Abstract
The primary objective of this meta-analysis was to estimate the prevalence of adult community-acquired pneumonia (CAP) caused by Streptococcus pneumoniae in Europe, adjusted for possible independent covariates. Two reviewers conducted a systematic literature search using PubMed on English-language articles that involved human subjects with CAP during the period from January 1990 to November 2011 across European countries. A mixed-effects meta-regression model was developed and populated with 24,410 patients obtained from 77 articles that met the inclusion criteria. The model showed that the observed prevalence of S. pneumoniae in CAP significantly varies between European regions, even after adjusting for explanatory covariates, including patient characteristics, diagnostic tests, antibiotic resistance, and health-care setting. The probability of detecting S. pneumoniae was substantially higher in studies that performed more frequently a diagnostic polymerase chain reaction assay compared to all the other diagnostic tests included. Furthermore, S. pneumoniae was more likely to be confirmed as the cause of a CAP in studies with intensive care unit patients as compared to those with hospital- or community-treated patients. This study provides estimates of the average observed prevalence of S. pneumoniae, which could be used for projecting the health and economic benefits of pneumococcal immunization.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP) is a common disease, with an annual incidence of 5 to 11 cases per thousand adults in Europe and Northern America [1]. Streptococcus pneumoniae is generally accepted to be the most common cause of CAP [2–4]. There is, however, no consensus regarding the prevalence of S. pneumoniae in CAP, and estimates vary from 5 to 60 % between different studies [2–4]. This may either reflect a true difference or, rather, a difference in confirmation rates.
Two earlier reviews, which focused on the causative agents of CAP, suggested that the frequency of S. pneumoniae differs between countries [3] and health-care settings [4]. However, large variations between studies within the same setting and country were observed, suggesting that these differences could be more related to the study methodology than to real differences [4]. Another factor which might have impacted the findings of the previous reviews is that the investigators also included studies in which radiographic confirmation of pneumonia was not an inclusion criterion. As a consequence, part of the study patients can be expected to have had respiratory tract infections other than pneumonia, or entirely other conditions, and the respiratory pathogens detected in those cases might not be relevant to describe the relative contribution of S. pneumoniae in CAP [5].
It is important to have a reliable estimate of the share of S. pneumoniae in the total burden of CAP, especially now that the results of a clinical trial estimating the efficacy of the 13-valent conjugated pneumococcal vaccine (PCV13) in the elderly are pending and the country-specific health and economic impact of this vaccine will largely depend on the share of S. pneumoniae in CAP [6, 7].
The primary objective of this meta-analysis is to estimate the average etiological fraction of S. pneumoniae in CAP while controlling for potential sources of heterogeneity attributed to regional, health-care settings, and other differences.
Methods
Search strategy and selection criteria
We used PubMed (http://www.pubmed.com) to search for original study reports during the period between January 1990 and November 2011 on the etiology of CAP among adults using the following search terms: “Pneumonia” [MAJR] AND (“etiology” [Subheading] OR “epidemiology” [Subheading]) AND (“Pneumonia, Bacterial” [MH] OR “Pneumonia, Viral” [MH] OR “microbiology” [Subheading] OR “virology” [Subheading] OR “Streptococcus pneumoniae” [MH]) AND (“Adult” [MH] OR “aged” [MH]) AND (“Journal article” [PT] NOT “meta-analysis” [PT] NOT “review” [PT] NOT “guideline” [PT]). We limited the articles to the English language. To ensure that articles actually dealt with the most accurate diagnostic definition of CAP, studies in which the CAP diagnosis was not confirmed with a new or increased infiltrate on a chest radiograph were excluded. Furthermore, we excluded: (1) case reports, editorials, reviews, and letters without original data; (2) studies which focused primarily on pneumonia related to sources other than the community; (3) articles that included only specific patient groups, such as patients with chronic obstructive pulmonary disease (COPD); (4) studies performed during the 2009 influenza pandemic; (5) clinical trials; and (6) studies which did not report the fraction of CAP being caused by S. pneumoniae.
After applying these inclusion and exclusion criteria, the titles of all potentially eligible articles were independently reviewed by two investigators (M.H.R. and E.H.). Articles were excluded from further review only if both investigators agreed on one or more reasons for exclusion. If a study was not excluded on the basis of the title, the study abstract was reviewed independently by both investigators. Subsequently, all articles judged to meet the inclusion criteria based on the reviewed abstract were retrieved for further evaluations. After reviewing the entire text of the retrieved papers, only those that met all inclusion criteria were included in the analysis and the relevant data were extracted (see below).
Data extraction
Two reviewers independently extracted the total number of CAP episodes and the number of CAP episodes in which S. pneumoniae could be detected. A CAP episode was assumed to be caused by S. pneumoniae if it was detected in a normally sterile site, in the nasopharynx, or in sputum. We also recorded the type of diagnostic tools applied and distinguished them between culture, serological, or polymerase chain reaction (PCR) tests, or more invasive sampling methods. Culture tests were sub-divided into those performed on either sputum or blood. Serological tests were separated into tests performed on urine and those performed on blood and sputum. More invasive sampling methods included trans-thoracic needle aspirations and bronchoscopic techniques.
