Abstract
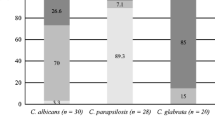
Candida albicans is classified into different serotypes according to cell wall mannan composition and cell surface hydrophobicity. Since the effectiveness of photodynamic therapy (PDT) depends on the cell wall structure of microorganisms, the objective of this study was to compare the sensitivity of in vitro biofilms of C. albicans serotypes A and B to antimicrobial PDT. Reference strains of C. albicans serotype A (ATCC 36801) and serotype B (ATCC 36802) were used for the assays. A gallium-aluminum-arsenide laser (660 nm) was used as the light source and methylene blue (300 μM) as the photosensitizer. After biofilm formation on the bottom of a 96-well microplate for 48 h, each Candida strain was submitted to assays: PDT consisting of laser and photosensitizer application (L + P+), laser application alone (L + P−), photosensitizer application alone (L−P+), and application of saline as control (L−P−). After treatment, biofilm cells were scraped off and transferred to tubes containing PBS. The content of the tubes was homogenized, diluted, and seeded onto Sabouraud agar plates to determine the number of colony-forming units (CFU/mL). The results were compared by analysis of variance and Tukey test (p < 0.05). The two strains studied were sensitive to PDT (L + P+), with a log reduction of 0.49 for serotype A and of 2.34 for serotype B. Laser application alone only reduced serotype B cells (0.53 log), and the use of the photosensitizer alone had no effect on the strains tested. It can be concluded that in vitro biofilms of C. albicans serotype B were more sensitive to PDT.


Similar content being viewed by others
References
Williams DW, Kuriyama T, Silva S, Malic S, Lewis MA (2011) Candida biofilms and oral candidosis: treatment and prevention. Periodontol 55:250–265. doi:10.1111/j.1600-0757.2009.00338.x
Li L, Redding S, Dongari-Bagtzoglou A (2007) Candida glabrata, an emerging oral opportunistic pathogen. J Dent Res 86:204–215. doi:10.1177/154405910708600304
Martínez JP, Gil ML, López-Ribot JL, Chaffin WL (1998) Serologic response to cell wall mannoproteins and proteins of Candida albicans. Clin Microbiol Rev 11(1):121–41
Mille C, Janbon G, Delplace F, Ibata-Ombetta S, Gaillardin C, Strecker G et al (2004) Inactivation of CaMIT1 inhibits Candida albicans phospholipomannan beta-mannosylation, reduces virulence, and alters cell wall protein beta-mannosylation. J Biol Chem 12(279):47952–60. doi:10.1074/jbc.M405534200
Shibata N, Kobayashi H, Okawa Y, Suzuki S (2003) Existence of novel b-1,2 linkage-containing side chain in the mannan of Candida lusitaniae, antigenically related to Candida albicans. Eur J Biochem 270:2565–2575. doi:10.1046/j.1432-1033.2003.03622.x
Shibata N, Suzuki A, Kobayashi H, Okawa Y (2007) Chemical structure of the cell wall of C. albicans serotype A and its difference in yeast and hyphal form. Biochem J 404:365–372. doi:10.1042/BJ20070081
Hazen BW, Hazen KC (1988) Dynamic expression of cell surface hydrophobicity during initial yeast cell growth and before germ tube formation of Candida albicans. Infect Immun 56:2521–2525
Hazen KC, Hazen BW (1987) Temperature-modulated physiological characteristics of Candida albicans. Microbiol Immunol Microbiol Immunol 31:497–508
Auger P, Dumas C, Joly J (1979) A study of 666 strains of Candida albicans: correlation between serotype and susceptibility to 5-fluorocytosine. J Infect Dis 139:590–4. doi:10.1093/infdis/139.5.590
Martin MV, Lamb DJ (1982) Frequency of Candida albicans serotypes in patients with denture induced stomatitis and in normal denture wearers. J Clin Pathol 35:888–91. doi:10.1136/jcp.35.8.888
Brawner DL, Anderson GL, Yuen KY (1992) Serotype prevalence of Candida albicans from blood culture isolates. J Clin Microbiol 30:149–53
Suryawanshi H, Ganvir SM, Hazarey VK, Wanjare VS (2012) Oropharyngeal candidosis relative frequency in radiotherapy patient for head and neck cancer. J Oral Maxillofac Pathol 16:31–7. doi:10.4103/0973-029X.92970
