Abstract
Aims/hypothesis
The relevance of the OGTT in predicting type 2 diabetes is unclear. We assessed the performance of 14 OGTT glucose traits in type 2 diabetes prediction.
Methods
We studied 2,603 and 2,386 Europeans from the Botnia study and Malmö Prevention Project (MPP) cohorts with baseline OGTT data. Over a follow-up period of 4.94 years and 23.5 years, 155 (5.95%) and 467 (19.57%) participants, respectively, developed type 2 diabetes. The main outcome was incident type 2 diabetes.
Results
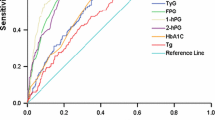
One-hour plasma glucose (1h-PG) was a fair/good predictor of incident type 2 diabetes in the Botnia study and MPP (AUC for receiver operating characteristic [AUCROC] 0.80 [0.77, 0.84] and 0.70 [0.68, 0.73]). 1h-PG alone outperformed the prediction model of multiple clinical risk factors (age, sex, BMI, family history of type 2 diabetes) in the Botnia study and MPP (AUCROC 0.75 [0.72, 0.79] and 0.67 [0.64, 0.70]). The same clinical risk factors added to 1h-PG modestly increased prediction for incident type 2 diabetes (Botnia, AUCROC 0.83 [0.80, 0.86]; MPP, AUCROC 0.74 [0.72, 0.77]). 1h-PG also outperformed HbA1c in predicting type 2 diabetes in the Botnia cohort. A 1h-PG value of 8.9 mmol/l and 8.4 mmol/l was the optimal cut-point for initial screening and selection of high-risk individuals in the Botnia study and MPP, respectively, and represented 30% and 37% of all participants in these cohorts. High-risk individuals had a substantially increased risk of incident type 2 diabetes (OR 8.0 [5.5, 11.6] and 3.8 [3.1, 4.7]) and captured 75% and 62% of all incident type 2 diabetes in the Botnia study and MPP.
Conclusions/interpretation
1h-PG is a valuable prediction tool for identifying adults at risk for future type 2 diabetes.

Similar content being viewed by others
Abbreviations
- 1h-PG:
-
1 h post-OGTT plasma glucose
- 2h-PG:
-
2 h post-OGTT plasma glucose
- AUCglucose :
-
AUC for OGTT glucose
- AUCROC :
-
AUC for ROC
- FPG:
-
Fasting plasma glucose
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- MPP:
-
Malmö Prevention Project
- NGT:
-
Normal glucose tolerance status
- NRI:
-
Net reclassification improvement
- PG:
-
Plasma glucose
- ROC:
-
Receiver operating characteristic
References
ADA Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (1997) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 20:1183–1197
Chen L, Magliano DJ, Zimmet PZ (2011) The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol 8:228–236
Fox CS, Coady S, Sorlie PD et al (2007) Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation 115:1544–1550
Vinik AI, Maser RE, Mitchell BD, Freeman R (2003) Diabetic autonomic neuropathy. Diabetes Care 26:1553–1579
Gaede P, Lund-Andersen H, Parving HH, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358:580–591
Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF (2003) Lifetime risk for diabetes mellitus in the United States. JAMA 290:1884–1890
Gang H, Hai Y, Dhingra R et al (2011) A novel hypoxia-inducible spliced variant of mitochondrial death gene Bnip3 promotes survival of ventricular myocytes. Circ Res 108:1084–1092
Dixon JB, Zimmet P, Alberti KG, Rubino F (2011) Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet Med 28:628–642
Merlotti C, Morabito A, Pontiroli AE (2014) Prevention of type 2 diabetes; a systematic review and meta-analysis of different intervention strategies. Diabetes Obes Metab 16:719–727
Tuomilehto J, Lindstrom J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Noble D, Mathur R, Dent T, Meads C, Greenhalgh T (2011) Risk models and scores for type 2 diabetes: systematic review. BMJ 343:d7163
Collins GS, de Groot JA, Dutton S et al (2014) External validation of multivariable prediction models: a systematic review of methodological conduct and reporting. BMC Med Res Methodol 14:40
Kodama S, Horikawa C, Fujihara K et al (2013) Use of high-normal levels of haemoglobin A(1C) and fasting plasma glucose for diabetes screening and for prediction: a meta-analysis. Diabetes Metab Res Rev 29:680–692
Abdul-Ghani MA, Lyssenko V, Tuomi T, DeFronzo RA, Groop L (2009) Fasting versus postload plasma glucose concentration and the risk for future type 2 diabetes: results from the Botnia Study. Diabetes Care 32:281–286
Rathmann W, Kowall B, Heier M et al (2010) Prediction models for incident type 2 diabetes mellitus in the older population: KORA S4/F4 cohort study. Diabet Med 27:1116–1123
