Abstract
Background
To investigate the prognostic significance of the systemic immune-inflammation index (SII) for patients with upper tract urothelial carcinoma (UTUC) after radical nephroureterectomy (RNU) and develop nomogram models for predicting overall survival (OS), intravesical recurrence (IVR), and extra-urothelial recurrence (EUR).
Methods
We retrospectively studied the clinical and pathological features of 195 patients who underwent RNU for UTUC. All patients were randomly divided into a training cohort (99 cases) and a validation cohort (96 cases). The training cohort was used to develop nomogram models, and the models were validated by the validation cohort. The least absolute shrinkage and selection operator (LASSO) regression and Cox regression were performed to identify independent predictors. The concordance index (C-index), receiver operator characteristics (ROC) analysis, and calibration plot were used to evaluate the reliability of the models. The clinical utility compared with the pathological T stage was assessed using the net reclassification index (NRI), integrated discrimination improvement (IDI), and decision curve analysis (DCA).
Results
SII was an independent risk factor in predicting OS and EUR. The C-index values of the nomogram predicting OS, IVR, and EUR were 0.675, 0.702, and 0.756 in the training cohort and 0.715, 0.756, and 0.713 in the validation cohort. A high level of SII was correlated with the invasion of the mucosa, muscle layer of the ureter, nerves, vessels, and fat tissues.
Conclusion
We developed nomogram models to predict the OS, IVR, and EUR of UTUC patients. The efficacy of these models was substantiated through internal validation, demonstrating favorable discrimination, calibration, and clinical utility. A high level of SII was associated with both worse OS and shorter EUR-free survival.
Similar content being viewed by others
Background
Upper tract urothelial carcinoma (UTUC) accounts for 5–10% of urothelial carcinomas [1]. Though radical nephroureterectomy (RNU) with bladder cuff removal is the standard treatment of UTUC patients, the tumors were found to be invasive at diagnosis in 60% of cases [2]. The disease recurrence in the bladder or non-bladder sites is frequent [3]. Many studies have focused on the pre-, intra-, and postoperative prognostic factors of patients with UTUC after RNU [4,5,6,7]. According to the European Association of Urology (EAU) Guidelines on UTUC, template lymphadenectomy, and perioperative platinum-based combination chemotherapy should be considered in patients with high-risk tumors [2]. Enhancing comprehension of prognostic factors and constructing a predictive model can facilitate the identification of patients at high risk of recurrence, thereby necessitating the implementation of more rigorous therapeutic and monitoring interventions.
Preoperative prognostic factors encompass various variables such as patient age, tobacco usage, tumor focality, tumor location, grade, hydronephrosis, and inflammation-related indicators, among others [6]. However, the accuracy of tumor pathological features obtained through uroscopy is limited [8]. Furthermore, preoperative ureteroscopy has been identified as a risk factor for intravesical recurrence (IVR) and has a negative impact on the prognosis of patients with UTUC after RNU [9, 10]. Additionally, imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) pose challenges in detecting microscopic invasion and are inadequate for determining personalized treatment approaches [6, 11, 12].
Inflammation plays a contributing role in the initiation and advancement of various cancers [13]. Numerous inflammation- and immune-related factors have been identified as having prognostic value for oncological outcomes in patients with UTUC following RNU [7, 14], including the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR). Increased NLR, PLR, and LMR have been linked to a heightened risk of recurrence and poorer survival rates [15]. The systemic immune-inflammation index (SII), which is an integrated immune and inflammatory index derived from peripheral lymphocyte, neutrophil, and platelet counts, has been identified as an independent prognostic indicator in various cancer types such as gastric cancer, colorectal cancer, hepatocellular cancer, and lung cancer [16,17,18,19]. A meta-analysis has demonstrated that a higher SII value is significantly associated with poorer survival outcomes in urological cancers, including prostate cancer and urothelial carcinoma [20].
The predictive efficacy of SII in patients with UTUC after RNU has been assessed in several studies. These studies have reported that a high SII is an independent predictor of poorer recurrence-free survival (RFS), cancer-specific survival (CSS), and overall survival (OS) [15, 21]. Additionally, an elevated SII is associated with an increased risk of muscle-invasive and non-organ-confined disease following RNU [15, 21]. Moreover, the SII has been shown to be a significant prognostic factor for bladder recurrence [11]. However, the prognostic significance of SII in relation to extra-urothelial recurrence (EUR) remains unexplored, and the potential correlation between tumor status and SII has not been thoroughly examined. This study aims to assess the predictive value of SII for survival outcomes and recurrence in patients with UTUC, investigate the association between tumor status and SII, and construct a predictive model based on significant prognostic factors.