Further, the following study-specific data were extracted: health-care setting, country and time period, age (mean or median if the mean is not reported), gender distribution, percentage of included patients with COPD and patients with severe immunosuppression (including patients with organ transplants, human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), chemotherapy, and chronic corticosteroids use of >20 mg/day). The health-care setting was divided into three distinctive groups: (1) cases managed in primary care; (2) cases admitted to hospital; and (3) cases admitted to the intensive care unit (ICU). Four different geographical regions were defined based on the United Nations geoscheme (North, East, South, and West) [8].
Also, country-specific antibiotic use and resistance of S. pneumoniae to antibiotics might have an impact on the observed prevalence of the respiratory agents [9].
To take antibiotic use into account, we used the defined daily dose of outpatient antibiotics (antimicrobials for systemic use, ATC Group J01) per 1,000 inhabitants as reported by Muller et al. for the year 2002 [10]. Since only reimbursement data were available for Spain, we corrected the number of doses upwards to correct for the fact that over-the-counter antibiotic use in Spain stands at around 30 % [9].
The S. pneumoniae-specific level of antibiotic resistance was based on the percentage of penicillin non-susceptibility using 2010 data of the antimicrobial resistance surveillance in Europe [11] and other sources for Switzerland [12] and Greece [13]. Although shifts in the use of antibiotics and related resistance might occur, it has been shown that antibiotic use and resistance in the selected countries remained quite stable over time [9–11, 14].
Statistical methods
In order to synthesize the collected evidence, we used a meta-regression model framework for binomial outcomes [15]. Given the large expected true variation of prevalence between studies, we decided to use a mixed-effects instead of a fixed-effects meta-regression framework [16]. In this specification, we assumed that the covariate-adjusted log odds of an S. pneumoniae-induced CAP is not constant but varies randomly across studies. We further assumed that the additional, study-specific random effects follow a normal distribution with zero mean and variance \( \sigma_{\mathrm{Study}}^2 . \) It was also assumed that the measure of association between the log odds of an S. pneumoniae-induced CAP and countries is random and normally distributed with mean zero and variance \( \sigma_{\mathrm{Country}}^2 . \) Additionally to these random effects, the model was corrected for a number of study- and country-specific covariates which were incorporated as fixed effects. From the full set of covariates, we sub-selected those that significantly improved the fit of the model. We fitted a variety of models with different covariates included and compared their goodness of fit using the Akaike information criterion (AIC) in order to arrive at the final set of covariates [17, 18].
Missing values in the covariates used were handled through multiple imputation [19, 20]. We created 25 imputed datasets, in each of which every missing value was replaced with a plausible value estimated through a regression model. Next, the meta-regression framework described above was applied for every dataset. The results were subsequently synthesized for statistical inference. All statistical analyses were implemented using the statistical software R (version 2.13.2) [21]. We additionally used the “mi”, “lme4”, and “meta” R packages for the implementation of multiple imputation, the estimation of the mixed-effects meta-regressions, and the visualization of the results, respectively [20, 22].
Results
Search results
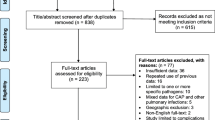
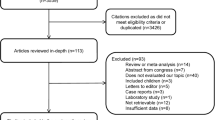
Of the 3,738 original citations, we excluded 3,290 (88 %) based on a review of the titles (Fig. 1). Of the remaining 448 selected studies, 277 were excluded after reviewing the abstract. After reviewing the entire text of the remaining 171 studies, 73 met eligibility criteria. In addition to the 73 studies included by the initial search term, four more were identified by the scanning of references and subsequently added, resulting in a total of 77 included studies [5, 23–98]. Several studies reported data separately for health-care settings. These studies were, therefore, split into setting-specific “sub-studies” in this analysis.
Study characteristics
The characteristics of the 77 selected studies are presented in Table 1. Of all (sub-)studies included, the majority reported cases admitted to hospital (n = 60), 17 were available for cases admitted to the ICU, and 14 for cases managed in the primary care. A total of 24,410 patients were included, with an average age of 62.1 years, with 62.3 % being male. Most of the studies originated from Southern Europe, with Spain being the most frequently represented country. No studies were found for Eastern Europe. In Fig. 2, the crude proportion of S. pneumonia per country is presented.
The country-specific, crude proportion of Streptococcus pneumoniae as a causative agent for community-acquired pneumonia (CAP). Numbers of episodes per country: Germany (1,783), Spain (12,804), UK (605), Netherlands (1,318), France (2,480), Italy (897), Sweden (892), Finland (688), Slovenia (325), Norway (19), Denmark (545), Estonia (439), Switzerland (1,464), Greece (88), Portugal (76)
S. pneumoniae
We identified 24,423 CAP episodes in 24,410 patients (patients could have more than one episode), of which 4,714 (19.3 %) were attributed to S. pneumoniae. Figure 3 presents the unadjusted, study-specific proportions of S. pneumoniae as the causative agent for CAP, together with the proportions’ confidence intervals (CIs).
