Abstract
Purpose
To evaluate the perioperative safety and mid-term prognosis (≤12 months) of HydroSoft coils in treating ruptured aneurysms at the anterior circulation compared with bare platinum coils.
Materials and Methods
Patients with aneurysmal subarachnoid hemorrhages admitted to our hospital between January 2009 and March 2012 were retrospectively analyzed. According to strict inclusion and exclusion criteria, cases were selected and classified into two groups: In group A, HydroSoft coils were used as the primary filling coils (≥40 % of total coil length); in group B, only bare platinum coils were used. Cases in both groups were all treated with stent-assistance. A comparison between the two groups was performed for periprocedural complications as well as immediate and mid-term outcomes. The stents used included Enterprise, Neuroform, and Solitaire.
Results
Fifty-six aneurysms were in group A patients, and 68 aneurysms were in group B patients. Compared with group B, group A did not have increased incidence of complications but had greater packing attenuation (44.5 ± 8.8–29.8 ± 9.1 %, t = 2.577, P = 0.014) and increased initial complete occlusion rates (63–44 %, χ 2 = 4.161, P = 0.041). Radiologic follow-up were performed in 46 patients from group A and 51 patients from group B. Complete occlusion rates at follow-up were significantly greater in group A than in group B (89.1–70.6 %, χ 2 = 5.08, P = 0.043); the difference in recanalization rates were statistically insignificant between the groups (6.5–5.9 %, P = 1.000).
Conclusion
HydroSoft coils proved safe during the periprocedural period and provided greater initial complete occlusion rates, greater packing density, and better follow-up results compared with bare platinum coils.
Similar content being viewed by others
Introduction
Endovascular embolization has become an effective modality for the treatment of intracranial aneurysms; however, relatively greater recurrence rate remains one of the major handicaps of this technique [1]. Low packing density is among the various factors potentially affecting aneurysm recurrence [2–4]. To improve packing density, various modified coils have been used [5–7]. HydroCoils, which are hydrogel-coated coils, have shown the encouraging results of decreasing recurrence rates [8]. However, these coils are stiffer than the bare coils, which limits their use. To overcome the shortages of the HydroCoil, the HydroSoft coil was developed. It is constructed as a platinum coil with an inner core of hydrogel and a stretch resistant filament, thus providing relatively low stiffness. A multicenter study has shown that compared with pure platinum or other coated coils, embolization using HydroSoft improves initial occlusion rates and durability [5].
Thus, the present work was aimed at assessing the perioperative safety as well as initial and mid-term outcomes of stent-assisted HydroSoft coil embolization for the treatment of ruptured aneurysms at the anterior circulation compared with bare platinum coils.
Materials and Methods
Patient Selection
Consecutive patients with aneurysmal subarachnoid hemorrhages (aSAHs) admitted to our hospital between January 2009 and March 2012 were retrospectively analyzed. The inclusion criteria were as follows: (1) ruptured intracranial aneurysms situated in the anterior circulation; (2) stent-assisted coil embolization performed; (3) Hunt and Hess (H–H) grades of I to approximately III. The exclusion criteria were as follows: (1) embolization with modified coils other than HydroSoft; (2) HydroSoft coils used but not as the primary filling coil (<40 % of total coil length); (3) multiple aneurysms in which it was difficult to determine the “culprit one” that caused SAH; (4) staged embolization; (5) repeat embolization for recanalized or recurrent aneurysm; and (6) fusiform, infectious, traumatic, or dissecting aneurysms.
Cases were then classified into two groups: Group A, in which HydroSoft coils were used as the primary filling coils (≥40 % of the total coil length); and group B, in which only bare platinum coils were used. Forty percent of HydroSoft coil percentage length was set as the cut-off value because we regarded to be sufficient to cause a packing difference compared with bare coil according to our experience. The study was reviewed and approved by the Ethical Committee of our institute.
