Abstract
Background
The cerebral palsy is highly actual issue of pediatrics, causing significant neurological disability. Though the great progress in the neuroscience has been recently achieved, the pathogenesis of cerebral palsy is still poorly understood.
Methods
In this work, we reviewed available experimental and clinical data concerning the role of immune cells in pathogenesis of cerebral palsy. Maintaining of homeostasis in nervous tissue and its transformation in case of periventricular leukomalacia were analyzed.
Results
The reviewed data demonstrate involvement of immune regulatory cells in the formation of nervous tissue imbalance and chronicity of inborn brain damage. The supported opinion, that periventricular leukomalacia is not a static phenomenon, but developing process, encourages our optimism about the possibility of its correction.
Conclusions
The further studies of changes of the nervous and immune systems in cerebral palsy are needed to create fundamentally new directions of the specific therapy and individual schemes of rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction (problem relevance)
The Cerebral Palsy (CP) is one of the most common diseases that cause severe neurological disability. The worldwide prevalence of CP is approximately 2–2.5 per 1000 live births [38]. It has been clinically defined as a “group of permanent disorders of the development of movement and posture, causing activity limitation that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain” [49]. Despite the remarkable developing brain’s plasticity, severe disturbance of neuronal development, and normal myelination because of neonatal brain injury generates life-persisting sensory-motor and cognitive deficits in the growing child with wide variability of clinical manifestations and variety of neurological symptoms.
The significance of the clinical issue is very high, since CP is a frequent, disabling, and costly problem. Current medicine puts emphasis on the early diagnosis of organic lesions of the central nervous system (CNS), because an early start of the treatment and rehabilitation gives better chance of achieving good outcomes [29]. The rehabilitation programs, in fact, are symptomatic and they are developed based on existing syndromes with orientation on the goal of improving functioning status of patient; as of today, there is no therapy strategies for CP based on its pathophysiology. In addition, the existing insight into the pathogenesis of nervous degenerations, which can include, with certain reservations, the children’s cerebral palsy, is because nerve cells losses greatly exceed the low regenerative potential of nervous tissue. This view in conjunction with a stereotype of conservative attitudes predetermines hopelessness in the rehabilitation results. The most successful therapy and rehabilitation are based on pathogenic mechanisms. Given the successes in neurobiological science and modern advances in molecular biology and genetics, the approaches to the treatment and rehabilitation of children with cerebral palsy will evolve to reflect this new knowledge [15, 30, 41, 42].
Undoubtedly, the origin of the clinical manifestations of the CP is the abnormality of brain development [27, 37]. At the same time, there are still many problematic issues and unresolved questions. There is no definitive explanation of the fact that some children diagnosed with brain pathology using various imaging types have certain clinical manifestation of cerebral palsy; whereas, in other children with the same pattern of brain pathology, the clinic is absent or negligible. Why are the pathological changes not demonstrated in the brain of 30 % of children with cerebral palsy using available imaging techniques? There are clinical studies which indicate that children with the same morphological picture of brain injury may have different clinical manifestations of cerebral palsy that may not follow classical topographic neurology [16, 50]. The answers to these and the other questions regarding pathogenesis and clinical progress of cerebral palsy are necessary for the formulation of pathogenesis-based therapy and rehabilitation strategy that places the ultimate goal on the improvement of the treatment outcomes in this complex pediatric pathology.
Data sources and searches
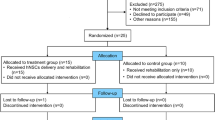
We searched PubMed, Google Scholar, Scopus, and Web of Science databases in August 2015 with no restrictions by date using a combination of keywords and text words related to cerebral palsy and immune regulation of nervous tissue homeostasis. The main MeSH descriptor in PubMed were CNS/immunology, CP/Neurogenesis, and Leucomalacia periventricular/etiology. Criteria for considering studies for this review were containing of data about immunological regulation of brain development and immunological changes accompanying CP. Inclusion criteria were peer-reviewed published articles on CP and immunological regulation, original research articles, reviews, meeting abstracts, proceedings papers, and book chapters. Exclusion criteria were documents that were not published in the public domain. All selected studies deemed suitable (69 articles from 117) were retrieved independently by the two authors to determine inclusion. Disagreements were resolved through consensus.