Mixed-effects meta-regression
The results of the final model, in which country and study were estimated as random-effects parameters and the rest of the covariates as fixed-effects parameters, are presented in Table 2. This model assumes as baseline a study with average proportions of blood cultures, urine serology, blood or sputum serology, and PCR tests. Additionally, this baseline study is assumed to originate from a Northern European country with average antibiotic resistance and with CAP episodes that were managed in primary care. Hence, the estimated odds of an S. pneumoniae-caused CAP for a study with baseline characteristics was 0.176, which corresponds to a probability of 0.15. The model also showed that, in studies in which the percentage of blood cultures, urine serology, blood or sputum serology, or PCR tests increased, the likelihood of detecting S. pneumoniae also significantly increased, with the highest increase observed for PCR tests (odds ratio 2.49; 95 % CI: 1.39–4.46).
Compared to studies with CAP episodes managed in primary care, the odds of S. pneumoniae being the cause of a CAP was 1.45 (95 % CI: 1.19–1.77) times higher in studies with episodes treated in the hospital and 2.33 (95 % CI: 1.80–3.02) times higher in the ICU. The odds of detecting S. pneumoniae as the cause of CAP in studies from Western and Southern Europe were almost two and three times smaller, respectively, compared to studies conducted in Northern Europe, where S. pneumoniae was the most frequently observed, independently of the percentage of diagnostic testing [Western Europe: 0.57 (95 % CI: 0.32–1.00); Southern Europe: 0.40 (95 % CI: 0.2–0.80)]. Illustratively, a study with baseline characteristics but originating from Southern Europe is expected to identify S. pneumoniae as the causative agent in 6.5 % of the CAP episodes (since \( {{{\left( {0.176*0.397} \right)}} \left/ {{\left( {1+0.176*0.397} \right)}} \right.}=0.065 \)).
The estimate of the variance for the study- and country-specific random effects indicated that there was significant heterogeneity among the estimates that was not captured through the fixed-effects covariates. The inclusion of both study- and country- specific random effects significantly improved the goodness-of-fit of the model.
Sputum culture and invasive detection techniques did not have a significant impact on the model or contributed to a better fit of the model to the study data, according to the AIC. Antibiotic resistance also did not significantly affect the probability to detect S. pneumoniae after inclusion of the random-effects term for per-country variations. However, antibiotic resistance was deemed as being useful for the fit of the model and was, therefore, included in the analysis.
Discussion
In this analysis, we showed that the observed prevalence of S. pneumoniae in adult CAP significantly varies between studies conducted in different European regions, even after correcting for effect modifiers, including diagnostic tests used, antibiotic resistance, and health-care setting. The probability of detecting S. pneumoniae was also substantially higher in studies that performed more frequently a diagnostic PCR assay compared to all the other diagnostic tests included. Furthermore, S. pneumoniae was observed less frequently in studies with CAP cases treated in the community as compared to those with cases treated in the hospital or in the ICU.
In contrast to earlier review studies on this topic, we approached the analysis of the observed frequency of S. pneumoniae among pneumonia cases through a mixed-effects meta-regression framework [3, 4]. In this respect, we not only accounted for the influence of various covariates on the observed prevalence of S. pneumoniae, such as the health-care setting, diagnostic tests used, and antibiotic resistance, but we also corrected for other study- and country-specific unobserved parameters that might also have an impact on this share. This correction revealed that significant unobserved variation exists among countries, as well as across studies, regarding the observed share of S. pneumoniae in CAP.
The finding that this share differs across health-care settings was also noted previously by Woodhead [4], although this was accompanied with the remark that individual studies showed a wide variety in the frequency of detecting S. pneumoniae. Our findings agreed with those observed by Woodhead, but through the use of a meta-regression model and the inclusion of more recent studies, we were able to confirm significant differences that were independent of other covariates.
One of the limitations of the previous reviews was that they did not exclude studies in which a radiographic confirmation of pneumonia was not an inclusion criterion. Without a chest radiograph, a CAP diagnosis cannot be made with certainty [5]. Similar clinical signs and symptoms can also be caused by non-infectious diseases, such as congestive heart failure or atelectasis [27]. Therefore, and because the interpretation of clinical assessments are prone to inter-observer variability, we only included those studies in which this was an inclusion criterion.
Our meta-analysis showed that, in studies in which the percentage of invasive techniques or sputum culture increased, the likelihood of detecting S. pneumoniae did not significantly increase. This finding for invasive testing might be counterintuitive, but can be attributed to the underreporting of the proportion of patients tested with this invasive method. In particular, almost all included studies report that invasive tests were performed, but the majority did not report the proportion of the patients tested. In most studies, the use of invasive techniques is likely to be limited to a few patients, as invasive sampling methods for lower respiratory secretions are impractical. This limited the accuracy of the estimate of the impact of invasive tests on detecting S. pneumoniae. A sub-analysis in the studies that reported the fraction of invasive testing revealed that the percentage of invasive tests performed had a significant positive impact on the study’s detected fraction of S. pneumoniae in CAP (data not shown).