Embolization Procedure
All endovascular treatments were performed with the patients under general anesthesia. After systemic heparinization, a guiding catheter (Envoy; Cordis, Miami Lakes, FL) was placed in the internal carotid artery to obtain a stable position. A microguidewire was introduced distally to the aneurysm with the help of a suitable microcatheter. The stent was then placed, after which the aneurysm was catheterized by way of stent mesh and subsequently coiled in the same session; or, before deploying the stent, the embolization microcatheter was navigated into the aneurysm and the stent fully deployed after the completion of coil embolization or a coil basket covering the entire perimeter of the aneurysm was achieved. The goal for stent placement was to ensure the stent extended at least 5 mm past each side of the aneurysm neck. The appropriate size and length of the stent were chosen, and Enterprise stents (Codman Neurovascular, Raynham, MA), Neuroform stents (Boston Scientific, Natick, MA), and Solitaire stents (ev3, Irvine, CA) were used. Y-configuration deployment was excluded because our previous experience suggested a greater thromboembolic event rate with such; overlapping or stent-in-stent configuration was excluded because stents played a role as a flow diverter in this situation.
Regarding coil embolization, a series of coils of appropriate dimensions were selected. HydroSoft (Microvention Terumo, Aliso Viejo, CA), GDC (Boston Scientific, Fremont, CA), and Microplex (Microvention, Aliso Viejo, CA) were used. In the HydroSoft coils group, three-dimensional platinum coils were generally used to establish the initial framework in the aneurysm lumen and form a multiplanar structure for subsequent HydroSoft coil deposition; however, HydroSoft coils could be used as framing, filling, or finishing coils. In the bare platinum coils group, no modified coils were used. In each case, the objective of the procedure was angiographic occlusion of the aneurysm.
Anticoagulation and Antiplatelet Regimens
A loading dose of clopidogrel and aspirin (300 mg each) was administered orally or rectally at 2 h before stenting. From January 2009 to June 2010, all patients were maintained on aspirin (300 mg daily) and clopidogrel (75 mg daily) for 6 weeks followed by aspirin alone (100 mg daily), which was continued indefinitely. After June 2010, the initial 300-mg daily aspirin dose was decreased to 100 mg daily [9].
Initial Outcome Assessment and Follow-Up
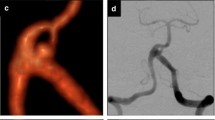
Digital subtraction angiography (DSA) results before and immediately after endovascular treatment were obtained. Immediate aneurysmal occlusion was defined by the modified Raymond-Roy classification as complete, residual neck, or residual sac [10].
The standard angiographic follow-up protocol consisted of a first angiography performed 1–6 months after the procedure and follow-up angiography at 6 or 12 months afterward. In patients with angiographic total occlusion, the follow-up was continued by magnetic resonance angiography on a yearly basis. For patients with angiographic recurrence, we continued follow-up by annual DSA. Follow-up data over 12 months were collected.
Follow-up results were further classified as stationary (contrast media filling increased <10 % or decreased <10 %), improved (contrast media filling decreased ≥10 %), or worsened (contrast media filling increased ≥10 %). A worsened result was regarded as recanalization. A blinded reviewer determined the occlusion status of each aneurysm on angiography. The packing density was defined as the ratio between the volume of coils inserted into the aneurysm and the aneurysm volume as has been described by previous studies [11]. Modified rankin scale (mRS) score was used to evaluate the clinical outcomes when patients were discharged and followed-up by rehospitalization, clinical visits, or phone calls.
Complications
Any periprocedural and postprocedural complications that were potential results of endovascular treatment was documented along with their clinical consequences, including the presence or absence of permanent disability.
Statistical Analysis
Continuous variables were described by means and SDs. Categorical variables were described by counts and percentages. P values for continuous variables were calculated using unpaired Student t test; P values for categorical variables were calculated using Fisher’s exact test or Pearson Chi square test. Statistical Package for the Social Sciences (version 18.0 for Windows; SPSS, Chicago, IL) was used to analyze the data. A P value of <0.05 was considered significant.