Methods
Patient selection
This retrospective study was approved by the Institutional Research Ethics Committee of China-Japan Friendship (2021–40-K24). Informed consent was obtained from all eligible participants in advance. We retrospectively collected the information of patients diagnosed with UTUC who received RNU treatment at our hospital from 2009 to 2020, and all patients’ details have been de-identified. We included the patients who meet the following criteria: (1) patients with UTUC confirmed pathologically, (2) patients with primary disease, (3) patients with unilateral onset, and (4) patients subject to RNU combined with cystic sleeve resection. Patients were excluded according to the following criteria: (1) patients with bilateral UTUC, (2) patients subject to no RNU combined with cystectomy, and (3) patients with metastatic uroepithelial carcinoma.
Follow-up and cohort definition
We monitored patients every 3 months during the first year after surgery, every 6 months through the third year, and once a year thereafter. Follow-up data included blood tests, cystoscopic examination, urinary system ultrasound, chest and abdomen CT, urine exfoliated cytology, and urography. Selective bone scan, PET/CT, or MRI were performed if clinically indicated. OS was defined as the time from the date of RNU to death from any cause. Intravesical recurrence-free survival (IVRFS) was defined as the time from the date of RNU to the date of the first IVR according to cystoscopic examination. Extraurothelial recurrence-free survival (EURFS) was defined as the time from the date of RNU to the date of the first EUR according to imaging examination. The patients were randomly divided into the training and validation cohorts with a ratio of 1:1 using the R function “createDataPartition.” The training set was utilized for the development of nomograms, determination of the cutoff value for SII, and serum aspartate transaminase/alanine transaminase (ALT/AST), as well as risk stratification. The findings derived from the training set were subsequently validated in the validation cohort.
Data collection
Sixteen variables were included: age, sex, history of hypertension, history of diabetes mellitus (DM), body mass index (BMI), tumor side, tumor location, tumor grade, pathological tumor stage, tumor size, SII, ALT/AST ratio, estimated glomerular filtration rate (eGFR), urine cytology, ureteroscopy, and presence of hydronephrosis. Pretreatment SII values were assessed within 30 days prior to RNU. SII was calculated as platelet count × neutrophil/lymphocyte count. The optimal SII cutoff value was defined by creating a time-dependent receiver operating characteristic (ROC) curve with OS as the endpoint to yield the highest Youden index value. The overall study population was divided into two separate SII groups (> 470 vs. ≤ 470) according to the optimal cutoff. The preoperative eGFR was calculated using the following formula: 186 (serum creatinine)^(–1.154)*(age)^(–0.203)*(0.742 if female). Patients with an eGFR lower than 60 ml/min/1.73 m2 were considered to have chronic kidney disease. Tumor stages were defined pathologically based on the American Joint Committee on Cancer (AJCC) Tumor, Node, Metastasis (TNM) classification (eighth edition). Tumor grades were defined using the 2008 World Health Organization (WHO) classification. The tumor location is marked according to the location of the dominant tumor. Positive urine cytology was defined as the presence of tumor cells or abnormal cells in preoperative samples. Conversely, negative urine cytology was defined as an evaluation that yielded negative results. The evaluation of all histopathological slides was conducted by the senior pathologist.
Statistical analysis
Predictive models were constructed through the utilization of Cox regression with the least absolute shrinkage and selection operator (LASSO) regression. In order to optimize parameter selection within the LASSO regression, a tenfold cross-validation was conducted. Subsequently, a multivariable Cox regression analysis was employed to ascertain independent risk factors, which were then integrated into the nomograms. Additionally, collinearity testing was conducted using the variance inflation factor (VIF), whereby a VIF value exceeding 4.0 was deemed indicative of multicollinearity. Variables exhibiting a VIF value surpassing 4.0 were consequently excluded from the model. The 1-/3-/5-year OS, IVRFS, and EURFS probabilities were estimated using the nomograms. The discriminations of the models were evaluated using concordance indexes (C-index) calculated by bootstrapping and time-dependent area under curve (AUC). Calibration curves were calculated to assess the predictive ability. We set time-dependent ROC curves with OS, IVRFS, and EVRFS as the endpoint, respectively, to define the optimal cutoff point for risk stratifications.
We expressed the categorical variables as the frequency (percentage). Some results were shown as interquartile ranges (IQRs). All variables were categorized using the cutoff set from time-dependent ROC or previous reports. The association of variables was assessed with the χ 2 test and Fisher’s exact test. The net reclassification index (NRI), integrated discrimination improvement (IDI), and decision curve analysis (DCA) were used for the evaluation of prediction improvement compared with prediction based on pathological tumor staging alone. All P values were two-tailed, and P < 0.05 was considered statistically significant. R software (Version 4.2.2) and IBM SPSS Statistics (Version 24) were utilized to complete all statistical analyses and figures.