Review
The modern concept of the pathogenesis of cerebral palsy in children considers two major interrelated mechanisms. On one hand, there is severe imbalance of homeostasis in the ischemic nervous tissue secondary to the disturbance of blood supply and dysregulation of apoptotic cell death [61, 64, 65]. On the other hand, there is immune dysregulation resulting in the formation of autoreactivity against damaged nervous tissue [14, 43, 66]. This approach gives some of the most important and promising directions to modern studies of cerebral palsy pathogenesis and the development of its treatment.
Functional anatomy of the nervous tissue
Recent studies have shown that the activity of neurons and nervous system in general is homeostatically regulated [18, 35, 54]. It is well known that the integration of the functional activity of the cells of various tissues in a single unit and managing the process of restructuring the tissue are influenced by regulatory systems. According to the current concepts, the interaction of the immune, nervous, and endocrine systems maintains information balance in the organism. Blood and lymph circulation creates the communication channels and enables the exchange of this information [47, 57]. At the tissue level, the process of information exchange is realized by constant synthesis of chemokines and cell adhesion molecules to ensure synchronization of the processes occurring under the control of regulatory systems [68]. If the basic mechanisms of the transmission of regulatory systems signals in general are well described, the clarification of the mechanisms of coordinated interaction of various messengers providing intercellular communication and allowing the cells to respond adequately to the ever-changing milieu is more complex and poorly understood part of the problem. The problem concerning study of intercellular communication is even more complicated considering that the extracellular matrix plays an active role in the formation of tissue ensemble and facilitates the process of cell migration [58]. In addition to collagen and elastin fibers in the structure of extracellular matrix, there are also adhesive glycoproteins, cytokines, hormones, and growth factors involved [47]. The extracellular matrix regulates the important processes of development, growth, and function of neurons [68]. Thus, tissue ensemble formation is a complex hierarchical system with many well-known components, as well as some poorly understood players. The possible direction of tissue homeostasis research lies in finding the integral indicators, which reflect the state of the tissue and the potential direction of its development in particular time. It is logical to look for markers of tissue behavior among parameters of regulatory systems, working in close relationship with each other. From this point of view, the functional anatomy of the nervous tissue should be under sighting consideration.
The unique lymphatic drainage system of the brain [4, 32], existence of blood-brain barrier [40], and low levels of expression of the Major Histocompatibility Complex (MHC) molecules on the brain cells provide a basis to consider that the CNS is an immune-privileged organ [5]. Recent advances in this field clearly demonstrate that the concept of CNS immune privilege “seems somewhat obsolete in the setting of acute infection” [20], and it was also reconsidered in case of tissue homeostasis regulation [13]. This privilege should rather be interpreted as a presence of a special set of rules applied to receptor-mediated immune cell entry into the CNS [13]. Moreover, the immune cells are present in the nervous system itself, and various forms of immune response can arise and develop under suitable conditions [9, 23]. It is believed, that the formation of any type of immune response in the CNS is undesirable, but not always means appearance of the pathological process [69]. The blood-brain barrier is currently considered not as a filter, but rather as selective flux of substances, information molecules, and ions due to tight intercellular connections between neurons, glial cells, and the endothelium of brain capillaries [28, 40]. The most interesting is the function of astrocytes and microglia; the research of which has led to the assumption that these cells may mediate the presence of specific features of the barrier phenotype in the microvascular endothelium of the brain. It was also found that under some circumstances, the brain endothelium enhances the growth and differentiation of the associated astrocytes; the cultivated endothelial cells of brain and astrocytes express functional receptors for a large number of agents that act as neurotransmitters and modulators in the brain [1]. Neuronal surface antigens include molecules directly involved in neurotransmission process. The experimental data suggest that there is a possibility of signal transfer between cells in neurovascular unit including microglia and oligodendrocytes [36, 48]. In addition, the signal communication between microglia, astrocytes, and neurons can be significant in various pathologies of the brain [31].