Of course, our study also has some limitations, which can be divided into those related to health-care setting, population, epidemiological, study methodological, and model-related factors [4]. Our model showed that S. pneumoniae was more likely to be prevalent in CAP cases treated in the ICU as compared to those treated in the hospital or in the community. We do, however, note that admission criteria for hospitalization or ICU admission might differ between hospitals and countries and may not always reflect severity. For example, in Spain, many patients seek medical care directly from the emergency service of the hospital rather than after a visit to a primary care physician [65]. Nevertheless, some of the country variation on the detection of S. pneumoniae is expected to have been captured through the country-specific random-effects parameter.
Secondly, factors related to the population, such as antibiotic therapy, vaccination status, immunosuppression, and comorbid conditions, might impact the share of S. pneumoniae detected. We tried to obtain as much information on the included studies as possible in order to be able to correct for these factors. For example, we obtained information on the proportion of immunosuppressed patients and patients suffering from COPD. However, the fit of the model was best when these factors were excluded. This might be explained by the fact that different definitions of ‘immunocompromised’ among studies were used or that specific data were just not reported. Additionally, the country-specific random-effects term used in the model might have corrected for enough across-country variation, constituting these variables as redundant. Furthermore, to minimize heterogeneity between studies, we decided to exclude clinical trials, as patients enrolled in these studies differ from those encountered in daily clinical practice. Considering the long time span of studies included into the model, we were unable to include PPV23 or influenza vaccination status, as country-specific vaccination coverage over time are not abundantly available. The impact of PPV23 vaccination is probably small, as the uptake, the efficacy, and the duration of protection of PPV23 are limited [99, 100]. Although the influenza vaccine does not protect directly against pneumococcal pneumonia, viral infections may pave the way for pneumococcal infections [101]. We based the level of antibiotic resistance on recent antimicrobial resistance surveillance data [11]. Resistance levels may change over time, but we note that the resistance patterns of the most recent EARSS report [11] are very similar to the earliest EARSS report using data from 1999 to 2001 [14].
Thirdly, epidemiological factors may change the share of S. pneumoniae cases. For example, the time of year might impact the frequency of S. pneumoniae detected. Most of the studies included in our analysis had a time span of over a year, which might have been long enough to capture the short-term seasonal effects.
Fourthly, methodological factors such as comprehensiveness of sample collection and microbiological investigation performed are important [4]. We explicitly took this into account by correcting for both the type of microbiological investigation performed, as well as for the frequency at which these tests were performed. As previously noted by Woodhead, some studies did not explicitly state the percentages of actually performed tests [4].
Finally, a limitation of our analysis is the inability to accurately estimate the true prevalence of S. pneumoniae among CAP cases. The main reason for this is that the applied tests cannot detect the true fraction of S. pneumoniae among the CAP cases, and, hence, the S. pneumoniae prevalence, due to their limited sensitivity and specificity. It is expected that there will be an undetected fraction of S. pneumoniae due to false-negative tests, i.e., low sensitivity. However, this undetected fraction might be partly compensated by the false-positive tests, i.e., low specificity.
Recently, the European Commission extended the indication of PCV13 to adults aged 50 years and older to prevent invasive pneumococcal disease caused by S. pneumoniae. While there is currently no indication for non-invasive pneumonia, clinical trial data will become available soon [6]. Recent cost-effectiveness studies have shown that, next to the vaccine efficacy, the proportion of non-bacteremic pneumonia due to S. pneumoniae is one of the key determinants of cost-effectiveness [7, 102]. Our current study might, therefore, support the decision-making process of the introduction of PCV13 [7, 102].
In conclusion, our study provides estimates of the average observed prevalence of S. pneumoniae, which could be used for projecting the health and economic benefits of pneumococcal immunization.