Results
Characteristics of patients and disease
A cohort of 195 patients who met the specified inclusion and exclusion criteria were included in the study. Data on 16 pre- or peri-operative variables, tumor invasion, and the duration of overall survival, intravenous revascularization, and endovascular ureteral reimplantation were collected. The patients were randomly divided into training and validation groups in a 1:1 ratio. The median follow-up period was 43 months, with an IQR of 26.5–70.5 months. The clinical characteristics of all patients were summarized in Table 1. There were no significant differences observed in pre- and peri-operative and demographic parameters among the patients.
Variable screening
We first utilized LASSO Cox regression to screen possible prognostic factors (Figure S1). When the minimum lambda was 0.022, 0.034, and 0.043, 18, 12, and 8 potential predictors for OS, IVR, and EUR were screened out in the training cohort, respectively. Then, we established a multivariate Cox model to identify independent risk factors significantly affecting OS, IVRFS, or EURFS in patients with UTUC after RNU. Finally, we identified several independent risk factors for predicting OS, including BMI, gender, SII, and tumor stage (Table 2). Additionally, urine cytology, eGFR, and tumor stage were found to be independent risk factors for predicting IVR (Table S1), while BMI, gender, SII, hydronephrosis, and tumor stage were independent risk factors for EUR (Table S2).
Nomogram construction and validation
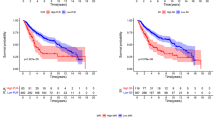
The independent risk factors above were incorporated to construct the nomograms to predict OS, IVR, and EUR in patients with UTUC after RNU. The impact of each factor on the clinical outcomes was explicitly listed in the nomograms. The cumulative risk scores, obtained by summing individual risk scores, were subsequently calculated. Notably, the total risk points for predicting OS in the patients included in this study ranged from 0 to 293.4 (Fig. 1). Patients in the present study had total risk points for predicting IVR ranging from 0 to 191.3 (Fig. 2). Patients had total risk points for predicting EUR ranging from 0 to 343.9 (Fig. 3). The discriminative value of the nomogram was evaluated using the concordance index. In the training cohort, the C-index value for predicting OS was 0.675, while in the validation cohort, it was 0.715. For predicting IVR, the C-index value was 0.702 in the training cohort and 0.756 in the validation cohort. Similarly, for predicting EUR, the C-index value was 0.752 in the training cohort and 0.713 in the validation cohort. Model calibration was visually assessed through calibration curves (Fig. 4), which indicated satisfactory calibration of the new model. In the training set, the 3-year AUC values for the nomogram’s predictions of OS, IVR, and EUR were 0.723, 0.676, and 0.802, respectively. Similarly, in the validation set, the 3-year AUC values for the nomogram’s predictions of OS, IVR, and EUR were 0.671, 0.648, and 0.668, respectively (Fig. 5). These findings indicated that our nomograms exhibit favorable discriminatory ability.
The calibration curves of the OS nomogram in the training cohort (A) and at the validation cohort (D). The calibration curves of the IVRFS nomogram in the training cohort (B) and at validation cohort (E). The calibration curves of the EURFS nomogram in the training cohort (C) and at the validation cohort (F)
Clinical application of the nomograms
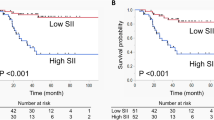
We also estimated the IDI and NRI to compare the accuracy between the nomograms and the AJCC criteria-based pathological tumor staging alone. Using the nomogram in the training cohort, the NRI for the 3-year OS was 0.065, and the IDI value for the 3-year OS was 0.086. The NRI for the 3-year IVR was 0.296, and the IDI value for the 3-year IVR was 0.106. The NRI for the 3-year EURFS was 0.38, and the IDI value was 0.173. These results were validated in the validation cohort. NRI and IDI revealed improvements in discrimination (Table 3). The DCA of the training set and the validation set are shown in Fig. 6. When a threshold probability ranges from threshold 1 to threshold 2, using the nomogram to predict OS, IVRFS, and EURFS can achieve more benefits than using the pathological tumor stage alone. Finally, risk stratification was performed by calculating with the nomogram. In the training and validation cohorts, respectively, patients were divided into two risk groups: low-risk (total points ≤ 193.4, 100, and 138.3, for OS, IVRFS, and EURFS prediction, respectively) and high-risk group (total points > 193.4, 100, and 138.3). The Kaplan–Meier curves showed perfect discrimination among the two risk groups in both training and validation sets (Figure S2).