The astrocytes and endothelial cells of the brain are considered as controllers of neuronal homeostasis, therefore, their dysfunction has significant effects on the neurophysiological level. The most comprehensive, in our view, should be a concept of regulation of homeostasis in the nervous tissue, which includes, along with neurovascular unit, the cells of immune system and the extracellular matrix. According to this concept, the CNS is able to respond to the damage by various pathogens (toxins, trauma, degenerative stimulus) with the development of a complex cascade of processes at cellular and tissue levels, conditionally called neuroinflammation [69]. This chain of reaction is carried out as a result of concerted action of recirculating regulatory T-lymphocytes (Foxp3+, CD25++CD4+) [34, 57] and tissue immune cells (which include microglial cells and astrocytes) [23, 51], endothelial cells and neurons, that in complex form an immunoregulatory zone. The immunoregulatory zone is, in fact, peripheral compartment or tertiary lymphoid organ of the immune system [59], i.e., the unit where an interaction of regulatory immune cells with tissue structures, information transfer, and the formation of tissue homeostasis take place.
Neurogenesis opportunity in children with CP
Development of modern concept of CP pathogenesis requires deeper and more thorough study of the complex and changing patterns of neurogenesis. Neural stem and progenitor cells, contained in the central nervous system of adult organisms in the certain amount, retain the ability to generate new neurons in certain areas of the brain [3]. This neurogenesis in the postnatal brain is the most important form of neuroplasticity required for its function [46]. Neuroplasticity is the amazing ability of the brain to change its basic structure and function; some of these changes are short-lived, but very obvious, while others are less visible, but lasting [55]. The genes, the mechanisms of brain development, and neuroplasticity tied together play a leading role in the formation of brain condition [19]. From the perspective of a very broad concept of neuroplasticity, which implies adaptation of the nervous system in health and disease at all levels from the systemic to the synaptic, almost all the events occurring in the functioning brain could be interpreted. Violation of neurogenesis is considered to be a key pathogenic mechanism of various diseases of the brain [24, 60, 67]. The question of the degree of involvement of neurogenesis caused by various injuries in the restoration of the brain is generally open. Building on the recent advances, there is an “unneurocentric” point of view being developed regarding different disorders of the nervous system, which assumes participation of other cellular elements of the brain besides neurocytes in the etiology of the disease [22].
The neurogenic inflammation apparently results in the homeostasis imbalance, which stimulates increase of metabolic activity and information requirements allowing to implementing the feature of neuroplasticity [69]. The basis of neuronal inflammation is malfunction of neuroglial nets and related disorders of the blood-brain barrier. In this case, the classic inflammatory mediators, cytokines, and prostaglandins, carry out neuromodulator functions in the brain. Thus, concerning regulatory function of immune system in relation to tissue homeostasis [54], reactions initiated by regulatory pool of T-cells on the tissue level is not true inflammation, but rather a physiological process of tissue steady-state maintaining [57]. Disturbance on the tissue level may also be supported by central regulatory mechanisms [34]. Investigation of cell involvement and composition of extracellular matrix with purpose of its remodeling is one of the most important new research directions as a result of which the new approaches to pathogenetic therapy of cerebral palsy in children can be developed.