References
Lim WS, Baudouin SV, George RC et al (2009) BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 64(Suppl 3):iii1–iii55
Janssens JP, Krause KH (2004) Pneumonia in the very old. Lancet Infect Dis 4(2):112–124
Welte T, Torres A, Nathwani D (2012) Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax 67:71–79
Woodhead M (2002) Community-acquired pneumonia in Europe: causative pathogens and resistance patterns. Eur Respir J Suppl 36:20s–27s
Holm A, Nexoe J, Bistrup LA et al (2007) Aetiology and prediction of pneumonia in lower respiratory tract infection in primary care. Br J Gen Pract 57(540):547–554
Hak E, Grobbee DE, Sanders EA et al (2008) Rationale and design of CAPITA: a RCT of 13-valent conjugated pneumococcal vaccine efficacy among older adults. Neth J Med 66(9):378–383
Rozenbaum MH, Hak E, van der Werf TS, Postma MJ (2010) Results of a cohort model analysis of the cost-effectiveness of routine immunization with 13-valent pneumococcal conjugate vaccine of those aged > or =65 years in the Netherlands. Clin Ther 32(8):1517–1532
United Nations Statistics Division (2008) Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings. Available online at: http://millenniumindicators.un.org/unsd/methods/m49/m49regin.htm
Goossens H, Ferech M, Vander Stichele R, Elseviers M; ESAC Project Group (2005) Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365(9459):579–587
Muller A, Coenen S, Monnet DL, Goossens H; ESAC Project Group (2007) European Surveillance of Antimicrobial Consumption (ESAC): outpatient antibiotic use in Europe, 1998–2005. Euro Surveill 12(10):E071011.1
European Centre for Disease Prevention and Control (ECDC) (2011) Antimicrobial resistance surveillance in Europe 2010. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC
Schweizerisches Zentrum für Antibiotikaresistenzen (2011) Available online at: http://www.anresis.ch/de/index.html#javascript:loadContent%28%27#content-data%27,%27include/resistancedataselection.html%27%29. Accessed 24Nov 2011
Poulakou G, Katsarolis I, Matthaiopoulou I et al (2007) Nationwide surveillance of Streptococcus pneumoniae in Greece: patterns of resistance and serotype epidemiology. Int J Antimicrob Agents 30(1):87–92
European Centre for Disease Prevention and Control (ECDC) (2001) EARSS annual report 2001. Stockholm: ECDC
Higgins JP, Thompson SG (2004) Controlling the risk of spurious findings from meta-regression. Stat Med 23(11):1663–1682
Thompson SG, Higgins JP (2002) How should meta-regression analyses be undertaken and interpreted? Stat Med 21(11):1559–1573
Bolker BM, Brooks ME, Clark CJ et al (2009) Generalized linear mixed models: a practical guide for ecology and evolution. Trends Ecol Evol 24(3):127–135
Akaike H (1974) A new look at the statistical model identification. IEEE Trans Automat Contr 19(6):716–723
Hox JJ, Roberts JK (eds) (2011) Handbook of advanced multilevel analysis. Routledge, New York, p 173
Su YS, Gelman A, Hill J, Yajima M (2011) Multiple imputation with diagnostics (mi) in R: opening windows into the black box. J Stat Softw 45(2):1–31
Development Core Team (2005) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0. Home page at: http://www.R-project.org/
Bates D, Maechler M, Bolker B (2011) lme4: linear mixed-effects models using S4 classes. R package version 0.999375-42. http://CRAN.R-project.org/package=lme4
Ewig S, Schlochtermeier M, Göke N, Niederman MS (2002) Applying sputum as a diagnostic tool in pneumonia: limited yield, minimal impact on treatment decisions. Chest 121(5):1486–1492
Marques MR, Nunes A, Sousa C, Moura F, Gouveia J, Ramos A (2010) Community-acquired pneumonia in an intensive care unit. Rev Port Pneumol 16(2):223–235
Manali E, Papadopoulos A, Tsiodras S, Polychronopoulos V, Giamarellou H, Kanellakopoulou K (2008) The impact on community acquired pneumonia empirical therapy of diagnostic bronchoscopic techniques. Scand J Infect Dis 40(4):286–292
Müller F, Christ-Crain M, Bregenzer T et al (2010) Procalcitonin levels predict bacteremia in patients with community-acquired pneumonia: a prospective cohort trial. Chest 138(1):121–129
Müller B, Harbarth S, Stolz D et al (2007) Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis 7:10
Janssens JP, Gauthey L, Herrmann F, Tkatch L, Michel JP (1996) Community-acquired pneumonia in older patients. J Am Geriatr Soc 44(5):539–544
Genné D, Siegrist HH, Lienhard R (2006) Enhancing the etiologic diagnosis of community-acquired pneumonia in adults using the urinary antigen assay (Binax NOW). Int J Infect Dis 10(2):124–128
Kirk O, Glenthøj J, Dragsted UB et al (2001) Penicillin as empirical therapy for patients hospitalised with community acquired pneumonia at a Danish hospital. Dan Med Bull 48(2):84–88
