Abstract
Objectives
To explore clinical and laboratory characteristics of primary Sjögren’s syndrome (pSS) complicated with interstitial lung disease (ILD) and investigate the risk factors for respiratory infections in pSS-ILD.
Methods
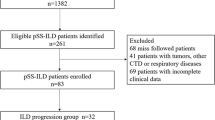
A cohort of 162 pSS-ILD patients in Peking University People’s Hospital from 2015 to 2020 were included, and all medical records were completely collected. We screened 53 patients suffering from respiratory infections as study cases, compared with 109 age- and sex-matched controls. Differences between infection group and control group were compared. Univariate and multivariate binary logistic regression tests were conducted to identify potential risk factors for respiratory infections in pSS-ILD patients.
Results
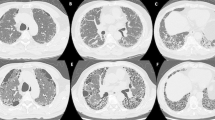
Among 162 pSS-ILD patients, 32.72% (53/162) suffered from respiratory infections. The most frequent type of ILD was nonspecific interstitial pneumonia (32.08%, 51/159), and the most common type of pathogen was bacteria (64.25%, 34/53). Infection group showed higher levels of ESSDAI (P < 0.001), CRP (P < 0.001), ESR (P = 0.003), and C3 (P = 0.020) but lower level of DLCO-SB (P = 0.015). Univariate logistic model revealed that PAH and the use of glucocorticoid increased infection risk in pSS-ILD patients. On multivariate logistic regression analysis, PAH (OR = 3.993, 95% CI = 1.192–13.373, P = 0.025) and severe reduction of DLCO (DLCO-SB < 40%, OR = 4.625, 95% CI = 1.281–16.702, P = 0.019) were significantly associated with increased risk of respiratory infections in pSS-ILD patients.
Conclusion
Among pSS-ILD patients, the most frequent type of ILD was nonspecific interstitial pneumonia. In patients with infection, bacteria were the most common pathogen. Higher levels of ESSDAI, CRP, ESR, and C3 may be correlated with increased infection risk. PAH and reduction of DLCO were identified as independent risk factors.
Key Points • ILD and infectious diseases severely affect pSS patient conditions. • Higher levels of ESSDAI, CRP, ESR, and C3 may be correlated with increased infection risks in pSS-ILD. • PAH and reduction of DLCO were identified as independent risk factors for lower respiratory infection. |


Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Gabriel SE, Michaud K (2009) Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 11(3):229
Palm O, Garen T, Berge Enger T et al (2013) Clinical pulmonary involvement in primary Sjogren’s syndrome: prevalence, quality of life and mortality--a retrospective study based on registry data. Rheumatology (Oxford, England). 52(1):173–179
American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias (2002) This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 165(2):277–304
Wang Y, Hou Z, Qiu M et al (2018) Risk factors for primary Sjgren syndrome-associated interstitial lung disease. J Thorac Dis 10(4):2108–2117
Meyer-Olson D, Witte T (2011) Immunology: prevention of infections in patients with autoimmune diseases. Nat Rev Rheumatol 7(4):198–200
Pease C, Pope JE, Truong D et al (2012) Comparison of anti-TNF treatment initiation in rheumatoid arthritis databases demonstrates wide country variability in patient parameters at initiation of anti-TNF therapy. Semin Arthritis Rheum 41(1):81–89
Fox RI, Fox CM (2011) Sjögren’s syndrome: infections that may play a role in pathogenesis, mimic the disease, or complicate the patient’s course. Indian J Rheumatol 6(1):13–25
Woodhead M, Blasi F, Ewig S et al (2011) Guidelines for the management of adult lower respiratory tract infections--full version. Clin Microbiol Infect 17(Suppl 6):E1–E59
Miller JM, Binnicker MJ, Campbell S et al (2018) A guide to utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2018 update by the Infectious Diseases Society of America and the American Society for Microbiology. Clin Infect Dis 67(6):e1–e94
Luppi F, Sebastiani M, Silva M et al (2020) Interstitial lung disease in Sjögren’s syndrome: a clinical review. Clin Exp Rheumatol 38:291–300
Flament T, Bigot A, Chaigne B et al (2016) Pulmonary manifestations of Sjögren’s syndrome. Eur Respir Rev 25(140):110–123
Mathieu A, Cauli A, Pala R et al (1995) Tracheo-bronchial mucociliary clearance in patients with primary and secondary Sjögren’s syndrome. Scand J Rheumatol 24(5):300–304
