Abstract
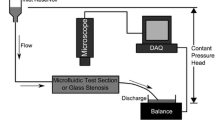
While cardiovascular device-induced thrombosis is associated with negative patient outcomes, the convoluted nature of the processes resulting in a thrombus makes the full thrombotic network too computationally expensive to simulate in the complex geometries and flow fields associated with devices. A macroscopic, continuum computational model is developed based on a simplified network, which includes terms for platelet activation (chemical and mechanical) and thrombus deposition and growth in regions of low wall shear stress (WSS). Laminar simulations are performed in a two-dimensional asymmetric sudden expansion geometry and compared with in vitro thrombus size data collected using whole bovine blood. Additionally, the predictive power of the model is tested in a flow cell containing a series of symmetric sudden expansions and contractions. Thrombi form in the low WSS area downstream of the asymmetric expansion and grow into the nearby recirculation region, and thrombus height and length largely remain within 95 % confidence intervals calculated from the in vitro data for 30 min of blood flow. After 30 min, predicted thrombus height and length are 0.94 and 4.32 (normalized by the 2.5 mm step height). Importantly, the model also correctly predicts locations of thrombus deposition observed in the in vitro flow cell of expansions and contractions. As the simulation results, which rely on a greatly reduced model of the thrombotic network, are still able to capture the macroscopic behavior of the full network, the model shows promise for timely predictions of device-induced thrombosis toward optimizing and expediting the device development process.










Similar content being viewed by others
Abbreviations
- \({\varvec{u}}\) :
-
Velocity
- p :
-
Pressure
- t :
-
Time
- \(\nu \) :
-
Kinematic viscosity
- \(\rho \) :
-
Density
- F :
-
Modified Brinkman function
- \(\varepsilon \) :
-
Aggregation intensity
- \(\varepsilon _\mathrm{t}\) :
-
Aggregation intensity threshold
- k :
-
Thrombus permeability
- Q :
-
Arbitrary scalar quantity
- D :
-
Diffusivity
- R :
-
Sources and sinks
- \(\phi _\mathrm{n}\) :
-
Non-activated platelet concentration
- \(\phi _\mathrm{a}\) :
-
Activated platelet concentration
- \(D_\mathrm{n}\) :
-
Diffusion coefficient for non-activated platelets
- \(D_\mathrm{a}\) :
-
Diffusion coefficient for activated platelets
- \(A_\mathrm{C}\) :
-
Chemical platelet activation rate
- ADP:
-
Adenosine diphosphate (ADP) concentration
- \(\mathrm{ADP}_\mathrm{t}\) :
-
ADP threshold for chemical activation
- \(t_\mathrm{ADP}\) :
-
Characteristic time for chemical activation
- \(A_\mathrm{M}\) :
-
Mechanical platelet activation rate
- \(\tau \) :
-
Scalar shear stress
- \(\bar{{\bar{\varvec{\sigma }}}}\) :
-
Viscous stress tensor
- \(\phi _\mathrm{f}\) :
-
Activated platelet fraction
- C :
-
Power law coefficient
- \(\alpha \) :
-
Power law coefficient
- \(\beta \) :
-
Power law coefficient
- \(D_\mathrm{ADP}\) :
-
Diffusion coefficient for ADP
- \(R_\mathrm{ADP}\) :
-
Amount of ADP in a platelet
- \(\alpha _\varepsilon \) :
-
Thrombus volumetric growth rate
- \(\tau _\mathrm{w}\) :
-
Wall shear stress (WSS)
- \(P_\mathrm{TSP}\) :
-
Weighting function for thrombus deposition /growth
- \(\tau _\mathrm{low,wall}\) :
-
Low WSS threshold for thrombus deposition
- \(\tau _\mathrm{high,wall}\) :
-
High WSS threshold for thrombus deposition
- \(\tau _\mathrm{low,thrombus}\) :
-
Low WSS threshold for thrombus growth
- \(\tau _\mathrm{high,thrombus}\) :
-
High WSS threshold for thrombus growth
- \(\beta _\varepsilon \) :
-
Thrombus breakdown function
- B :
-
Thrombus breakdown rate
- \(\tau _\mathrm{breakdown,wall}\) :
-
WSS threshold for thrombus breakdown at a wall
- \(\tau _\mathrm{breakdown,thrombus}\) :
-
WSS threshold for thrombus breakdown at a thrombus surface
- U :
-
Average inlet velocity
- h :
-
Step height
- \(\phi _{\mathrm{a},i}\) :
-
Initial (background) concentration of activated platelets
- \(\phi _{\mathrm{n},i}\) :
-
Initial concentration of non-activated platelets
- \(t_{\mathrm{G}}\) :
-
Characteristic thrombus growth time
- H :
-
Thrombus height
- L :
-
Thrombus length
References
Adolph R, Vorp DA, Steed DL, Webster MW, Kameneva MV, Watkins SC (1997) Cellular content and permeability of intraluminal thrombus in abdominal aortic aneurysm. J Vasc Surg 25(5):916–926. doi:10.1016/S0741-5214(97)70223-4