Results
Patients and Aneurysms
A total of 336 ruptured aneurysms were treated by stent-assisted coil embolization in our hospital from January 2009 to March 2012, among which 124 aneurysms were eligible for the study. These cases include the following: 56 ruptured aneurysms in 56 patients treated using HydroSoft coils (group A) and 68 ruptured aneurysms in 68 patients treated using only bare platinum coils (group B). Stents were typically used for wide-neck aneurysms (neck >4 mm and/or a dome-to-neck ratio <2) and for aneurysms that involved significant circumferential portions of the parent vessel. All cases were wide-necked aneurysms. Enterprise stents were used in 111 aneurysms, Neuroform stents in 8 aneurysms, and Solitaire stents in 5 aneurysms. Aneurysms included were located in a wide variety of locations in the anterior circulation. Patient demographics, aneurysm characteristics, and treatment information for these groups are listed in Table 1.
Complications
In group A, one MCA aneurysm ruptured during the intraprocedural period and caused SAH. The aneurysm ruptured after the first bare platinum coil placement; two HydroSoft coils were placed to obliterate the aneurysm, and decompressive craniectomy was then performed. The patient fully recovered without any neurologic deficit. Thromboembolism occurred in three cases; intravenous injection of tirofiban was given, which resulted in the disappearance of thrombi as seen on DSA. Postprocedural events included the following: one AchoAOphthalmic aneurysm rebleeding, which occurred 4 h after procedure and was treated by occlusion of the parent artery with Hydrogel-coated coils (Table 2).
In group B, two cases of thromboembolism occurred during surgery; one case of vasospasm occurred 8 days after surgery, and balloon dilation was performed. One 83-year-old female patient of pcom aneurysm aneurysm underwent SAH 3 days after the procedure and eventually died (Table 2). Nine patients underwent ventriculostomy or ventriculoperitoneal shunt placement (six in group A and three in group B), and there was no symptomatic catheter-related hemorrhage or radiographic hemorrhage was found. Compared with the bare platinum coil group, the use of HydroSoft coils did not increase complications, and no complications were definitively attributed to the use of HydroSoft coils.
Radiological Results
Initial complete occlusion rates between groups A and B was significantly different (63–44 %, χ 2 = 4.161, P = 0.041) (Tables 3, 4). The HydroSoft coil provided a packing attenuation of 44.5 ± 8.8 % compared with 29.8 ± 9.1 % using bare platinum coils, and the difference is significant (t = 2.577, P = 0.014).
In the HydroSoft coils group, radiologic follow-up data were available for 46 (82 %) aneurysms after coiling (mean interval 9.3 months). One patient in this group had aneurysmal rerupture and rebled 3 months after treatment; due to a lack of money, he did not receive any treatment and eventually died. Fifty-one (75 %) of the bare platinum coil-treated patients underwent follow-up angiography (mean interval 10.1 months). Detailed results are listed in Table 3.
Complete occlusion rates at follow-up were significantly greater in group A than in group B (89.1–70.6 %, χ 2 = 5.08, P = 0.043) (Table 4); three cases in group A and another three in group B showed worsened/recurring result at follow-up, and the difference in recanalization rates were statistically insignificant between the groups (6.5–5.9 %, P = 1.000).
In the respect of progressive occlusion of the initially incompletely occluded aneurysms, the difference between group A and B was insignificant (16/19–17/26, P = 0.191). In the neck remnant cases, 5/6 of group A and 6/8 of group B achieved improvement (P = 1.000); in the sac remnant cases, 11/13 in group A and 11/18 in group B achieved improvement (P = 0.238). Detailed data are listed in Table 3.
Clinical Results
In group A, mid-term follow-up was available for 53 of 56 patients with a mean of 11.2-month follow-up. One patient died at 3 months (Table 3). There were no or mild disability (mRS ≤ 2 [favorable outcome]) in 92.5 % (49 of 53) of patients. Three patients had moderately severe disability (mRS score 3 or 4).
In group B, long-term follow-up was available for 61 of 62 patients with a mean of 10.5-month follow-up. There were no or mild disability (mRS ≤ 2 [favorable outcome]) in 95.1 % (58 of 61) of patients. Two patients had moderately severe disability (mRS score 3 or 4).