Ostergaard L, Andersen PL (1993) Etiology of community-acquired pneumonia. Evaluation by transtracheal aspiration, blood culture, or serology. Chest 104(5):1400–1407
Farina C, Arosio M, Vailati F, Moioli F, Goglio A (2002) Urinary detection of Streptococcus pneumoniae antigen for diagnosis of pneumonia. New Microbiol 25(2):259–263
Guglielmo L, Leone R (1997) Aetiology and therapy of community-acquired pneumonia: a hospital study in northern Italy. Veneto Pneumonia Research Group. Eur J Clin Pharmacol 51(6):437–443
Michetti G, Pugliese C, Bamberga M et al (1995) Community-acquired pneumonia: is there difference in etiology between hospitalized and out-patients? Minerva Med 86(9):341–351
Burman LA, Trollfors B, Andersson B et al (1991) Diagnosis of pneumonia by cultures, bacterial and viral antigen detection tests, and serology with special reference to antibodies against pneumococcal antigens. J Infect Dis 163:1087–1093
Johansson N, Kalin M, Tiveljung-Lindell A, Giske CG, Hedlund J (2010) Etiology of community-acquired pneumonia: increased microbiological yield with new diagnostic methods. Clin Infect Dis 50(2):202–209
Ortqvist A, Hedlund J, Grillner L et al (1990) Aetiology, outcome and prognostic factors in community-acquired pneumonia requiring hospitalization. Eur Respir J 3:1105–1113
Strålin K, Olcén P, Törnqvist E, Holmberg H (2010) Definite, probable, and possible bacterial aetiologies of community-acquired pneumonia at different CRB-65 scores. Scand J Infect Dis 42(6–7):426–434
Hohenthal U, Vainionpää R, Meurman O et al (2008) Aetiological diagnosis of community acquired pneumonia: utility of rapid microbiological methods with respect to disease severity. Scand J Infect Dis 40(2):131–138
Jokinen C, Heiskanen L, Juvonen H et al (2001) Microbial etiology of community-acquired pneumonia in the adult population of 4 municipalities in eastern Finland. Clin Infect Dis 32(8):1141–1154
Beović B, Bonac B, Kese D et al (2003) Aetiology and clinical presentation of mild community-acquired bacterial pneumonia. Eur J Clin Microbiol Infect Dis 22(10):584–591
Socan M, Marinic-Fiser N, Kraigher A, Kotnik A, Logar M (1999) Microbial aetiology of community-acquired pneumonia in hospitalised patients. Eur J Clin Microbiol Infect Dis 18:777–782
Melbye H, Berdal BP, Straume B, Russell H, Vorland L, Thacker WL (1992) Pneumonia—a clinical or radiographic diagnosis? Etiology and clinical features of lower respiratory tract infection in adults in general practice. Scand J Infect Dis 24(5):647–655
Leesik H, Ani U, Juhani A, Altraja A (2006) Microbial pathogens of adult community-acquired pneumonia in Southern Estonia. Medicina (Kaunas) 42(5):384–394
Fantin B, Aubert JP, Unger P, Lecoeur H, Carbon C (2001) Clinical evaluation of the management of community-acquired pneumonia by general practitioners in France. Chest 120(1):185–192
Georges H, Leroy O, Vandenbussche C et al (1999) Epidemiological features and prognosis of severe community-acquired pneumococcal pneumonia. Intensive Care Med 25(2):198–206
Leroy O, Georges H, Beuscart C et al (1996) Severe community-acquired pneumonia in ICUs: prospective validation of a prognostic score. Intensive Care Med 22(12):1307–1314
Moine P, Vercken JB, Chevret S, Chastang C, Gajdos P (1994) Severe community-acquired pneumonia. Etiology, epidemiology, and prognosis factors. French Study Group for Community-Acquired Pneumonia in the Intensive Care Unit. Chest 105(5):1487–1495
Paganin F, Lilienthal F, Bourdin A et al (2004) Severe community-acquired pneumonia: assessment of microbial aetiology as mortality factor. Eur Respir J 24(5):779–785
Renaud B, Coma E, Labarere J et al (2007) Routine use of the Pneumonia Severity Index for guiding the site-of-treatment decision of patients with pneumonia in the emergency department: a multicenter, prospective, observational, controlled cohort study. Clin Infect Dis 44(1):41–49
Laurichesse H, Sotto A, Bonnet E et al (2001) Pre- and in-hospital management of community-acquired pneumonia in southern France, 1998–99. Eur J Clin Microbiol Infect Dis 20(11):770–778
Blasi F, Cosentini R, Raccanelli R et al (1995) Emerging pathogens of community-acquired pneumonia: a two-year prospective study. J Chemother 7(Suppl 4):115–116
Cosentini R, Blasi F, Raccanelli R et al (1996) Severe community-acquired pneumonia: a possible role for Chlamydia pneumoniae. Respiration 63(2):61–65
Woodhead MA, Arrowsmith J, Chamberlain-Webber R, Wooding S, Williams I (1991) The value of routine microbial investigation in community-acquired pneumonia. Respir Med 85(4):313–317
Boersma WG, Löwenberg A, Holloway Y, Kuttschrütter H, Snijder JA, Koëter GH (1991) Pneumococcal capsular antigen detection and pneumococcal serology in patients with community acquired pneumonia. Thorax 46:902–906
