Xu J, Tazuma S, Inoue M. Acid-suppressive effects of rabeprazole: comparing 10 mg and 20 mg twice daily in Japanese Helicobacter pylori-negative and -positive CYP2C19 extensive metabolisers. Dig Liver Dis. 2006;38(11):802–8.
Dean BB, Gano AD Jr, Knight K, Ofman JJ, Fass R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2004;2(8):656–64.
Kamolz T, Velanovich V. Psychological and emotional aspects of gastroesophageal reflux disease. Dis Esophagus. 2002;15(3):199–203.
Frazzoni M, De Micheli E, Grisendi A, Savarino V. Hiatal hernia is the key factor determining the lansoprazole dosage required for effective intra-oesophageal acid suppression. Aliment Pharmacol Ther. 2002;16(5):881–6.
Holtmann G, Cain C, Malfertheiner P. Gastric Helicobacter pylori infection accelerates healing of reflux esophagitis during treatment with the proton pump inhibitor pantoprazole. Gastroenterology. 1999;117(1):11–6.
Acknowledgments
Eisai Co., Ltd. made a contribution with no restrictions on use.
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The authors of the Acid-Related Symptom (ARS) Research Group are given in the Appendix.
Appendix: Members of the ARS (Acid-Related Symptom) Research Group
Appendix: Members of the ARS (Acid-Related Symptom) Research Group
Shuichi Ohara, Department of Gastroenterology, Tohoku Rosai Hospital, Sendai, Japan; Yasuyuki Shimoyama, Department of Endoscopy and Endoscopic Surgery, Gunma University Hospital, Maebashi, Japan; Osamu Kawamura, Department of Medicine and Molecular Science, Gunma University Graduate School of Medicine, Maebashi, Japan; Yoshio Hoshihara, Clinic of the Ministry of Economy, Trade and Industry, Tokyo, Japan; Kouji Yakabi and Susumu Kurosawa, Department of Gastroenterology and Hepatology, Saitama Medical Center, Saitama Medical University, Kawagoe, Japan; Yusuke Watanabe, Department of Otorhinolaryngology, International University of Health and Welfare Mita Hospital, Tokyo, Japan; Masafumi Nishino, First Department of Medicine, Hamamatsu University School of Medicine, Hamamatsu, Japan; Takashi Joh, Makoto Sasaki and Tsuneya Wada, Department of Gastroenterology and Metabolism, Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan; Kazuhide Higuchi, Second Department of Internal Medicine, Osaka Medical College, Takatsuki, Japan; Yasuki Habu, Department of Gastroenterology, Saiseikai Noe Hospital, Osaka, Japan; Hiroto Miwa, Tadayuki Oshima and Junji Tanaka, Division of Upper Gastroenterology, Department of Internal Medicine, Hyogo College of Medicine, Nishinomiya, Japan; Ken Haruma, Division of Gastroenterology, Department of Internal Medicine, Kawasaki Medical School, Kurashiki, Japan; Noriaki Manabe, Division of Endoscopy and Ultrasonography, Kawasaki Medical School, Kurashiki, Japan; Kyoichi Adachi, Department of Clinical Nursing, Shimane University Faculty of Medicine, Izumo, Japan; Kenji Furuta, Department of Internal Medicine II, Shimane University Faculty of Medicine, Izumo, Japan; Masanori Ito, Department of Medicine and Molecular Science, Hiroshima University, Hiroshima, Japan; Kazuma Fujimoto, Department of Internal Medicine, Saga Medical School, Saga, Japan.
Rights and permissions
About this article
Cite this article
Furuta, T., Shimatani, T., Sugimoto, M. et al. Investigation of pretreatment prediction of proton pump inhibitor (PPI)-resistant patients with gastroesophageal reflux disease and the dose escalation challenge of PPIs—TORNADO study: a multicenter prospective study by the Acid-Related Symptom Research Group in Japan. J Gastroenterol 46, 1273–1283 (2011). https://doi.org/10.1007/s00535-011-0446-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0446-2