Hansclever HF, Mitchell WO (1961) Antigenic studies of Candida. III. Comparative pathogenicity of Candida albicans group A, group B, and Candida stellatoidea. J Bacteriol 82:578–81
Junqueira JC, Jorge AO, Barbosa JO, Rossoni RD, Vilela SF, Costa AC et al (2012) Photodynamic inactivation of biofilms formed by Candida spp., Trichosporon mucoides, and Kodamaea ohmeri by cationic nanoemulsion of zinc 2,9,16,23-tetrakis(phenylthio)-29H, 31H-phthalocyanine (ZnPc). Lasers Med Sci 27:1205–12. doi:10.1007/s10103-012-1050-2
Fuchs BB, Tegos GP, Hamblin MR, Mylonakis E (2007) Susceptibility of Cryptococcus neoformans to photodynamic inactivation is associated with cell wall integrity. Antimicrob Agents Chemother 51:2929–36. doi:10.1128/AAC.00121-07
Kharkwal GB, Sharma SK, Huang YY, Dai T, Michael R, Hamblin MR (2011) Photodynamic therapy for infections: clinical applications. Lasers Surg Med 43:755–767. doi:10.1002/lsm.21080
Bertoloni G, Rossi F, Valduga G, Jori G, Ali H, van Lier JE (1992) Photosensitizing activity of water- and lipid-soluble phthalocyanines on prokaryotic and eukaryotic microbial cells. Microbios 71:33–46
Teichert MC, Jones JW, Usacheva MN, Biel MA (2002) Treatment of oral candidiasis with methylene blue-mediated photodynamic therapy in an immunodeficient murine model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93(2):155–60. doi:10.1067/moe.2002.120051
Konopka K, Goslinski T (2007) Photodynamic therapy in dentistry. J Dent Res 86(8):694–707. doi:10.1177/154405910708600803
Souza SC, Junqueira JC, Balducci I, Ito-Koga CY, Munin E, Jorge AOC (2006) Photosensitization of different Candida species by low power laser light. Photochem Photobiol B Biol 83:34–38. doi:10.1016/j.jphotobiol.2005.12.002
Jin Y, Samaranayake LP, Samaranayake Y, Yip HK (2004) Biofilm formation of Candida albicans is variably affected by saliva and dietary sugars. Arch Oral Biol 49(10):789–98. doi:10.1016/j.archoralbio.2004.04.011
Giroldo LM, Felipe MP, Oliveira MA, Munin E, Alves LP, Costa MS (2009) Photodynamic antimicrobial chemotherapy (PACT) with methylene blue increases membrane permeability in Candida albicans. Lasers Med Sci 24:109–12. doi:10.1007/s10103-007-0530-2
Souza RC, Junqueira JC, Rossoni RD, Pereira CA, Munin E, Jorge AO (2010) Comparison of the photodynamic fungicidal efficacy of methylene blue, toluidine blue, malachite green and low-power laser irradiation alone against Candida albicans. Lasers Med Sci 25:385–9. doi:10.1007/s10103-009-0706-z
Boyce JM, Pittet D (2002) Guideline for hand hygiene in health-care settings: recommendations of the healthcare infection control practices advisory committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task force. Infect Control Hosp Epidemiol 23:S3–40. doi:10.1086/50316
Gonzales FP, Felgenträger A, Bäumler W, Maisch T (2013) Fungicidal photodynamic effect of a twofold positively charged porphyrin against Candida albicans planktonic cells and biofilms. Future Microbiol 8:785–97. doi:10.2217/fmb.13.44
Pereira CA, Romeiro RL, Costa ACBP, Machado AKS, Junqueira JC, Jorge AO (2011) Susceptibility of Candida albicans, Staphylococcus aureus, and Streptococcus mutans biofilms to photodynamic inactivation: an in vitro study. Lasers Med Sci 26:341–8. doi:10.1007/s10103-010-0852-3
Schneider M, Kirfel G, Berthold M, Frentzen M, Krause F, Braun A (2012) The impact of antimicrobial photodynamic therapy in an artificial biofilm model. Lasers Med Sci 27:615–20. doi:10.1007/s10103-011-0998-7
Vilela SF, Junqueira JC, Barbosa JO, Majewski M, Munin E, Jorge AO (2012) Photodynamic inactivation of Staphylococcus aureus and Escherichia coli biofilms by malachite green and phenothiazine dyes: an in vitro study. Arch Oral Biol 57:704–10. doi:10.1016/j.archoralbio.2011.12.002