Boersma WG, Daniels JM, Löwenberg A, Boeve WJ, van de Jagt EJ (2006) Reliability of radiographic findings and the relation to etiologic agents in community-acquired pneumonia. Respir Med 100(5):926–932
Bohte R, van Furth R, van den Broek PJ (1995) Aetiology of community-acquired pneumonia: a prospective study among adults requiring admission to hospital. Thorax 50:543–547
Endeman H, Schelfhout V, Voorn GP, van Velzen-Blad H, Grutters JC, Biesma DH (2008) Clinical features predicting failure of pathogen identification in patients with community acquired pneumonia. Scand J Infect Dis 40(9):715–720
Holloway Y, Snijder JA, Boersma WG (1993) Demonstration of circulating pneumococcal immunoglobulin G immune complexes in patients with community-acquired pneumonia by means of an enzyme-linked immunosorbent assay. J Clin Microbiol 31(12):3247–3254
Templeton KE, Scheltinga SA, van den Eeden WC, Graffelman AW, van den Broek PJ, Claas EC (2005) Improved diagnosis of the etiology of community-acquired pneumonia with real-time polymerase chain reaction. Clin Infect Dis 41(3):345–351
van der Eerden MM, Vlaspolder F, de Graaff CS, Groot T, Jansen HM, Boersma WG (2005) Value of intensive diagnostic microbiological investigation in low- and high-risk patients with community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 24(4):241–249
Vegelin AL, Bissumbhar P, Joore JC, Lammers JW, Hoepelman IM (1999) Guidelines for severe community-acquired pneumonia in the western world. Neth J Med 55(3):110–117
Cillóniz C, Ewig S, Polverino E et al (2011) Microbial aetiology of community-acquired pneumonia and its relation to severity. Thorax 66(4):340–346
Falcó V, Fernández de Sevilla T, Alegre J, Ferrer A, Martínez Vázquez JM (1991) Legionella pneumophila. A cause of severe community-acquired pneumonia. Chest 100:1007–1011
Falguera M, Sacristán O, Nogués A et al (2001) Nonsevere community-acquired pneumonia: correlation between cause and severity or comorbidity. Arch Intern Med 161(15):1866–1872
García-Ordóñez MA, García-Jiménez JM, Páez F et al (2001) Clinical aspects and prognostic factors in elderly patients hospitalised for community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 20(1):14–19
García-Vázquez E, Soto S, Gómez J, Herrero JA (2008) Simple criteria to assess mortality in patients with community-acquired pneumonia. Med Clin (Barc) 131(6):201–204
Garcia-Vidal C, Carratalà J, Fernández-Sabé N et al (2009) Aetiology of, and risk factors for, recurrent community-acquired pneumonia. Clin Microbiol Infect 15(11):1033–1038
Gómez J, Baños V, Ruiz Gómez J et al (1996) Prospective study of epidemiology and prognostic factors in community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 15(7):556–560
Ewig S, Bauer T, Hasper E, Pizzulli L, Kubini R, Lüderitz B (1995) Prognostic analysis and predictive rule for outcome of hospital-treated community-acquired pneumonia. Eur Respir J 8(3):392–397
Krüger S, Ewig S, Papassotiriou J et al (2009) Inflammatory parameters predict etiologic patterns but do not allow for individual prediction of etiology in patients with CAP: results from the German competence network CAPNETZ. Respir Res 10:65
Steinhoff D, Lode H, Ruckdeschel G et al (1996) Chlamydia pneumoniae as a cause of community-acquired pneumonia in hospitalized patients in Berlin. Clin Infect Dis 22(6):958–964
Bella F, Tort J, Morera MA, Espaulella J, Armengol J (1993) Value of bacterial antigen detection in the diagnostic yield of transthoracic needle aspiration in severe community acquired pneumonia. Thorax 48(12):1227–1229
Blanquer J, Blanquer R, Borrás R et al (1991) Aetiology of community acquired pneumonia in Valencia, Spain: a multicentre prospective study. Thorax 46(7):508–511
Briones ML, Blanquer J, Ferrando D, Blasco ML, Gimeno C, Marín J (2006) Assessment of analysis of urinary pneumococcal antigen by immunochromatography for etiologic diagnosis of community-acquired pneumonia in adults. Clin Vaccine Immunol 13(10):1092–1097
Valencia M, Badia JR, Cavalcanti M et al (2007) Pneumonia severity index class v patients with community-acquired pneumonia: characteristics, outcomes, and value of severity scores. Chest 132(2):515–522
Rello J, Rodriguez R, Jubert P, Alvarez B (1996) Severe community-acquired pneumonia in the elderly: epidemiology and prognosis. Study Group for Severe Community-Acquired Pneumonia. Clin Infect Dis 23(4):723–728
Rello J, Bodi M, Mariscal D et al (2003) Microbiological testing and outcome of patients with severe community-acquired pneumonia. Chest 123(1):174–180
Rello J, Quintana E, Ausina V, Net A, Prats G (1993) A three-year study of severe community-acquired pneumonia with emphasis on outcome. Chest 103(1):232–235