Newball HH, Brahim SA (1977) Chronic obstructive airway disease in patients with Sjögren’s syndrome. Am Rev Respir Dis 115(2):295–304
Soto-Cardenas MJ, Perez-De-Lis M, Bove A et al (2010) Bronchiectasis in primary Sjögren’s syndrome: prevalence and clinical significance. Clin Exp Rheumatol 28(5):647–653
Fairfax AJ, Haslam PL, Pavia D et al (1981) Pulmonary disorders associated with Sjögren’s syndrome. Q J Med 50(199):279–295
Kelly C, Gardiner P, Pal B et al (1991) Lung function in primary Sjögren’s syndrome: a cross sectional and longitudinal study. Thorax 46(3):180–183
García-Carrasco M, Ramos-Casals M, Rosas J et al (2002) Primary Sjögren syndrome: clinical and immunologic disease patterns in a cohort of 400 patients. Medicine 81(4):270–280
Zhang T, Yuan F, Xu L et al (2020) Characteristics of patients with primary Sjögren’s syndrome associated interstitial lung disease and relevant features of disease progression. Clin Rheumatol 39(5):1561–1568
Lin W, Xin Z, Zhang J et al (2022) Interstitial lung disease in primary Sjögren’s syndrome. BMC Pulm Med 22(1):73
Almirall J, Serra-Prat M, Bolíbar I et al (2017) Risk factors for community-acquired pneumonia in adults: a systematic review of observational studies. Respiration 94(3):299–311
Danza Á, Graña D, Goñi M et al (2016) Hydroxychloroquine for autoimmune diseases. Rev Med Chil 144(2):232–240
Nirk EL, Reggiori F, Mauthe M (2020) Hydroxychloroquine in rheumatic autoimmune disorders and beyond. EMBO Mol Med 12(8):e12476
Tishler M, Yaron I, Shirazi I et al (1999) Hydroxychloroquine treatment for primary Sjögren’s syndrome: its effect on salivary and serum inflammatory markers. Ann Rheum Dis 58(4):253–256
Yao X, Ye F, Zhang M et al (2020) In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis 71(15):732–739
Rogliani P, Calzetta L, Cavalli F et al (2016) Pirfenidone, nintedanib and N-acetylcysteine for the treatment of idiopathic pulmonary fibrosis: a systematic review and meta-analysis. Pulm Pharmacol Ther 40:95–103
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183(6):788–824
Muramatsu Y, Sugino K, Ishida F et al (2016) Effect of inhaled N-acetylcysteine monotherapy on lung function and redox balance in idiopathic pulmonary fibrosis. Respir Investig 54(3):170–178
Mathai SC, Danoff SK (2016) Management of interstitial lung disease associated with connective tissue disease. BMJ (Clinical research ed). 352:h6819
Raghu G, Remy-Jardin M, Richeldi L et al (2022) Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 205(9):e18–e47
Martinez FJ, de Andrade JA, Anstrom KJ et al (2014) Randomized trial of acetylcysteine in idiopathic pulmonary fibrosis. N Engl J Med 370(22):2093–2101
Shi H, Yin D, Bonella F et al (2020) Efficacy, safety, and tolerability of combined pirfenidone and N-acetylcysteine therapy: a systematic review and meta-analysis. BMC Pulm Med 20(1):128
Zhou X, Liu Y, Jin Y et al (2021) Immune responses after influenza vaccination in patients of primary Sjögren’s syndrome. Rheumatology (Oxford, England). 60(1):224–230
Singh JA, Saag KG, Bridges SL Jr et al (2016) 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol (Hoboken, NJ). 68(1):1–26
Furer V, Rondaan C, Heijstek MW et al (2020) 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 79(1):39–52
Murdaca G, Orsi A, Spanò F et al (2016) Vaccine-preventable infections in systemic lupus erythematosus. Hum Vaccin Immunother 12(3):632–643
Funding
This study was supported by the National Natural Science Foundation of China and by the Beijing Sci-Tech Program [Z191100006619114], NSFC (Natural Science Foundation of China) Grant [81701607], and Peking University People’s Hospital Scientific Research Development Funds [RDZH2022-03].
Author information
Authors and Affiliations
Contributions
XZ and HL drafted the manuscript and performed most of the data collection. JH and YJ conceived the study and participated in its design and coordination, and interpreted the data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Disclosures
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, X., Li, H., Wang, N. et al. Respiratory infection risk in primary Sjögren’s syndrome complicated with interstitial lung disease: a retrospective study. Clin Rheumatol 43, 707–715 (2024). https://doi.org/10.1007/s10067-023-06803-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06803-5