Nobile CJ, Mitchell AP (2006) Genetics and genomics of Candida albicans biofilm formation. Cell Microbiol 8:1382–91. doi:10.1111/j.1462-5822.2006.00761.x
Ramage G, Walle KV, Wickes BL, Lopes-Ribot JL (2001) Biofilm formation by Candida dubliniensis. J Clin Microbiol 39:3234–40. doi:10.1128/JCM.39.9.3234-3240.2001
Andrade MC, Ribeiro AP, Dovigo LN, Brunetti IL, Giampaolo ET, Bagnato VS, et al (2012) Effect of different pre-irradiation times on curcumin-mediated photodynamic therapy against planktonic cultures and biofilms of Candida spp. Arch Oral Biol S0003-9969(12)00372-X. doi: 10.1016/j.archoralbio.2012.10.011
Sant’Ana Pde L, Milan EP, Martinez R, Queiroz-Telles F, Ferreira MS, Alcântara AP et al (2002) Multicenter Brazilian study of oral Candida species isolated from AIDS patients. Mem Inst Oswaldo Cruz 97:253–7. doi:10.1590/S0074-02762002000200019
Velegraki A (1995) In vitro susceptibility to itraconazole and fluconazole of switch phenotypes of Candida albicans serotypes A and B isolated from immunocompromised hosts. J Med Vet Mycol 33:83–85. doi:10.1080/02681219580000181
Brawner DL, Cutler JE (1989) Oral Candida albicans isolates from nonhospitalized normal carriers, immunocompetent hospitalized patients, and immunocompromised patients with or without acquired immunodeficiency syndrome. J Clin Microbiol 27:1335–1341
Hazen KC, Mandell G, Coleman E, Wu G (2000) Influence of fluconazole at subinhibitory concentrations on cell surface hydrophobicity and phagocytosis of Candida albicans. FEMS Microbiol Lett 183:89–94
Gutknecht N, Moritz A, Conrads G, Sievert T, Lampert F (1996) Bactericidal effect of the Nd:YAG laser in vitro root canals. J Clin Laser Med Surg 14:77–80
Gouw-Soares S, Gutknecht N, Conrads G, Lampert F, Matson E, Eduardo CP (2000) The bactericidal effect of Ho:Yag laser irradiation within contaminated root dentinal samples. J Clin Laser Med Surg 18:81–87. doi:10.1089/clm.2000.18.81
Nussbaum EL, Lilge L, Mazzulli T (2002) Effects of 810 nm laser irradiation on in vitro growth of bacteria: comparison of continuous wave and frequency modulated light. Lasers Surg Med 31:343–351. doi:10.1002/lsm.10121
Nussbaum EL, Lilge L, Mazzulli T (2002) Effects of 630-, 660-,810-, and 905-nm laser irradiation delivering radiant exposure of 1-50 J/cm2 on three species of bacteria in vitro. J Clin Laser Med Surg 20:325–33
Maver-Biscanin M, Mravak-Stipetic M, Jerolimov V (2005) Effect of low-level laser therapy on Candida albicans growth in patients with denture stomatitis. Photomed Laser Surg 23:328–332. doi:10.1089/pho.2005.23.328
Basso FG, Oliveira CF, Fontana A, Kurachi C, Bagnato VS, Spolidório DM et al (2011) In vitro effect of low-level laser therapy on typical oral microbial biofilms. Braz Dent J 22:502–10. doi:10.1590/S0103-64402011000600011
Lambrechts SA, Aalders MC, Van Marle J (2005) Mechanistic study of the photodynamic inactivation of Candida albicans by a cationic porphyrin. Antimicrob Agents Chemother 49:2026–2034. doi:10.1128/AAC.49.5.2026-2034.2005
Wainwright M, Crossley KB (2002) Methylene blue—a therapeutic dye for all seasons? J Chemother 14:431–43. doi:10.1179/joc.2002.14.5.431
Calzavara-Pinton PG, Venturini M, Sala R (2005) A comprehensive overview of photodynamic therapy in the treatment of superficial fungal infections of the skin. J Photochem Photobiol B 78:1–6. doi:10.1016/j.jphotobiol.2004.06.006
Paz-Cristobal MP, Royo D, Rezusta A, Andrés-Ciriano E, Alejandre MC, Meis JF et al (2014) Photodynamic fungicidal efficacy of hypericin and dimethyl methylene blue against azole-resistant Candida albicans strains. Mycoses 57:35–42. doi:10.1111/myc.12099
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossoni, R.D., Barbosa, J.O., de Oliveira, F.E. et al. Biofilms of Candida albicans serotypes A and B differ in their sensitivity to photodynamic therapy. Lasers Med Sci 29, 1679–1684 (2014). https://doi.org/10.1007/s10103-014-1570-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1570-z