The periventricular leukomalacia
(PVL) is one of the most consistent morphological signs of cerebral palsy [16, 26]. PVL is an age-specific form of brain injury in the premature infant, and it is the main cause of subsequent neurological disability, such as spastic motor deficits (cerebral palsy) and cognitive deficits. According to available data in the literature, this process is initiated during the fetal life, and then continues for the duration of the disease [25]. It is kind of a sustained process of the periventricular zone abnormality, initiated in the antenatal period by various influences, especially hypoxia, and continuing throughout the period of childhood [52]. Therefore, the PVL is no longer considered as a static phenomenon, but rather as pathological process of the tissue degradation associated with autosensitization by own brain antigens [43, 66]. This pathological process interferes with effective treatment of the disease. The autoreactive disease nature is confirmed by the fact that in patients with CP detection, frequency of the autoantibodies to the neurospecific protein S-100 have been significantly exceeded the level in healthy individuals; whereas, the number and functional activity of T-lymphocytes have been significantly reduced, especially CD8+ lymphocytes [53]. Interestingly, available laboratory tests do not detect significant differences in antigenic specificity of CD4+ and CD8+ T-cell responses in patients with autoimmune nerve disorders and healthy subjects [10]. Allegedly, distinction could be detected when these responses are dissected down to specific epitopes. Results of studies in this field suggest that differences may not exist in the cell morphology but rather in the functional role of CNS-specific T-cells [2].
The recent advances in the field of physiological regulation of nervous tissue homeostasis, as previously mentioned, involve better understanding of the close interaction between the nervous, endocrine, and immune systems. In the central nervous system, the immune system is represented by three morphologically and functionally different cell factors: lymphoid cells of cerebrospinal fluid; non-lymphoid cells of the nervous tissue - microglia, astrocytes, oligodendrocytes; and endothelial cells of cerebral vessels. In addition, activated T-cells can cross the blood-brain barrier penetrating into the CNS and provide immunological surveillance [13, 54]. Cytokines (interferons, interleukins, TNF, etc.) as immune system mediators are involved in interactions between immune and nerve cells, including a mechanism of brain tissue damage and neuron loss [14]. The neuroglia creates a permanent and stable intrinsic environment to the nervous tissue for normal functioning of nerve cells and the maintenance of tissue homeostasis [36]. The majority of neurons (20 to 80 %) die during the nervous tissue histogenesis by apoptosis, i.e., by the programmed physiological cell death. The biological meaning of glia programmed cell death is based on known facts about the physiological role of apoptosis in transferring genetic information to neurocytes necessary for their differentiation and acquisition of specialization [7]. Microglial cells have certain properties of immunocompetent cells. They are capable of migration and phagocytosis of nerve tissue products in the necrosis foci and alien particles and are involved in transporting these products in the perivascular and subarachnoid spaces. Moreover, CD4-marker of T-helpers is expressed on glial cells [11]. This transmembrane glycoprotein is expressed on lymphocytes and on some monocytes, and is involved in recognizing antigens associated with molecules of class II of the MHC, which provides the coordination between various cells of the immune system and plays an important role in the immune response development. Furthermore, neural stem cells have the astroglia phenotype (GFAP + cells), and they are often located in the subependymal layer of the ventricles and periventricular zone of the brain [23]. This once again confirms the importance of this brain area in nerve tissue histogenesis during the postnatal period. Based on the above, the CP patients form a special group with combined nervous and immune system lesions.
The role of apoptosis in pathogenesis of CP
Apoptosis plays central role in maintaining cellular homeostasis of adult organism tissues and organs [17]. It is universal mechanism of genetically programmed cell death, closely linked to the apoptotic body phagocytosis process required for highly specific cells differentiation, including the neural tissue. The cell death coincides with the period of the migration completion, proliferation, and beginning of the tissue-specific differentiation of neural elements [21]. These processes are of particular importance in embryogenesis and the process of nervous tissue formation; in the postnatal period, these processes are less pronounced, but no less important, as they are the foundation for the formation of a mature nervous system [63]. Regarding the participation of apoptosis process in the nervous system diseases, the pathological apoptosis occurs in the ischemic brain lesions [64]. Now, it is clear that both apoptosis and necrosis are significant components of cell death following hypoxic-ischemic injury, but number of different factors determine whether a cell will undergo apoptosis or necrosis [65, 61]. In addition, the apoptosis is one of the ways to eliminate T-cells from neuroinflammation foci. The apoptosis plays a significant role in developing cerebral degeneration, as well as in pathogenesis of children’s cerebral palsy [8]. In turn, degenerative changes in the brain are presumably supported by immune mediated inflammation [39, 56]. Taking into account the importance of the apoptosis and differentiation of neurocytes during the ontogenesis and in the maintenance of the brain function in the postnatal period, it is necessary to investigate the apoptotic status of the patient with CP.