SII level and tumor invasion
The correlation between SII level and other clinical, pathological factors was shown in Table 4. Our analysis revealed a significant correlation between a high SII level and invasion in the mucosa, muscular layer of the ureter, fat tissues, and neural and vascular invasion. However, no correlation was observed between SII level and invasion in the subepithelial layer of the ureter, renal sinus, pararenal area, ureteral ends, and lymph node.
Discussion
Our study revealed that a high SII was a notable unfavorable prognostic determinant for OS and EUR in patients with UTUC after RNU. While certain factors such as tumor stage, tumor grade, and surgical margins have been associated with poor survival outcomes, these are typically assessed postoperatively using pathological specimens. In contrast, blood-based inflammation biomarkers can be conveniently obtained prior to surgery and aid urologists in making optimal clinical decisions for individual patients.
Inflammation and immune responses are critical components of tumor genesis, proliferation, invasion, and metastasis [22]. Inflammation-related indicators including SII, NLR, PLR, and LMR can reflect the situation of systemic inflammatory response and have been demonstrated to show prognostic value in in various malignancies [23,24,25,26]. The inflammation, infection, and oncogene activation lead to the activation of transcription factors in tumors and stroma, which subsequently lead to the production of chemokines, cytokines, and prostaglandins and induce the recruitment of inflammatory cells [27]. The secretion of chemokines and cytokines in the circulation mediates alteration in distant sites and results in tumor-derived cytokines and growth factors secreted into the systemic circulation to mediate alteration in distant sites [13]. Through the production of growth factors (for example G-CSF and GM-CSF) and the production of inflammatory cytokines, including IL-6, IL-1β, and IL-17 (neutrophil diversity and plasticity in tumor progression and therapy), tumor cells and tumor niche regulate the development, maturation, and release from the bone marrow of neutrophils, which result in peripheral neutrophilia [28, 29].
Neutrophils have complex roles in tumor development and progression. The pro-tumor phenotype of tumor-associated neutrophils can support tumor growth via different mechanisms, including the promotion of genetic instability, tumor cell proliferation, angiogenesis, metastasis, and immunosuppression [30, 31]. High infiltration of tumor-associated neutrophils and peripheral neutrophilia has been reported to be associated with poor prognosis in many human tumors [32, 33]. It has also been reported that high NLR and increased peripheral blood neutrophil counts may be associated with a higher frequency of tumor-infiltrating neutrophils [34]. Peripheral neutrophils also contribute to tumor development, progression, and metastasis through a variety of mechanisms, including the promotion of angiogenesis, production of matrix metalloproteinases, and escorting of circulating tumor cells [35,36,37].
Platelets play an important role in tumor progression. Paracrine secretion of IL-6 from tumor cells stimulates the production of thrombopoietin (TPO), resulting in megakaryopoiesis and platelet genesis and leading to a status of thrombocytosis and hypercoagulability known as Trousseau’s syndrome [38, 39]. Platelets can directly or indirectly interact with tumor cells and increase tumor progression by promoting proliferation, resisting cell death, inducing angiogenesis, activating invasion, establishing pre-metastatic microhabitats, and evading immune detection [40]. Elevated platelet counts have been reported to be associated with increased cancer risk at several sites [41].
Numerous studies have reported associations between elevated platelet counts and decreased disease-specific survival rates across various types of cancer [42]. In the context of cancer immune surveillance and resistance, lymphocytes play a crucial role in impeding the proliferation and growth of tumor cells through cytotoxic cell death. Conversely, the presence of T lymphocytes within the tumor microenvironment has been consistently linked to improved prognoses, highlighting their significant anti-tumor functionality [43, 44]. Lymphocytes inhibit the proliferation and growth of tumor cells by cytotoxic cell death in cancer immune surveillance and resistance. In contrast, lymphocytes have an important anti-tumor function, and infiltration of T lymphocytes in the tumor microenvironment was known to be correlated with better prognosis [43, 44]. CD8 + T cells contribute to direct tumor cell lysis and the production of cytotoxic cytokines. CD4 + Th1 cells assist cytotoxic T lymphocytes and impress tumor progression by the production of cytokines (for example, IFN-γ), Th17 cells, and Treg cells function in the anti-tumor process by activating cytotoxic lymphocytes or suppression of inflammation [45]. To summarize, neutrophils, platelets, and lymphocytes are crucial components in inflammation and immunity related to cancer. In UTUC, multiple system inflammation and immune-related indexes based on these factors have been developed to predict the prognosis of patients after RNU, including NLR, PLR, and LMR[7, 46,47,48]. The SII, which incorporates the counts of neutrophils, platelets, and lymphocytes, offers a more comprehensive assessment of the host’s immune and inflammatory status compared to the aforementioned indicators [49].