Discussion
Despite the proven efficacy of endovascular coil embolization for the treatment of ruptured intracranial aneurysm reported in International Subarachnoid Aneurysm Trial [12], long-term durability still remains a major handicap of this treatment technique. Among the many factors leading to recurrence, initial low packing density and subtotal obliteration are regarded as prominent impacting factors. Greater packing density has been correlated with decreased coil compaction and theoretically decreases recurrence rates [13], but in clinical studies there have been conflicting results [2, 3, 14, 15].
Intracranial stents have a multifactorial favorable role in aneurysm embolization: It may enable dense coil mass packing [16, 17], change vascular morphology, induce intraaneurysmal flow modifications [18–22], and provide a structural basis for endothelialization [23, 24]. However, the use of stent-assisted coil embolization more commonly has been reserved for unruptured aneurysms in order to determine the difference between thromboembolic events and hemorrhagic events when treating acutely ruptured aneurysms compared with unruptured ones. Bodily et al. [25] reviewed 339 patients with acutely ruptured aneurysms treated by stent-assisted coiling, all of whom received dual-antiplatelet therapy during or immediately after surgery. They found an 8 % incidence of hemorrhagic complications and a 6 % incidence of thromboembolic events. In our study, rates of both kinds of complications were lower; this may due to three reasons. First, for patients who need a craniotomy for drainage of hematoma, the stent-assisted technique was generally avoided, and only a few external ventricular drainages were performed in our series, which increased the number of hemorrhagic complications [26]. Second, there were patients in our series who were admitted into our hospital >3 days after the onset of SAH. Last, only patients with H–H grade I to III were included in our series.
Hydrogel-coated coils were developed to increase packing density and promote endothelialization. They are platinum coils coated with polymeric gel composed of cross-linked acrylamide/sodium acrylate that absorbs water by diffusion in an optimal acid–base environment of blood, resulting in swelling to improve the volumetric occlusion of aneurysms [27]. Hydrogel-coated coils target dead space, which is present even in angiographically completely occluded aneurysm.
The precedent HydroCoils are generally used as filling coils rather than framing or finishing coils due to its stiffness. In a randomized controlled trial, HydroCoil Endovascular Aneurysm Occlusion and Packing Study, White et al. [8, 28] proved that HydroCoils can lower recurrent rates while not increasing periprocedural complications. Similar results were showed by Cloft et al. [29, 30].
The new design, HydroSoft, comprises a platinum coil with hydrogel inside. The new coil possesses lower stiffness while the coil-expansion decreases compared with the HydroCoil (0.013 vs. 0.022 inches). In addition, the HydroSoft coil does not require prehydration for softening, and there is virtually no time limitation for deployment after it is exposed to blood. HydroSoft is extremely gentle in treating smaller aneurysm or deployed as final coils near the neck of an aneurysm [31–34] and can complement the HydroCoil system for challenges, such as resistance or microcatheter instability.
We used HydroSoft coils both as framing, filling, and finishing coils in selected cases. A combined deployment of platinum coils and HydroSoft coils was performed in group A to maximize the benefits of each coil type to achieve better occlusion of aneurysms.
By using HydroSoft in embolization, Guo et al. [33] reported packing attenuation of 47 %, and Park et al. [5] reported packing attenuation of 42 %. Our study conforms to their results. Significantly greater aneurysm packing density was achieved with HydroSoft than bare coils, although the volumetric packing density calculation assumes full hydrogel expansion, which might not occur in vivo. Packing densities achieved in our study were lower than previously reported in studies using HydroCoils (45–85 %) [30, 33, 35, 36] and greater than what has been achieved with stent-assisted bare coils (36.59 %) [16].
Previous studies showed initial complete occlusion rates from 27–73 % [37–40] in treating aneurysms by stent-assisted coiling; compared with these studies, our results appeared moderate (63 % in group A and 44 % in group B). The cases included in the present series were all wide-necked and ruptured aneurysms, thus posing a challenge to angiographic occlusion. Although our neurointerventionists were experienced, angiographic occlusion was difficult to achieve in some aneurysms. For the HydroSoft-treated cases, due to the slow hydrogel expansion, greater packing density and initial complete occlusion rate were more easily achieved. Animal experiments have reported similar results [41].