The particular importance is placed on possibilities of using inhibition or activation of the apoptotic type of cell death in the therapy. The therapy targeted at apoptosis can be carried out predominantly in three directions: suppressing the apoptotic process at its redundancy; elimination of the factors stimulating apoptosis; and the use neuronal differentiation inducers. In the early postnatal development, an apoptosis inducer, along with other factors, may be a restriction of the inflow of afferent information, which is the trophic incentive source for both developing and already mature CNS [7]. This is also confirmed by the available facts of importance of sensory inflow as the regulator of the nervous system maturation process, its morphogenesis, damage repair, and trophic support [6, 12, 62]. In essence, a continuous information flow is essential for the nervous system existence and development. This fact explains the role of physical rehabilitation methods in pathogenetic correction process in children with cerebral palsy. An important factor impeding the development of both apoptotic and necrotic changes is to increase the neurotrophic brain provision [33, 45]. This confirms the importance of neurotrophic drugs in medical rehabilitation of patients with cerebral diseases [37, 44].
Conclusions
From the standpoint of immune regulation of tissue homeostasis, the cerebral palsy in children, despite the variety of its clinical forms, can be considered as arising from perinatal and lasting imbalance of the nervous tissue structure leading to persistent functional abnormality. The immunological mechanisms participate in the process of chronicity of hypoxemic-ischemic injuries, which arose during the perinatal period. However, considering the neuroplasticity property of the brain, which is most pronounced at young age, these changes in the nervous tissue may be reversible, which gives hope for the specific treatment effectiveness. In the long term, the identification of morphological and biochemical apoptosis markers and parameters characterizing the immune regulation of tissue homeostasis should contribute to a deeper understanding of the disease pathogenesis, improving the differential diagnosis, and creating fundamentally new directions of the specific therapy. Further study of the nervous and immune system changes may help to develop the individual schemes of treating and rehabilitating children with CP. Gaining more comprehensive understanding of the development mechanisms of cerebral palsy in children as a disease associated with immune system dysfunction has profound clinical implications.
References
Abbott JN, Rоnnbаck L, Hansson E (2006) Astrocyte–endothelial interactions at the blood–brain barrier. Nat Rev Neurosci 7:41–53
Aslam A, Chan H, Warrell DA, Misbah S, Ogg GS (2010) Tracking antigen-specific T-cells during clinical tolerance induction in humans. PLoS One 5(6):e11028
Braun SM, Jessberger S (2014) Adult neurogenesis and its role in neuropsychiatric disease, brain repair and normal brain function. Neuropathol Appl Neurobiol 40(1):3–12
Carare RO, Hawkes CA, Weller RO (2014) Afferent and efferent immunological pathways of the brain. Anatomy, function and failure. Brain Behav Immun 36:9–14
Carson MJ, Doose JM, Melchior B, Schmid CD, Ploix CC (2006) CNS immune privilege: hiding in plain sight. Immunol Rev 213:48–65
Carulli D, Foscarin S, Rossi F (2011) Activity-dependent plasticity and gene expression modifications in the adult CNS. Front Mol Neurosci 28(4):50
