Abstract
Background
Despite the value of simulation for surgical training, it is unclear whether acquired competencies persist long term. A prior randomized trial showed that structured simulation improves knowledge of the safe use of electrosurgery (ES) amongst trainees up to 3 months after the curriculum (Madani et al. in Surg Endosc 28(10):2772–2782, 2014). We now analyse long-term knowledge retention. This study estimates the effects of a structured simulation-based curriculum to teach the safe use of ES on knowledge after 1 year.
Methods
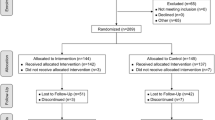
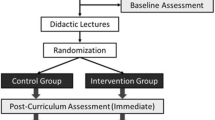
Trainees previously participated in a 1-h didactic ES course, followed by randomization into one of two groups: an unstructured hands-on session where trainees used ES devices (control group) or a goal-directed hands-on training session (Sim group). Knowledge of pre- and post-curriculum (immediate, 3 months and 1 year) and knowledge of ES safety were assessed using different multiple-choice examinations. Data are expressed as median (interquartile range), *p < 0.05.
Results
Fifty-nine trainees participated (30 control group; 29 Sim group). Despite equal baseline examination scores, Sim group demonstrated higher scores compared to control immediately (89 % [83; 94] vs. 83 % [71; 86]*), 3 months (77 % [69; 90] vs. 60 % [51; 80]*) and 1 year after curriculum (70 % [61; 74] vs. 60 % [31; 71]*). One-year score remained significantly greater compared to baseline in the Sim group (70 % [61; 74] vs. 49 % [43; 57]*), but was similar to baseline in the control group (60 % [31; 71] vs. 45 % [34; 52]).
Conclusions
After ES simulation training, retention of competencies persists longer when the hands-on component is designed to reinforce specific learning objectives in a structured curriculum. Despite routine clinical use of ES devices, knowledge degrades overtime, suggesting the need for ongoing formal educational activities to reinforce curricular objectives.



Similar content being viewed by others
References
Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL (2006) The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg 243:864–871 (discussion 871–865)
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, Cools-Lartigue J, Kayssi A, Lipsman N, Elmi M, Kulkarni AV, Parshuram C, Mainprize T, Warren RJ, Fata P, Gorman MS, Feinberg S, Rutka J (2014) A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 259:1041–1053
Kasotakis G, Lakha A, Sarkar B, Kunitake H, Kissane-Lee N, Dechert T, McAneny D, Burke P, Doherty G (2014) Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg 260:483–490 (discussion 490–483)
Bridges M, Diamond DL (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 177:28–32
Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ (2005) Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 27:10–28
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ (2006) Surgical simulation: a systematic review. Ann Surg 243:291–300
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 (discussion 463–454)
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525 (discussion 525–518)
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, Minter RM (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243:854–860 (discussion 860–853)
Hyltander A, Liljegren E, Rhodin PH, Lonroth H (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA III, Ramel S, Smith CD, Arvidsson D (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, Hutchison C (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177:167–170
Tsuda S, Scott D, Doyle J, Jones DB (2009) Surgical skills training and simulation. Curr Probl Surg 46:271–370
Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ (2014) A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy. Ann Surg 259:236–248
Palter VN, Orzech N, Reznick RK, Grantcharov TP (2013) Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 257:224–230
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199:115–120
Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD, Force FT (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Madani A, Watanabe Y, Vassiliou MC, Fuchshuber P, Jones DB, Schwaitzberg SD, Fried GM, Feldman LS (2014) Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28:2772–2782
Feldman LS, Brunt LM, Fuchshuber P, Jones DB, Jones SB, Mischna J, Munro MG, Rozner MA, Schwaitzberg SD, Committee SF (2013) Rationale for the fundamental use of surgical energy (FUSE) curriculum assessment: focus on safety. Surg Endosc 27:4054–4059
Zevin B, Levy JS, Satava RM, Grantcharov TP (2012) A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg 215(580–586):e583
Madani A, Jones DB, Fuchshuber P, Robinson TN, Feldman LS (2014) Fundamental Use of Surgical Energy (FUSE): a curriculum on surgical energy-based devices. Surg Endosc 28:2509–2512
Fuchshuber PR, Robinson TN, Feldman LS, Jones DB, Schwaitzberg SD (2014) The SAGES FUSE program: bridging a patient safety gap. Bull Am Coll Surg 99:18–27
Mayooran Z, Pearce S, Tsaltas J, Rombauts L, Brown TI, Lawrence AS, Fraser K, Healy DL (2004) Ignorance of electrosurgery among obstetricians and gynaecologists. BJOG 111:1413–1418
Ericsson K, Krampe R, Tesch-Romer C (1993) The role of deliberate practice in the acquisition of expert performance. Psychol Rev 100:363–406
Ericsson K, Charness N (1994) Expert performance: its structure and acquisition. Am Psychol 49:725–747
Jowett N, LeBlanc V, Xeroulis G, MacRae H, Dubrowski A (2007) Surgical skill acquisition with self-directed practice using computer-based video training. Am J Surg 193:237–242
Dale E (1969) Audiovisual methods in teaching, 3rd edn. Holt, Reinhart and Winston, New York
Lajoie S, Azevedo R (2006) Teaching and learning in technology-rich environments. In: Alexander P, Winne P (eds) Handbook of educational psychology. Routledge, New York, pp 803–821
Stefanidis D, Heniford BT (2009) The formula for a successful laparoscopic skills curriculum. Arch Surg 144:77–82 (discussion 82)
Acknowledgments
We acknowledge the SAGES FUSE task force for the development of the FUSE curriculum and presentation slides, as well as the facilitators who assisted in conducting the electrosurgery course. AM is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program.
Disclosures
The Steinberg-Bernstein Centre receives unrestricted educational grants from ConMed and Covidien Canada. Dr. Melina Vassiliou was a consultant for Covidien. Dr. Daniel Jones was a consultant for Intuitive and Allurion. Dr. Steven Schwaitzberg was a consultant for Stryker, Olympus, Human Extension and Acuity Bio. Drs. Amin Madani, Yusuke Watanabe, Pascal Fuchshuber, Gerald M. Fried and Liane S. Feldman have no conflicts of interest or financial ties to disclose. Dr. Amin Madani is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Madani, A., Watanabe, Y., Vassiliou, M.C. et al. Long-term knowledge retention following simulation-based training for electrosurgical safety: 1-year follow-up of a randomized controlled trial. Surg Endosc 30, 1156–1163 (2016). https://doi.org/10.1007/s00464-015-4320-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4320-9