For patients with UTUC after RNU, IVR and EUR can significantly decrease survival time. Therefore, the relative prediction model also aroused a great interest in recent years. To our knowledge, the present study is the first proposal to confirm that SII possesses predictive value for EUR among UTUC patients and construct a prediction model with SII included. In accordance with prior research, our findings indicated that urine cytology, eGFR, and tumor stage were independent prognostic factors for IVR [48]. Interestingly, SII was not associated with IVR from our results. Although Chen et al. reported elevated SII can predict bladder recurrence, some patients with a history of bladder cancer were included in their study [11]. We hypothesize that the observed disparity may be attributed to the heterogeneity of the study population, variations in baseline characteristics, inclusion of different variables, inadequate sample size, or statistical noise. Undoubtedly, further investigations involving larger sample sizes are imperative to establish reliable conclusions.
In addition, an examination was conducted to investigate the correlation between preoperative SII levels and invasion sites. The outcomes revealed a significant association between elevated SII levels and high tumor grade, as well as invasion in various anatomical locations including the mucosa, muscle, adipose tissue, and neural and vascular structures. These findings suggested a heightened invasiveness of tumors exhibiting elevated SII levels. Plausible mechanistic explanations for these observations involve tumor-induced inflammation and subsequent cytokine production, particularly IL-6 and IL-8, which are known to play a pivotal role in the epithelial-mesenchymal transition (EMT). Furthermore, the induction and maintenance of tumor EMT are facilitated by the presence of inflammation, thereby facilitating the advancement towards metastasis [50].
There are several limitations to the present study that should be acknowledged. Firstly, it is imperative to note that this study is retrospective and conducted within a single center, thus potentially limiting the generalizability of the findings due to the relatively small sample size. Secondly, the inclusion of only 11 patients with low-grade tumor grade necessitates further validation of the predictive capabilities of the models for clinical outcomes in patients with low tumor grade. Lastly, it is crucial to develop a more universally applicable threshold for SII, as the cutoff employed in this study may not be applicable across other studies.
Conclusion
Our study suggested that a high level of preoperative SII is associated with both worse OS and shorter EURFS in UTUC patients after RNU. We developed nomogram models for predicting the OS, IVR, and EUR of patients, respectively, and their discrimination, calibration, and clinical use were proved through internal validation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EUR:
-
Extraurothelial recurrence
- UTUC:
-
Upper tract urothelial carcinoma
- RUN:
-
Radical nephroureterectomy
- EAU:
-
European Association of Urology
- IVR:
-
Intravesical recurrence
- CT:
-
Computed tomography
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- LMR:
-
Lymphocyte-to-monocyte ratio
- SII:
-
Systemic immune-inflammation index
- RFS:
-
Recurrence-free survival
- CSS:
-
Cancer-specific survival
- OS:
-
Overall survival
- EUR:
-
Extraurothelial recurrence
- IVRFS:
-
Intravesical recurrence-free survival
- EURFS:
-
Extraurothelial recurrence-free survival
- ALT/AST:
-
Aspartate transaminase/alanine transaminase
- DM:
-
Diabetes mellitus
- BMI:
-
Body mass index
- eGFR:
-
Estimated glomerular filtration rate
- ROC:
-
Receiver operating characteristic
- AJCC:
-
American Joint Committee on Cancer
- TNM:
-
Tumor, node, metastasis
- WHO:
-
World Health Organization
- LASSO:
-
Least absolute shrinkage and selection operator
- VIF:
-
Variance inflation factor
- C-index:
-
Concordance indexes
- AUC:
-
Area under the curve
- IQRs:
-
Interquartile ranges
- NRI:
-
Net reclassification index
- IDI:
-
Integrated discrimination improvement
- DCA:
-
Decision curve analysis
- TPO:
-
Thrombopoietin
- EMT:
-
Epithelial-mesenchymal transition
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. https://doi.org/10.3322/caac.21551.
Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur Urol. 2021;79(1):62–79. https://doi.org/10.1016/j.eururo.2020.05.042.
Favaretto RL, Shariat SF, Chade DC, Godoy G, Adamy A, Kaag M, et al. The effect of tumor location on prognosis in patients treated with radical nephroureterectomy at Memorial Sloan-Kettering Cancer Center. Eur Urol. 2010;58(4):574–80. https://doi.org/10.1016/j.eururo.2010.07.003.
Margulis V, Youssef RF, Karakiewicz PI, Lotan Y, Wood CG, Zigeuner R, et al. Preoperative multivariable prognostic model for prediction of nonorgan confined urothelial carcinoma of the upper urinary tract. J Urol. 2010;184(2):453–8. https://doi.org/10.1016/j.juro.2010.03.142.