In animal model studies, it is suggested that hydrogel increased neointima formation and thrombus organization and promote a healing reaction compared with bare platinum coils, suggesting a greater progressive occlusion rate [42, 43]. However, in our series, progressive occlusion rates (34 and 33 % of HydroSoft and bare coil, respectively) were lower than previous studies [44–46] and showed no significant difference among the two groups. The different results may due to anticoagulation therapies after embolization and different judgment criteria.
In our series, three patients had rebleeding. Although one of them recovered well after endovascular therapy; one remained with mild neurological deficit; and one eventually died from SAH without definite lesion. The one death may have been due to the patient’s advanced age and hypocoagulative status. This suggests that postprocedural rebleeding is highly dangerous and that dual-antiplatelet therapy should be carefully used for older patients, although it was safe for most patients.
Complete occlusion rates at follow-up were significantly greater in group A than in group B; however, the recurrence rates were not significantly different between the two groups. This suggests that although HydroSoft improved complete occlusion rate, the bare coil was also effective at 12-month follow-up. It is possible that HydroSoft would result in lower recurrence rates if the follow-up period lasted longer.
Conclusion
This is the first study that has focused on stent-assisted HydroSoft coils in treating ruptured aneurysms in the anterior circulation. In this study, the use of HydroSoft coils proved to be safe periprocedurally, provided greater packing density, and resulted in better initial and follow-up aneurysm obliteration compared with bare platinum coils.
References
Molyneux A, Kerr R, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group, Stratton I, Sandercock P, Clarke M et al (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurological clipping versus endovascular coiling in 2,143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet 11(6):304–314
Kawanabe Y, Sadato A, Taki W, Hashimoto N (2001) Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: correlation between coil packing density and coil compaction. Acta Neurochir (Wien) 143(5):415–451
Sluzewski M, van Rooij WJ, Slob MJ, Bescós JO, Slump CH, Wijnalda D (2004) Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology 231(3):653–658
Abdihalim M, Watanabe M, Chaudhry SA, Jagadeesan B, Suri MF, Qureshi AI (2013) Are coil compaction and aneurysmal growth two distinct etiologies leading to recurrence following endovascular treatment of intracranial aneurysm? J Neuroimaging doi. doi:10.1111/j.1552-6569.2012.00786.x
Park JH, Kang HS, Han MH, Jeon P, Yoo DS, Lee TH, Korean HydroSoft Registry Investigators (2011) Embolization of intracranial aneurysms with Hydrosoft coils: results of the Korean multicenter study. AJNR Am J Neuroradiol 32(9):1756–1761
Chun YI, Roh HG, Choe WJ, Cho J, Moon CT, Koh YC (2013) Tiny aneurysms treated with single coil: morphological comparison between bare platinum coil and matrix coil. Clin Neurol Neurosurg 115(5):529–534
Butteriss D, Gholkar A, Mitra D, Birchall D, Jayakrishnan V (2008) Single-center experience of cerecyte coils in the treatment of intracranial aneurysms: initial experience and early follow-up results. AJNR Am J Neuroradiol 29(1):53–56
White PM, Lewis SC, Gholkar A, Sellar RJ, Nahser H, Cognard CHELPS, Collaborators Trial et al (2011) Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet 377(9778):1655–1662
Huang QH, Wu YF, Shen J, Hong B, Yang PF, Xu Y et al (2013) Endovascular treatment of acutely ruptured, wide-necked anterior communicating artery aneurysms using the Enterprise stent. J Clin Neurosci 20(2):267–271
