Abstract
Purpose
To determine the utility of systemic inflammatory response and develop a model based on serum inflammatory indices to aid prognostication in patients with upper urinary tract urothelial carcinoma (UTUC).
Methods
The study population comprised 277 patients with non-metastatic UTUC who underwent nephroureterectomy between 1999 and 2010. Multivariate survival analysis was performed using Cox’s proportional hazards model, and a new model was developed to predict recurrence-free (RFS) and disease-specific survival (DSS). The factors considered, in relation to systemic inflammatory responses, were as follows: albumin, white blood cell count, neutrophil count, lymphocyte count, red blood cell count, serum creatinine level, platelet count, prognostic nutritional index, platelet/lymphocyte ratio, neutrophil/lymphocyte ratio (NLR), and derived NLR.
Results
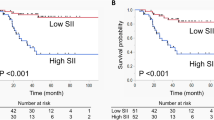
The final model consisted of bladder cuffing, pathologic T stage, lymphovascular invasion, and derived NLR. The bootstrap-concordance indices of the model were 0.778 [95 confidence interval (CI) 0.730–0.826] for RFS and 0.802 (95 % CI 0.752–0.851) for DSS, respectively, and integrated area under the curve value for time to RFS and DSS for patients was 0.738 and 0.760, respectively. When we generated calibration curves, the nomograms were reasonably calibrated.
Conclusions
Derived NLR may be used in combination with conventional staging techniques and other clinicopathological parameters to improve the prediction of survival in patients with UTUC.



Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59:225–249
Raman JD, Scherr DS (2007) Management of patients with upper urinary tract transitional cell carcinoma. Nat Clin Pract Urol 4:432–443
Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E, The Upper Tract Urothelial Carcinoma Collaboration et al (2009) Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 115:1224–1233
Novara G, De Marco V, Gottardo F, Dalpiaz O, Bouygues V, Galfano A et al (2007) Independent predictors of cancer-specific survival in transitional cell carcinoma of the upper urinary tract: multi-institutional dataset from 3 European centers. Cancer 110:1715–1722
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Glen P, Jamieson NB, McMillan DC, Carter R, Imrie CW, McKay CJ (2006) Evaluation of an inflammation-based prognostic score in patients with inoperable pancreatic cancer. Pancreatology 6:450–453
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Maltoni M, Caraceni A, Brunelli C, Broeckaert B, Christakis N, Eychmueller S, Steering Committee of the European Association for Palliative Care et al (2005) Prognostic factors in advanced cancer patients: evidence-based clinical recommendations-a study by the Steering Committee of the European Association for Palliative Care. J Clin Oncol 23:6240–6248
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DSJ et al (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer 47:2633–2641
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F et al (2009) Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 197:466–472
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Gondo T, Nakashima J, Ohno Y, Choichiro O, Horiguchi Y, Namiki K et al (2012) Prognostic value of neutrophil-to-lymphocyte ratio and establishment of novel preoperative risk stratification model in bladder cancer patients treated with radical cystectomy. Urology 79:1085–1091
Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ (2012) A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer 107:695–699
Todenhöfer T, Renninger M, Schwentner C, Stenzl A, Gakis G (2012) A new prognostic model for cancer-specific survival after radical cystectomy including pretreatment thrombocytosis and standard pathological risk factors. BJU Int 110:E533–540
Hashimoto T, Ohno Y, Nakashima J, Gondo T, Ohori M, Tachibana M (2013) Clinical significance of preoperative peripheral blood neutrophil count in patients with non-metastatic upper urinary tract carcinoma. World J Urol 31:953–958
Lehmann J, Suttmann H, Kovac I, Hack M, Kamradt J, Siemer S et al (2007) Transitional cell carcinoma of the ureter: prognostic factors influencing progression and survival. Eur Urol 51:1281–1288
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ (2003) Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer 89:1028–1030
McMillan DC (2008) An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc 67:257–262
Kasymjanova G, MacDonald N, Agulnik JS, Cohen V, Pepe C, Kreisman H et al (2010) The predictive value of pre-treatment inflammatory markers in advanced non-small-cell lung cancer. Curr Oncol 17:52–58
Ku JH, Kim M, Choi WS, Kwak C, Kim HH (2014) Preoperative serum albumin as a prognostic factor in patients with upper urinary tract urothelial carcinoma. Int Braz J Urol 40:753–762
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Heagerty PJ, Lumley T, Pepe MS (2000) Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56:337–544
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30:1073–1081
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M (2007) The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 73:215–220
Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6:283–287
Ding PR, An X, Zhang RX, Fang YJ, Li LR, Chen G et al (2010) Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage IIA colon cancer. Int J Colorectal Dis 25:1427–1433
Hung HY, Chen JS, Yeh CY, Changchien C-R, Tang R, Hsieh P-S et al (2011) Effect of preoperative neutrophil-lymphocyte ratio on the surgical outcomes of stage II colon cancer patients who do not receive adjuvant chemotherapy. Int J Colorectal Dis 26:1059–1065
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12:223–226
Richards CH, Roxburgh CS, MacMillan MT, Isswiasi S, Robertson EG, Guthrie GK et al (2012) The relationships between body composition and the systemic inflammatory response in patients with primary operable colorectal cancer. PLoS ONE 7:e41883
Conflict of interest
The authors have no financial conflict of interests.
Ethical standard
The protocol of this study was approved by the Institutional Review Board of our institutions (Approval No. H1311-069-533). The need for informed consent was waived by the Institutional Review Board because of the retrospective design with minimal risk of harm to subjects. All personal identifiers were removed, and data were analyzed anonymously.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
See Table 4.
Appendix 2
See Table 5.
Appendix 3
See Fig. 4.
Time-dependent receiver operating characteristics curve analysis of the nomogram. Curve plots the area under the curve over time. Recurrence-free survival for the nomogram excluding (a) and including (b) derived NLR. Integrated area under the curve value was 0.718 (a) and 0.738 (b), respectively. Disease-specific survival for the nomogram excluding (c) and including (d) derived NLR. Integrated area under the curve value was 0.745 (a) and 0.760 (b), respectively
Appendix 4
See Fig. 5.
Appendix 5
See Table 6.
Appendix 6
See Table 7.
Rights and permissions
About this article
Cite this article
Kim, M., Moon, K.C., Choi, W.S. et al. Prognostic value of systemic inflammatory responses in patients with upper urinary tract urothelial carcinoma. World J Urol 33, 1439–1457 (2015). https://doi.org/10.1007/s00345-015-1484-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1484-9