Simsir A, Sarsik B, Cureklibatir I, Sen S, Gunaydin G, Cal C. Prognostic factors for upper urinary tract urothelial carcinomas: stage, grade, and smoking status. Int Urol Nephrol. 2011;43(4):1039–45. https://doi.org/10.1007/s11255-011-9915-z.
Lughezzani G, Burger M, Margulis V, Matin SF, Novara G, Roupret M, et al. Prognostic factors in upper urinary tract urothelial carcinomas: a comprehensive review of the current literature. Eur Urol. 2012;62(1):100–14. https://doi.org/10.1016/j.eururo.2012.02.030.
Mori K, Janisch F, Mostafaei H, Lysenko I, Kimura S, Egawa S, Shariat SF. Prognostic value of preoperative blood-based biomarkers in upper tract urothelial carcinoma treated with nephroureterectomy: a systematic review and meta-analysis. Urol Oncol. 2020;38(5):315–33. https://doi.org/10.1016/j.urolonc.2020.01.015.
Margolin EJ, Matulay JT, Li G, Meng X, Chao B, Vijay V, et al. Discordance between ureteroscopic biopsy and final pathology for upper tract urothelial carcinoma. J Urol. 2018;199(6):1440–5. https://doi.org/10.1016/j.juro.2018.02.002.
Marchioni M, Primiceri G, Cindolo L, Hampton LJ, Grob MB, Guruli G, et al. Impact of diagnostic ureteroscopy on intravesical recurrence in patients undergoing radical nephroureterectomy for upper tract urothelial cancer: a systematic review and meta-analysis. BJU Int. 2017;120(3):313–9. https://doi.org/10.1111/bju.13935.
Yonese I, Ito M, Waseda Y, Kobayashi S, Toide M, Takazawa R, Koga F. Adverse prognostic impact of diagnostic ureterorenoscopy in a subset of patients with high-risk upper tract urothelial carcinoma treated with radical nephroureterectomy. Cancers (Basel). 2022;14(16). https://doi.org/10.3390/cancers14163962.
Chien TM, Li CC, Lu YM, Chou YH, Chang HW, Wu WJ. The predictive value of systemic immune-inflammation index on bladder recurrence on upper tract urothelial carcinoma outcomes after radical nephroureterectomy. J Clin Med. 2021;10(22). https://doi.org/10.3390/jcm10225273.
Honda Y, Nakamura Y, Teishima J, Goto K, Higaki T, Narita K, et al. Clinical staging of upper urinary tract urothelial carcinoma for T staging: review and pictorial essay. Int J Urol. 2019;26(11):1024–32. https://doi.org/10.1111/iju.14068.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. https://doi.org/10.1016/S1470-2045(14)70263-3.
Shao Y, Li W, Wang D, Wu B. Prognostic value of preoperative lymphocyte-related systemic inflammatory biomarkers in upper tract urothelial carcinoma patients treated with radical nephroureterectomy: a systematic review and meta-analysis. World J Surg Oncol. 2020;18(1):273. https://doi.org/10.1186/s12957-020-02048-7.
Jan HC, Yang WH, Ou CH. Combination of the preoperative systemic immune-inflammation index and monocyte-lymphocyte ratio as a novel prognostic factor in patients with upper-tract urothelial carcinoma. Ann Surg Oncol. 2019;26(2):669–84. https://doi.org/10.1245/s10434-018-6942-3.
Zhaojun X, Xiaobin C, Juan A, Jiaqi Y, Shuyun J, Tao L, et al. Correlation analysis between preoperative systemic immune inflammation index and prognosis of patients after radical gastric cancer surgery: based on propensity score matching method. World J Surg Oncol. 2022;20(1):1. https://doi.org/10.1186/s12957-021-02457-2.
Shi H, Jiang Y, Cao H, Zhu H, Chen B, Ji W. Nomogram based on systemic immune-inflammation index to predict overall survival in gastric cancer patients. Dis Markers. 2018;2018:1787424. https://doi.org/10.1155/2018/1787424.
Chen JH, Zhai ET, Yuan YJ, Wu KM, Xu JB, Peng JJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–72. https://doi.org/10.3748/wjg.v23.i34.6261.
Tong YS, Tan J, Zhou XL, Song YQ, Song YJ. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J Transl Med. 2017;15(1):221. https://doi.org/10.1186/s12967-017-1326-1.