Armaly BF, Durst F, Pereira JCF, Schonung B (1983) Experimental and theoretical investigation of backward-facing step flow. J Fluid Mech 127:473–496. doi:10.1017/S0022112083002839
Basmadjian D (1989) Embolization: critical thrombus height, shear rates, and pulsatility. Patency of blood vessels. J Biomed Mater Res 23(11):1315–1326. doi:10.1002/jbm.820231108
Bludszuweit C (1994) A theoretical approach to the prediction of haemolysis in centrifugal blood pumps. Dissertation, University of Strathclyde
Bluestein D, Niu L, Schoephoerster RT, Dewanjee MK (1996) Steady flow in an aneurysm model: correlation between fluid dynamics and blood platelet deposition. J Biomech Eng 118:280–286. doi:10.1115/1.2796008
Cito S (2013) Review of macroscopic thrombus modeling methods. Thromb Res 131:116–124. doi:10.1016/j.thromres.2012.11.020
Fogelson AL (1992) Continuum models of platelet aggregation: formulation and mechanical properties. SIAM J Appl Math 52(4):1089–1110. doi:10.1137/0152064
Fogelson AL, Guy RD (2008) Immersed-boundary-type models of intravascular platelet aggregation. Comput Methods Appl Mech Eng 197:2087–2104. doi:10.1016/j.cma.2007.06.030
Folie BJ, McIntire LV (1989) Mathematical analysis of mural thrombogenesis: concentration profiles of platelet-activating agents and effects of viscous shear flow. Biophys J 56(6):1121–1141. doi:10.1016/S0006-3495(89)82760-2
Frojmovic MM, Mooney RF, Wong T (1994) Dynamics of platelet glycoprotein IIb–IIIa receptor expression and fibrinogen binding. I. Quantal activation of platelet subpopulations varies with adenosine diphosphate concentration. Biophys J 67:2060–2068. doi:10.1016/S0006-3495(94)80689-7
Gear AR (1982) Rapid reactions of platelets studied by a quenched-flow approach: aggregation kinetics. J Lab Clin Med 100(6):866–886. doi:10.1111/j.1365-2141.1984.tb03969.x
Goldsmith HL, Turitto VT (1986) Rehological aspects of thrombosis and haemostasis: basic principles and applications. ICTH-Report-Subcommittee on Rheology of the International Committee on Thrombosis and Haemostasis. Thrombo Haemost 55(3):415–435 ISSN: 0340-6245
Goodman PD, Barlow ET, Crapo PM, Mohammad SF, Solen KA (2005) Computational model of device-induced thrombosis and thromboembolism. Ann Biomed Eng 33(6):780–797. doi:10.1007/s10439-005-2951-z
Gottschall JL, Rzad L, Aster RH (1986) Studies of the minimum temperature at which human platelets can be stored with full maintenance of viability. Transfusion 26(5):460–462. doi:10.1046/j.1537-2995.1986.26587020126.x
Guj G, Stella F (1988) Numerical solutions of high-Re recirculating flows in vorticity-velocity form. Int J Numer Methods Fluids 8(4):405–416. doi:10.1002/fld.1650080404
Hansen KB, Arzani A, Shadden SC (2015) Mechanical platelet activation in abdominal aortic aneurysms. J Biomech Eng 137:041005–1–8. doi:10.1115/1.4029580
Holme S, Heaton A (1995) In vitro platelet ageing at 22 \(^{\circ }\)C is reduced compared to in vivo ageing at 37 \(^{\circ }\)C. Br J Haematol 91(1):212–218. doi:10.1111/j.1365-2141.1995.tb05272.x
Holmsen H, Weiss HJ (1979) Secretable storage pools in platelets. Ann Rev Med 30:119–134. doi:10.1146/annurev.me.30.020179.001003
Hubbell JA, McIntire LV (1986a) Platelet active concentration profiles near growing thrombi. Biophys J 50:937–945. doi:10.1016/S0006-3495(86)83535-4
Hubbell JA, McIntire LV (1986b) Visualization and analysis of mural thrombogenesis on collagen, polyurethane and nylon. Biomaterials 7:354–363. doi:10.1016/0142-9612(86)90006-2
Karino T, Goldsmith HL (1979) Adhesion of human platelets to collagen on the walls distal to a tubular expansion. Microvasc Res 17:238–262. doi:10.1016/S0026-2862(79)80002-3
Kennedy SD, Igarashi Y, Kickler TS (1997) Measurement of in vitro P-selectin expression by flow cytometry. Am J Clin Pathol 107:99–104 ISSN: 0002-9173
Leiderman K, Fogelson AL (2011) Grow with the flow: a spatial-temporal model of platelet deposition and blood coagulation under flow. Math Med Biol 28:47–84. doi:10.1093/imammb/dqq005
Leiderman K, Fogelson AL (2014) An overview of mathematical modeling of thrombus formation under flow. Thromb Res 133:S12–S14. doi:10.1016/j.thromres.2014.03.005
Medvitz RM (2008) Development and validation of a computational fluid dynamics methodology for pulsatile blood pump design and prediction of thrombus potential. Ph.D. Dissertation, The Pennsylvania State University