Choi C, Benveniste EN (2004) Fas ligand/Fas system in the brain: regulator of immune and apoptotic responses. Brain Res Brain Res Rev 44(1):65–81
Clarke G, Lumsden CJ (2005) Heterogeneous cellular environments modulate one-hit neuronal death kinetics. Brain Res Bull 65(1):59–67
Colton AC (2013) immune heterogeneity in neuroinflammation: dendritic cells in the brain. J NeuroImmune Pharmacol 8(1):145–162
Crawford MP, Yan SX, Ortega SB, Mehta RS, Hewitt RE, Price DA, et al. (2015) High prevalence of autoreactive, neuroantigen-specific CD8+ T cells in multiple sclerosis revealed by novel flow cytometric assay. Blood 103(11):4222–4231
Eggen BJ, Raj D, Hanisch U-K, Boddeke HW (2013) Microglial phenotype and adaptation. J NeuroImmune Pharmacol 8(4):807–823
Ekusheva EV, Damulin IV (2013) Rehabilitation after stroke: the role of neuroplasticity and sensorimotor integration. Zh Nevrol Psikhiatr Im S S Korsakova 113(12Pt2):35–41
Engelhardt B, Liebner S (2014) Novel insights into the development and maintenance of the blood–brain barrier. Cell Tissue Res 355(3):687–699
Folkerth RD, Keefe RJ, Haynes RL, Trachtenberg FL, Volpe JJ, Kinney HC (2004) Interferon-γ expression in periventricular leukomalacia in the human brain. Brain Pathol 14(3):265–274
Gainetdinova DD, Aizatulina DV, Valeeva IK, Iusupova EF (2011) Mechanisms of genome instability in children with periventricular leucomalacia that resulted in cerebral palsy. Zh Nevrol Psikhiatr Im S S Korsakova 111(1):74–77
Gapt AA, Sahu CS (2010) Magnetic resonance imaging in evaluation of periventricular leucomalacia. MJAFL 66(4):374–380
Green D, Reed J (2011) Apoptosis. Physiology and pathology. Cambridge University Press, Cambridge 438p
Hill J, Rom S, Ramirez SH, Persidsky Y (2014) Emerging roles of pericytes in the regulation of the neurovascular unit in health and disease. J NeuroImmune Pharmacol 9(5):591–605
Hsieh J, Eisch AJ (2010) Epigenetics, hippocampal neurogenesis, and neuropsychiatric disorders: unraveling the genome to understand the mind. Neurobiol Dis 39(1):73–84
Huber AK, Irani DN (2015) Is the concept of central nervous system immune privilege irrelevant in the setting of acute infection? Front Oncol 28(5):99
Jaeger A, Fröhlich M, Klum S, Lantow M, Viergutz T, Weiss DG, Kriehuber R (2015) Characterization of apoptosis signaling cascades during the differentiation process of human neural ReNcell VM progenitor cells in vitro. Cell Mol Neurobiol. 35(8):1203–1216
Janigro D, Walker MC (2014) What non-neuronal mechanisms should be studied to understand epileptic seizures? Adv Exp Med Biol 813:253–264
Jensen CJ, Ann M, De Keyser J (2013) Immune players in the CNS: the astrocyte. J NeuroImmune Pharmacol 8(4):824–839
Johnston MV (2011) Clinical disorders of brain plasticity. Brain and Development 26(2):73–80
Katusic A (2011) Early brain injury and plasticity: reorganization and functional recovery. Transl Neurosci 2(1):33–42
Kaur C, Ling EA (2009) Periventricular white matter damage in the hypoxic neonatal brain: role of microglial cells. Prog Neurobiol 4:264–280
Khwaja O, Volpe JJ (2008) Pathogenesis of cerebral white matter injury of prematurity. Archives of disease in childhood. Fetal and Neonatal Edition 93(2):153–161
Kuvacheva NV, Salmina AB, Komleva YK, Malinovskaya NA, Morgun AV, Pozhilenkova EA, et al. (2013) Permeability of the hematoencephalic barrier in normalcy, brain development pathology and neurodegeneration. Zh Nevrol Psikhiatr Im S S Korsakova 113(4):80–85
Lambrecht S, Urra O, Grosu S, Nombela SP (2014) Emerging rehabilitation in cerebral palsy. Emerging Therapies in Neurorehabilitation Biosystems & Biorobotics 4:23–49