Riquelme R, Torres A, El-Ebiary M et al (1996) Community-acquired pneumonia in the elderly: a multivariate analysis of risk and prognostic factors. Am J Respir Crit Care Med 154(5):1450–1455
Ruiz-González A, Falguera M, Nogués A, Rubio-Caballero M (1999) Is Streptococcus pneumoniae the leading cause of pneumonia of unknown etiology? A microbiologic study of lung aspirates in consecutive patients with community-acquired pneumonia. Am J Med 106(4):385–390
Sordé R, Falcó V, Lowak M et al (2011) Current and potential usefulness of pneumococcal urinary antigen detection in hospitalized patients with community-acquired pneumonia to guide antimicrobial therapy. Arch Intern Med 171(2):166–172
Torres A, Serra-Batlles J, Ferrer A et al (1991) Severe community-acquired pneumonia. Epidemiology and prognostic factors. Am Rev Respir Dis 144(2):312–318
Zalacain R, Torres A, Celis R et al (2003) Community-acquired pneumonia in the elderly: Spanish multicentre study. Eur Respir J 21(2):294–302
Howard LSGE, Sillis M, Pasteur MC, Kamath AV, Harrison BDW (2005) Microbiological profile of community-acquired pneumonia in adults over the last 20 years. J Infect 50:107–113
Lim WS, Macfarlane JT, Boswell TC et al (2001) Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines. Thorax 56(4):296–301
[No authors listed] (1992) The aetiology, management and outcome of severe community-acquired pneumonia on the intensive care unit. The British Thoracic Society Research Committee and The Public Health Laboratory Service. Respir Med 86(1):7–13
Venkatesan P, Gladman J, Macfarlane JT et al (1990) A hospital study of community acquired pneumonia in the elderly. Thorax 45(4):254–258
Gutiérrez F, Masiá M, Mirete C et al (2006) The influence of age and gender on the population-based incidence of community-acquired pneumonia caused by different microbial pathogens. J Infect 53(3):166–174
Lorente ML, Falguera M, Nogués A, González AR, Merino MT, Caballero MR (2000) Diagnosis of pneumococcal pneumonia by polymerase chain reaction (PCR) in whole blood: a prospective clinical study. Thorax 55:133–137
Martínez-Moragón E, García Ferrer L, Serra Sanchis B, Fernández Fabrellas E, Gómez Belda A, Julve Pardo R (2004) Community-acquired pneumonia among the elderly: differences between patients living at home and in nursing homes. Arch Bronconeumol 40(12):547–552
Menéndez R, Córdoba J, de La Cuadra P et al (1999) Value of the polymerase chain reaction assay in noninvasive respiratory samples for diagnosis of community-acquired pneumonia. Am J Respir Crit Care Med 159(6):1868–1873
Molinos L, Fernandez R, Dominguez MJ, Riesgo C, Escudero C, Martinez J (1997) Adenosine deaminase activity in the aetiological diagnosis of community-acquired pneumonia. Scand J Infect Dis 29(3):287–290
Molinos L, Clemente MG, Miranda B et al (2009) Community-acquired pneumonia in patients with and without chronic obstructive pulmonary disease. J Infect 58(6):417–424
Sopena N, Sabrià M, Pedro-Botet ML et al (1999) Prospective study of community-acquired pneumonia of bacterial etiology in adults. Eur J Clin Microbiol Infect Dis 18(12):852–858
Pachon J, Prados MD, Capote F, Cuello JA, Garnacho J, Verano A (1990) Severe community-acquired pneumonia. Etiology, prognosis, and treatment. Am Rev Respir Dis 142(2):369–373
Pareja A, Bernal C, Leyva A, Piedrola G, Maroto MC (1992) Etiologic study of patients with community-acquired pneumonia. Chest 101:1207–1210
Querol-Ribelles JM, Tenías JM, Querol-Borrás JM et al (2005) Levofloxacin versus ceftriaxone plus clarithromycin in the treatment of adults with community-acquired pneumonia requiring hospitalization. Int J Antimicrob Agents 25(1):75–83
Huss A, Scott P, Stuck AE, Trotter C, Egger M (2009) Efficacy of pneumococcal vaccination in adults: a meta-analysis. CMAJ 180(1):48–58
Musher DM, Sampath R, Rodriguez-Barradas MC (2011) The potential role for protein-conjugate pneumococcal vaccine in adults: what is the supporting evidence? Clin Infect Dis 52(5):633–640
Bakaletz LO (1995) Viral potentiation of bacterial superinfection of the respiratory tract. Trends Microbiol 3(3):110–114
Rozenbaum MH, van Hoek AJ, Fleming D, Trotter CL, Miller E, Edmunds WJ (2012) Vaccination of risk groups in England using the 13 valent pneumococcal conjugate vaccine: economic analysis. BMJ 345:e6879
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rozenbaum, M.H., Pechlivanoglou, P., van der Werf, T.S. et al. The role of Streptococcus pneumoniae in community-acquired pneumonia among adults in Europe: a meta-analysis. Eur J Clin Microbiol Infect Dis 32, 305–316 (2013). https://doi.org/10.1007/s10096-012-1778-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1778-4