Huang Y, Gao Y, Wu Y, Lin H. Prognostic value of systemic immune-inflammation index in patients with urologic cancers: a meta-analysis. Cancer Cell Int. 2020;20:499. https://doi.org/10.1186/s12935-020-01590-4.
Mori K, Resch I, Miura N, Laukhtina E, Schuettfort VM, Pradere B, et al. Prognostic role of the systemic immune-inflammation index in upper tract urothelial carcinoma treated with radical nephroureterectomy: results from a large multicenter international collaboration. Cancer Immunol Immunother. 2021;70(9):2641–50. https://doi.org/10.1007/s00262-021-02884-w.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. https://doi.org/10.1038/nature01322.
Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020;18(1):360. https://doi.org/10.1186/s12916-020-01817-1.
Yamamoto T, Kawada K, Obama K. Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int J Mol Sci. 2021;22(15). https://doi.org/10.3390/ijms22158002.
Huang H, Liu Q, Zhu L, Zhang Y, Lu X, Wu Y, Liu L. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer. Sci Rep. 2019;9(1):3284. https://doi.org/10.1038/s41598-019-39150-0.
Jiang Y, Xu D, Song H, Qiu B, Tian D, Li Z, et al. Inflammation and nutrition-based biomarkers in the prognosis of oesophageal cancer: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e048324. https://doi.org/10.1136/bmjopen-2020-048324.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44. https://doi.org/10.1038/nature07205.
Ocana A, Nieto-Jiménez C, Pandiella A, Templeton AJ. Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer. 2017;16(1):137. https://doi.org/10.1186/s12943-017-0707-7.
Ruka W, Rutkowski P, Kaminska J, Rysinska A, Steffen J. Alterations of routine blood tests in adult patients with soft tissue sarcomas: relationships to cytokine serum levels and prognostic significance. Ann Oncol. 2001;12(10):1423–32. https://doi.org/10.1023/a:1012527006566.
Jaillon S, Ponzetta A, Di Mitri D, Santoni A, Bonecchi R, Mantovani A. Neutrophil diversity and plasticity in tumour progression and therapy. Nat Rev Cancer. 2020;20(9):485–503. https://doi.org/10.1038/s41568-020-0281-y.
Que H, Fu Q, Lan T, Tian X, Wei X. Tumor-associated neutrophils and neutrophil-targeted cancer therapies. Biochim Biophys Acta Rev Cancer. 2022;1877(5):188762. https://doi.org/10.1016/j.bbcan.2022.188762.
Shaul ME, Fridlender ZG. Tumour-associated neutrophils in patients with cancer. Nat Rev Clin Oncol. 2019;16(10):601–20. https://doi.org/10.1038/s41571-019-0222-4.
Mitchell KG, Diao L, Karpinets T, Negrao MV, Tran HT, Parra ER, et al. Neutrophil expansion defines an immunoinhibitory peripheral and intratumoral inflammatory milieu in resected non-small cell lung cancer: a descriptive analysis of a prospectively immunoprofiled cohort. J Immunother Cancer. 2020;8(1). https://doi.org/10.1136/jitc-2019-000405.
Takakura K, Ito Z, Suka M, Kanai T, Matsumoto Y, Odahara S, et al. Comprehensive assessment of the prognosis of pancreatic cancer: peripheral blood neutrophil-lymphocyte ratio and immunohistochemical analyses of the tumour site. Scand J Gastroenterol. 2016;51(5):610–7. https://doi.org/10.3109/00365521.2015.1121515.
Tan KW, Chong SZ, Wong FH, Evrard M, Tan SM, Keeble J, et al. Neutrophils contribute to inflammatory lymphangiogenesis by increasing VEGF-A bioavailability and secreting VEGF-D. Blood. 2013;122(22):3666–77. https://doi.org/10.1182/blood-2012-11-466532.
Szczerba BM, Castro-Giner F, Vetter M, Krol I, Gkountela S, Landin J, et al. Neutrophils escort circulating tumour cells to enable cell cycle progression. Nature. 2019;566(7745):553–7. https://doi.org/10.1038/s41586-019-0915-y.
Bausch D, Pausch T, Krauss T, Hopt UT, Fernandez-del-Castillo C, Warshaw AL, et al. Neutrophil granulocyte derived MMP-9 is a VEGF independent functional component of the angiogenic switch in pancreatic ductal adenocarcinoma. Angiogenesis. 2011;14(3):235–43. https://doi.org/10.1007/s10456-011-9207-3.
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–8. https://doi.org/10.1056/NEJMoa1110352.
Haemmerle M, Stone RL, Menter DG, Afshar-Kharghan V, Sood AK. The platelet lifeline to cancer: challenges and opportunities. Cancer Cell. 2018;33(6):965–83. https://doi.org/10.1016/j.ccell.2018.03.002.