Roy D, Milot G, Raymond J (2011) Endovascular treatment of unruptured aneurysms. Stroke 32(9):1998–2004
Gaba RC, Ansari SA, Roy SS, Marden FA, Viana MA, Malisch TW (2006) Embolization of intracranial aneurysms with hydrogel-coated coils versus inert platinum coils: effects on packing density, coil length and quantity, procedure performance, cost, length of hospital stay, and durability of therapy. Stroke 37(6):14431450
Molyneux A, Kerr R, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group, Stratton I, Sandercock P, Clarke M et al (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurological clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis 11(6):304–314
Kadirvel R, Ding YH, Dai D, Lewis DA, Kallmes DF (2012) Proteomic analysis of aneurysm healing mechanism after coil embolization: comparison of dense packing with loose packing. AJNR Am J Neuroradiol 33(6):1177–1181
Goddard JK, Moran CJ, Cross DT 3rd, Derdeyn CP (2005) Absent relationship between the coil-embolization ratio in small aneurysms treated with a single detachable coil and outcomes. AJNR Am J Neuroradiol 26(8):1916–1920
Piotin M, Spelle L, Mounayer C, Salles-Rezende MT, Giansante-Abud D, Vanzin-Santos R et al (2007) Intracranial aneurysms: treatment with bare platinum coils—aneurysm packing, complex coils, and angiographic recurrence. Radiology 243(2):500–508
Izar B, Rai A, Raghuram K, Rotruck J, Carpenter J (2011) Comparison of devices used for stent-assisted coiling of intracranial aneurysms. PLoS One 6(9):e24875
Bendok BR, Parkinson RJ, Hage ZA, Adel JG, Gounis MJ (2007) The effect of vascular reconstruction device-assisted coiling on packing density, effective neck coverage, and angiographic outcome: an in vitro study. Neurosurgery 61(4):835–840 (discussion 840–841)
Gao B, Baharoglu MI, Cohen AD, Malek AM (2012) Stent-assisted coiling of intracranial bifurcation aneurysms leads to immediate and delayed intracranial vascular angle remodeling. AJNR Am J Neuroradiol 33(4):649–654
Gao B, Baharoglu MI, Malek AM (2013) Angular remodeling in single stent-assisted coiling displaces and attenuates the flow impingement zone at the neck of intracranial bifurcation aneurysms. Neurosurgery 72(5):739–748
King RM, Chueh JY, van der Bom IM, Silva CF, Carniato SL, Spilberg G et al (2012) The effect of intracranial stent implantation on the curvature of the cerebrovasculature. AJNR Am J Neuroradiol 33(9):1657–1662
Huang QH, Wu YF, Xu Y, Hong B, Zhang L, Liu JM (2011) Vascular geometry change because of endovascular stent placement for anterior communicating artery aneurysms. AJNR Am J Neuroradiol 32(9):1721–1725
Tateshima S, Tanishita K, Hakata Y, Tanoue SY, Viñuela F (2009) Alteration of intraaneurysmal hemodynamics by placement of a self-expandable stent. J Neurosurg 111(1):22–27
Wanke I, Forsting M (2008) Stents for intracranial wide-necked aneurysms: more than mechanical protection. Neuroradiology 50(12):991–998
Sedat J, Chau Y, Mondot L, Vargas J, Szapiro J, Lonjon M (2009) Endovascular occlusion of intracranial wide-necked aneurysms with stenting (neuroform) and coiling: mid-term and long-term results. Neuroradiology 51(6):401–409
Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF (2011) Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol 32(7):1232–1236
Kung DK, Policeni BA, Capuano AW, Rossen JD, Jabbour PM, Torner JC et al (2011) Risk of ventriculostomy-related hemorrhage in patients with acutely ruptured aneurysms treated using stent-assisted coiling. J Neurosurg 114(4):1021–1027
Kallmes DF, Fujiwara NH (2002) New expandable hydrogel-platinum coil hybrid device for aneurysm embolization. AJNR Am J Neuroradiol 23(9):1580–1588
White PM, Lewis SC, Nahser H, Sellar RJ, Goddard T, Gholkar A, HELPS Trial Collaboration (2008) HydroCoil endovascular aneurysm occlusion and packing study (HELPS Trial): procedural safety and operator-assessed efficacy results. AJNR Am J Neuroradiol 29(2):217–223