Lee RW, Poretti A, Cohen JS, Levey E, Gwynn H, Johnston MV, et al. (2014) Diagnostic approach for cerebral palsy in the genomic era. Neruomol Med 16(4):821–844
Liu Y, Xu X, Dou H, Hua Y, Xu J, Hui X (2015) Apolipoprotein E knockout induced inflammatory responses related to microglia in neonatal mice brain via astrocytes. Int J Clin Exp Med 8(1):737–743
Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, et al. (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523(7560):337–341
Machalinski B, Lazewski-Banaszak P, Dąbkowska E, Paczkowska E, Golab-Janowska M, Nowacki P (2012) The role of neurotrophic factors in regeneration of the nervous system. Neurol Neurochir Pol 46(6):579–590
Martinez-Pasamar S, Abad E, Moreno B, Velez de Mendizabal N, Martinez-Forero I, Garcia-Ojalvo J, Villoslada P (2013) Dynamic cross-regulation of antigen-specific effector and regulatory T cell subpopulations and microglia in brain autoimmunity. BMC Syst Biol 26(7):34
Martino G, Pluchino S, Bonfanti L, Schwartz M (2011) Brain regeneration in physiology and pathology: the immune signature driving therapeutic plasticity of neural stem cells. Physiol Rev 91(4):1281–1304
Michell-Robinson MA, Touil H, Healy LM, Owen DR, Durafourt BA, Bar-Or A, et al. (2015) Roles of microglia in brain development, tissue maintenance and repair. Brain 138(Pt5):1138–1159
Morgun AV, Kuvacheva NV, Taranushenko TE, Khilazheva ED, Malinovskaia NA, Gorina IV, et al. (2013) Current concepts of perinatal ischemic injury in the brain neurovascular unit: molecular targets for neuroprotection. Vestn Ross Akad Med Nauk 12:26–35
Nelson KB (2003) Can we prevent cerebral palsy? N Engl J Med 349:1765–1769
Ngono AE, Pettre S, Salou M, Bahbouhi B, Soulillou J-P, Brouard S, Laplaud D-A (2012) Frequency of circulating autoreactive T cells committed to myelin determinants in relapsing–remitting multiple sclerosis patients. Clin Immunol 144(2):117–126
Obermeier B, Daneman R, Ransohoff RM (2013) Development, maintenance and disruption of the blood-brain barrier. Nat Med 19(12):1584–1596
O’Callaghan ME, MacLennan AH, Haan EA (2009) The genomic basis of cerebral palsy. Hum Genet 1:49–72
Omran A, Elimam D, Shalaby S, Peng J, Yin F (2012) MicroRNAs: a light into the “black box” of neuropediatric diseases? Neuro Molecular Medicine 14(4):244–261
Ortega SB, Kong X, Venkataraman R, Savedra AM, Kernie SG, Stowe AM, Raman L (2015) Perinatal chronic hypoxia induces cortical inflammation, hypomyelination, and peripheral myelin-specific T cell autoreactivity. J Leukoc Biol 99(1):21–29. doi:10.1189/jlb.5HI0914-447R
Park DH, Eve DJ, Chung YG (2010) Regenerative medicine for neurological disorders. The Scientific World J 10:470–489
Perlman JM (2006) Summary proceeding from the neurology group on hypoxic-ischemic encephalopathy. Pediatrics 117(3Pt2):28–30
Pimentel-Coelho PM, Mendez-Otero R (2014) Endogenous regenerative potential of neural stem/progenitor cells of the newborn brain (an overview). Stem Cells and Cancer Stem Cells 11:253–263
Porlan E, Perez-Villalba A, Delgado AC, Ferron SR (2013) Paracrine regulation of neural stem cells in the subependymal zone. Arch Biochem Biophys 534(1–2):11–19
Pushchina EV, Obukhov DK, Varaksin AA (2013) Features of adult neurogenesis and neurochemical signaling in the cherry salmon Oncorhynchus masou brain. Neural Regen Res 8(1):13–23
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B (2007) A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 109:8–14