Franco AT, Corken A, Ware J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood. 2015;126(5):582–8. https://doi.org/10.1182/blood-2014-08-531582.
Giannakeas V, Kotsopoulos J, Cheung MC, Rosella L, Brooks JD, Lipscombe L, et al. Analysis of platelet count and new cancer diagnosis over a 10-year period. JAMA Netw Open. 2022;5(1):e2141633. https://doi.org/10.1001/jamanetworkopen.2021.41633.
Simanek R, Vormittag R, Ay C, Alguel G, Dunkler D, Schwarzinger I, et al. High platelet count associated with venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS). J Thromb Haemost. 2010;8(1):114–20. https://doi.org/10.1111/j.1538-7836.2009.03680.x.
van der Leun AM, Thommen DS, Schumacher TN. CD8+ T cell states in human cancer: insights from single-cell analysis. Nat Rev Cancer. 2020;20(4):218–32. https://doi.org/10.1038/s41568-019-0235-4.
Stanton SE, Disis ML. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J Immunother Cancer. 2016;4:59. https://doi.org/10.1186/s40425-016-0165-6.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99. https://doi.org/10.1016/j.cell.2010.01.025.
Stangl-Kremser J, Muto G, Grosso AA, Briganti A, Comperat E, Di Maida F, et al. The impact of lymphovascular invasion in patients treated with radical nephroureterectomy for upper tract urothelial carcinoma: an extensive updated systematic review and meta-analysis. Urol Oncol. 2022;40(6):243–61. https://doi.org/10.1016/j.urolonc.2022.01.014.
Kohada Y, Hayashi T, Goto K, Kobatake K, Abdi H, Honda Y, et al. Preoperative risk classification using neutrophil-lymphocyte ratio and hydronephrosis for upper tract urothelial carcinoma. Jpn J Clin Oncol. 2018;48(9):841–50. https://doi.org/10.1093/jjco/hyy084.
Vartolomei MD, Mathieu R, Margulis V, Karam JA, Rouprêt M, Lucca I, et al. Promising role of preoperative neutrophil-to-lymphocyte ratio in patients treated with radical nephroureterectomy. World J Urol. 2017;35(1):121–30. https://doi.org/10.1007/s00345-016-1848-9.
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–22. https://doi.org/10.1158/1078-0432.CCR-14-0442.
Dominguez C, David JM, Palena C. Epithelial-mesenchymal transition and inflammation at the site of the primary tumor. Semin Cancer Biol. 2017;47:177–84. https://doi.org/10.1016/j.semcancer.2017.08.002.
Acknowledgements
We sincerely thank Tom & Jerry for their spiritual support. We also gratefully acknowledge Fairy Sun for her help.
Funding
This study was supported by the Academy level project of China-Japan Friendship Hospital (2023-ZF-57).
Author information
Authors and Affiliations
Contributions
(I) Study design: Zhenshan Ding and Guan Zhang. (II) Data collection: Yangxuanyu Yan, Tao Huang, and Yuhao Liu; (III) Data analysis and interpretation: Haijie Chen, Yunfan Guan, and Zhenkai Luo; (IV) Manuscript writing: Yangxuanyu Yan, Zhenkai Luo, and Binbin Jiao; (V) Manuscript revision: Zhenkai Luo.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by China-Japan Friendship Hospital. The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
LASSO coefficient profiles of all variables predicting OS (A), 10-fold cross-validation for tuning parameter selection in the least LASSO model related to OS (B); LASSO coefficient profiles of the variables predicting IVRFS (C), 10-fold cross validation for tuning parameter selection in the least LASSO model related to IVRFS (D); LASSO coefficient profiles of the variables predicting EURFS (E), 10-fold cross validation for tuning parameter selection in the least LASSO model related to EURFS (F).
Additional file 2: Figure S2.
The Kaplan-Meier curves of OS nomogram in the training cohort (A) and validation cohort (D); The Kaplan-Meier curves of IVRFS nomogram in the training cohort (B) and validation cohort (E); The Kaplan-Meier curves of EURFS nomogram in the training cohort (C) and validation cohort (F).
Additional file 3: Table S1.
Univariate and multivariate analyses of predictive factors for intravesical recurrence.
Additional file 4: Table S2.
Univariate and multivariate analyses of predictive factors for extraurothelial recurrence.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, Z., Yan, Y., Jiao, B. et al. Prognostic value of the systemic immune-inflammation index in patients with upper tract urothelial carcinoma after radical nephroureterectomy. World J Surg Onc 21, 337 (2023). https://doi.org/10.1186/s12957-023-03225-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03225-0