Cloft HJ (2006) HydroCoil for endovascular aneurysm occlusion (HEAL) study: periprocedural results. AJNR Am J Neuroradiol 27(2):289–292
Cloft HJ, HEAL Investigators (2007) HydroCoil for endovascular aneurysm occlusion (HEAL) study: 3–6 month angiographic follow-up results. AJNR Am J Neuroradiol 28(1):152–154
Tsumoto T, Niimi Y, Berenstein A (2009) Evaluation of the new HydroSoft coil in a canine model of bifurcation aneurysm laboratory investigation. J Neurosurg 111(1):11–16
Suri MF, Memon MZ, Qureshi AI (2008) Treatment of unruptured intracranial aneurysms using internally expanding coils. J Vasc Interv Neurol 1(2):42–45
Guo XB, Fan YM, Zhang JN (2011) HydroSoft coil versus HydroCoil for endovascular aneurysm occlusion study: a single center experience. Eur J Radiol 79(2):e42–e46
Waldau B, Turk AS 3rd, Yashar P, Khaldi A, Turner RD 4th, Chaudry MI et al (2012) Perioperative safety of Hydrosoft coils. J Neurointerv Surg 4(5):375–378
Cloft HJ, Kallmes DF (2004) Aneurysm packing with HydroCoil embolic system versus platinum coils: initial clinical experience. AJNR Am J Neuroradiol 25(1):60–62
Arthur AS, Wilson SA, Dixit S, Barr JD (2005) Hydrogel-coated coils for the treatment of cerebral aneurysms: preliminary results. Neurosurg Focus 18(2):E1
Mocco J, Snyder KV, Albuquerque FC, Bendok BR, Alan SB, Carpenter JS et al (2009) Treatment of intracranial aneurysms with the Enterprise stent: a multicenter registry. J Neurosurg 110(1):35–39
Lodi YM, Latorre JG, El-Zammar Z, Swarnkar A, Deshaies E, Fessler RD (2012) Stent assisted coiling of the ruptured wide necked intracranial aneurysm. J Neurointerv Surg 4(4):281–286
Tähtinen OI, Vanninen RL, Manninen HI, Rautio R, Haapanen A, Niskakangas T et al (2009) Wide-necked intracranial aneurysms: treatment with stent-assisted coil embolization during acute (<72 h) subarachnoid hemorrhage—Experience in 61 consecutive patients. Radiology 253(1):199–208
Klisch J, Clajus C, Sychra V, Eger C, Strasilla C, Rosahl S et al (2010) Coil embolization of anterior circulation aneurysms supported by the Solitaire™ AB Neurovascular Remodeling Device. Neuroradiology 52(5):349–359
Killer M, Hauser T, Wenger A, Richling B, Ladurner G (2009) Comparison of experimental aneurysms embolized with second-generation embolic devices and platinum coils. Acta Neurochir (Wien) 151:497–505
Killer M, Kallmes D, Jones R, Ding Y, Vestal M, Hauser T et al (2010) Long-term angiographic and histological results of a new hydrogel-containing filling coil in experimental rabbit aneurysms. Minim Invasive Neurosurg 53(3):97–105
Yoshino Y, Niimi Y, Song JK, Silane M, Berenstein A (2004) Endovascular treatment of intracranial aneurysms: comparative evaluation in a terminal bifurcation aneurysm model in dogs. J Neurosurg 101:996–1003
Yavuz K, Geyik S, Pamuk AG, Koc O, Saatci I, Cekirge HS (2007) Immediate and midterm follow-up results of using an electro-detachable, fully retrievable SOLO stent system in the endovascular coil occlusion of wide-necked cerebral aneurysms. J Neurosurg 107(1):49–55
Kurre W, Berkefeld J (2008) Materials and techniques for coiling of cerebral aneurysms: how much scientific evidence do we have? Neuroradiology 50(11):909–927
Lubicz B, Bandeira A, Bruneau M, Dewindt A, Balériaux D, De Witte O (2009) Stenting is improving and stabilizing anatomical results of coiled intracranial aneurysms. Neuroradiology 51(6):419–425
Conflict of interest
The authors declare that they have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, C., Yu, Y., Hong, B. et al. Stent-Assisted Coil Embolization for the Treatment of Ruptured Aneurysms at the Anterior Circulation: Comparison Between HydroSoft Coils and Bare Platinum Coils. Cardiovasc Intervent Radiol 37, 935–941 (2014). https://doi.org/10.1007/s00270-013-0769-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0769-x