Navitsky MA, Taylor JO, Smith AB, Slattery MJ, Deutsch S, Siedlecki CA, Manning KB (2014) Platelet adhesion to polyurethane urea under pulsatile flow conditions. Artif Organs 38(12):1046–1053. doi:10.1111/aor.12296
Roache PJ (1994) Perspective—a method for uniform reporting of grid refinement studies. ASME J Fluids Eng 116(3):405–413. doi:10.1115/1.2910291
Samra S (2011) Numerical implementation of a continuum platelet aggregation model. M.S. Thesis, The Pennsylvania State University
Soares JS, Sheriff J, Bluestein D (2013) A novel mathematical model of activation and sensitization of platelets subjected to dynamic stress histories. Biomech Model Mechanobiol 12:1127–1141. doi:10.1007/s10237-013-0469-0
Sohn JL (1988) Evaluation of FIDAP on some classical laminar and turbulent benchmarks. Int J Numer Methods Fluids 8(12):1469–1490. doi:10.1002/fld.1650081202
Soloviev MV, Okazaki Y, Harasaki H (1999) Whole blood platelet aggregation in humans and animals: a comparative study. J Surg Res 82(2):180–187. doi:10.1006/jsre.1998.5543
Sorensen EN, Burgreen GW, Wagner WR, Antaki JF (1999a) Computational simulation of platelet deposition and activation: I. Model development and properties. Ann Biomed Eng 27:436–438. doi:10.1114/1.200
Sorensen EN, Burgreen GW, Wagner WR, Antaki JF (1999b) Computational simulation of platelet deposition and activation: II. Results for Poiseuille flow over collagen. Ann Biomed Eng 27:449–458. doi:10.1114/1.201
Tamagawa M, Kaneda H, Hiramoto M, Nagahama S (2009) Simulation of thrombus formation in shear flows using lattice Boltzmann method. Artif Organs 33(8):604–610. doi:10.1111/j.1525-1594.2009.00782.x
Taylor JO, Witmer KP, Neuberger T, Craven BA, Meyer RS, Deutsch S, Manning KB (2014) In vitro quantification of time dependent thrombus size using magnetic resonance imaging and computational simulations of thrombus surface shear stresses. J Biomech Eng 136:071012. doi:10.1115/1.4027613
Topper SR, Navitsky MA, Medvitz RB, Paterson EG, Siedlecki CA, Slattery MJ, Deutsch S, Rosenberg G, Manning KB (2014) The use of fluid mechanics to predict regions of microscopic thrombus formation in pulsatile VADs. Cardiovasc Eng Technol 5(1):54–69. doi:10.1007/s13239-014-0174-x
Wang W, King MR (2012) Multiscale modeling of platelet adhesion and thrombus growth. Ann Biomed Eng 40(11):2345–2354. doi:10.1007/s10439-012-0558-8
Welsh JD, Stalker TJ, Voronov R, Muthard RW, Tomaiuolo M, Diamond SL, Brass LF (2014) A systems approach to hemostasis: 1. The interdependence of thrombus architecture and agonist movements in the gaps between platelets. Blood 124(11):1808–1815. doi:10.1182/blood-2014-01-550335
Williams PT, Baker AJ (1997) Numerical simulations of laminar flow over a 3D backward-facing step. Int J Numer Methods Fluids 24(11):1159–1183. doi:10.1002/(SICI)1097-0363(19970615)24:11<1159::AID-FLD534>3.0.CO;2-R
Wufsus AR, Macera NE, Neeves KB (2013) The hydraulic permeability of blood clots as a function of fibrin and platelet density. Biophys J 104(8):1812–1823. doi:10.1016/j.bpj.2013.02.055
Xu Z, Chen N, Kamocka MM, Rosen ED, Alber M (2008) A multiscale model of thrombus development. J R Soc Interface 5:705–722. doi:10.1098/rsif.2007.1202
Xu Z, Chen N, Shadden SC, Marsden JE, Kamocka MM, Rosen ED, Alber M (2009) Study of blood flow impact on growth of thrombi using a multiscale model. Soft Matter 5:769–779. doi:10.1039/B812429A
Xu Z, Lioi J, Mu J, Kamocka MM, Liu X, Chen DZ, Rosen ED, Alber M (2010) A multiscale model of venous thrombus formation with surface-mediated control of blood coagulation cascade. Biophys J 98:1723–1732. doi:10.1016/j.bpj.2009.12.4331
Xu Z, Kamocka M, Alber M, Rosen ED (2011) Computational approaches to studying thrombus development. Arterioscler Thromb Vasc Biol 31(3):500–505. doi:10.1161/ATVBAHA.110.213397
Acknowledgments
A Walker Graduate Assistantship from the Applied Research Laboratory at the Pennsylvania State University and a Penn State Grace Woodward Foundation grant supported this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taylor, J.O., Meyer, R.S., Deutsch, S. et al. Development of a computational model for macroscopic predictions of device-induced thrombosis. Biomech Model Mechanobiol 15, 1713–1731 (2016). https://doi.org/10.1007/s10237-016-0793-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-016-0793-2