Rutherford M, Martinez MB, Allsop J, Counsell S, Cowan F (2010) MRI of perinatal brain injury. Pediatr Radiol 40(6):819–833
Salmina AB, Komleva YK, Lopatina OL, Kuvacheva NV, Gorina YV, Panina YA, et al. (2015) Astroglial control of neuroinflammation: TLR3-mediated dsRNA-sensing pathways are in the focus. Rev Neurosci 26(2):143–159
Saugstad OD (2014) Oxygen and oxidative stress in the newborn studies on pediatric disorders. Oxidative Stress in Appl Basic Res Clin Pract 3–13
Semenov AS (2003) Validity of “Gravistat” device for the improvement of statics and locomotion: interrelation with neuro-auto-immune reactions. Aviakosm Ekolog Med 37(1):61–63
Senovilla L, Galluzzi L, Zitvogel L, Kroemer G (2013) Immunosurveillance as a regulator of tissue homeostasis. Trends Immunol 34(10):471–481
Simpkins CA, Simpkins AM (2013) Neuroplasticity and neurogenesis: changing moment-by-moment. Neuroscience for Clinicians 11:165–174
Sindic CJ (2002) Multiple sclerosis: from the immune system to inflammatory demyelination and irreversible neurodegeneration. Bull Mem Acad R Med Belg 157(7–9):391–398
Smigiel KS, Srivastava S, Stolley JM, Campbell DJ (2014) Regulatory T-cell homeostasis: steady-state maintenance and modulation during inflammation. Immunol Rev 259(1):40–59
Soleman S, Filippov MA, Dityatev A, Fawcett JV (2013) Targeting the neural extracellular matrix in neurological disoders. Neuroscience 253:194–213
Stranford S, Ruddle N (2012) Follicular dendritic cells, conduits, lymphatic vessels, and high endothelial venules in tertiary lymphoid organs: parallels with lymph node stroma. Front Immunol 30:3389
Strat YL, Ramoz N, Gorwood P (2009) The role of genes involved in neuroplasticity and neurogenesis in the observation of a Gene-environment interaction (GxE) in schizophrenia. Current Molecular Medicine 9(4):1–13
Sun Y, Zhang Y, Wang X, Blomgren K, Zhu C (2012) Apoptosis-inducing factor downregulation increased neuronal progenitor, but not stem cell, survival in the neonatal hippocampus after cerebral hypoxia-ischemia. Mol Neurodegener 7:17
Tahayori B, Port NL, Koceja DM (2012) The inflow of sensory information for the control of standing is graded and bidirectional. Exp Brain Res 218(1):111–118
Taupin P (2006) Adult neurogenesis and neuroplasticity. Restor Neurol Neurosci 24(1):9–15
Taylor DL, Edwards DA, Mehmet H (1999) Oxidative metabolism, apoptosis and perinatal brain injury. Brain Pathol 9(1:93–117
Thornton C, Rousset CI, Kichev A, Miyakuni Y, Vontell R, Baburamani AA et al. (2012) Molecular Mechanisms of Neonatal Brain Injury. Neurol Res Int Article ID 506320, 16 p
van Coevorden-Hameete MH, de Graaff E, Titulaer MJ, Hoogenraad CC, Sillevis Smitt PA (2014) Molecular and cellular mechanisms underlying anti-neuronal antibody mediated disorders of the central nervous system. Autoimmun Rev 13(3):299–312
Vezzani A, Friedman A, Dingledine RJ (2013) The role of inflammation in epileptogenesis. Neuropharmacology 69:16–24
Wojcik-Stanaszek L, Gregor A, Zalewska T (2011) Regulation of neurogenesis by extracellular matrix and integrins. Acta Neurobiol Exp 71:103–112
Xanthos DN, Sandkuhler J (2014) Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nat Rev Neuroscience 15(1):43–53
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lisovska, N., Daribayev, Z., Lisovskyy, Y. et al. Pathogenesis of cerebral palsy through the prism of immune regulation of nervous tissue homeostasis: literature review. Childs Nerv Syst 32, 2111–2117 (2016). https://doi.org/10.1007/s00381-016-3245-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3245-5