Abdul-Ghani MA, Lyssenko V, Tuomi T, Defronzo RA, Groop L (2010) The shape of plasma glucose concentration curve during OGTT predicts future risk of type 2 diabetes. Diabetes Metab Res Rev 26:280–286
Tura A, Morbiducci U, Sbrignadello S, Winhofer Y, Pacini G, Kautzky-Willer A (2011) Shape of glucose, insulin, C-peptide curves during a 3-h oral glucose tolerance test: any relationship with the degree of glucose tolerance? Am J Physiol Regul Integr Comp Physiol 300:R941–R948
Kanauchi M, Kimura K, Kanauchi K, Saito Y (2005) Beta-cell function and insulin sensitivity contribute to the shape of plasma glucose curve during an oral glucose tolerance test in non-diabetic individuals. Int J Clin Pract 59:427–432
Tschritter O, Fritsche A, Shirkavand F, Machicao F, Haring H, Stumvoll M (2003) Assessing the shape of the glucose curve during an oral glucose tolerance test. Diabetes Care 26:1026–1033
Froslie KF, Roislien J, Qvigstad E et al (2013) Shape information from glucose curves: functional data analysis compared with traditional summary measures. BMC Med Res Methodol 13:6
Lyssenko V, Jonsson A, Almgren P et al (2008) Clinical risk factors, DNA variants, and the development of type 2 diabetes. N Engl J Med 359:2220–2232
Genter PM, Ipp E (1994) Accuracy of plasma glucose measurements in the hypoglycemic range. Diabetes Care 17:595–598
Sonowane M, Savory J, Cross RE, Heintges MG, Chester B (1976) Kinetic measurement of glucose with a centrifugal analyzer; hexokinase and glucose oxidase procedures compared. Clin Chem 22:1100–1101
(2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1): S62–S69
Rolandsson O, Hagg E, Nilsson M, Hallmans G, Mincheva-Nilsson L, Lernmark A (2001) Prediction of diabetes with body mass index, oral glucose tolerance test and islet cell autoantibodies in a regional population. J Intern Med 249:279–288
Abdul-Ghani MA, Williams K, DeFronzo RA, Stern M (2007) What is the best predictor of future type 2 diabetes? Diabetes Care 30:1544–1548
Song SH, Hardisty CA (2009) Early onset type 2 diabetes mellitus: a harbinger for complications in later years—clinical observation from a secondary care cohort. QJM 102:799–806
Almgren P, Lehtovirta M, Isomaa B et al (2011) Heritability and familiality of type 2 diabetes and related quantitative traits in the Botnia Study. Diabetologia 54:2811–2819
Manco M, Panunzi S, Macfarlane DP et al (2010) One-hour plasma glucose identifies insulin resistance and beta-cell dysfunction in individuals with normal glucose tolerance: cross-sectional data from the Relationship between Insulin Sensitivity and Cardiovascular Risk (RISC) study. Diabetes Care 33:2090–2097
Marini MA, Succurro E, Frontoni S et al (2012) Insulin sensitivity, β-cell function, and incretin effect in individuals with elevated 1-hour postload plasma glucose levels. Diabetes Care 35:868–872
Dupuis J, Langenberg C, Prokopenko I et al (2010) New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet 42:105–116
Saxena R, Hivert MF, Langenberg C et al (2010) Genetic variation in GIPR influences the glucose and insulin responses to an oral glucose challenge. Nat Genet 42:142–148
Stern MP, Williams K, Haffner SM (2002) Identification of persons at high risk for type 2 diabetes mellitus: do we need the oral glucose tolerance test? Ann Intern Med 136:575–581
Gerstein HC, Santaguida P, Raina P et al (2007) Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: a systematic overview and meta-analysis of prospective studies. Diabetes Res Clin Pract 78:305–312
Investigators DT, Gerstein HC, Yusuf S et al (2006) Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368:1096–1105
Knowler WC, Barrett-Connor E, Fowler SE et al (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Boyko EJ, Gerstein HC, Mohan V et al (2010) Effects of ethnicity on diabetes incidence and prevention: results of the Diabetes REduction Assessment with ramipril and rosiglitazone Medication (DREAM) trial. Diabet Med 27:1226–1232
Abdul-Ghani MA, Abdul-Ghani T, Ali N, DeFronzo RA (2008) One hour plasma glucose concentration and the metabolic syndrome identifies subjects at high risk for future type 2 diabetes. Diabetes Care 31:1650–1655
Matyka KA (2008) Type 2 diabetes in childhood: epidemiological and clinical aspects. Br Med Bull 86:59–75
Lijmer JG, Bossuyt PM (2009) Various randomized designs can be used to evaluate medical tests. J Clin Epidemiol 62:364–373
Robin X, Turck N, Hainard A et al (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinforma 12:77
Acknowledgements
We thank all the participants in the Botnia study and MPP.
Funding
The Botnia study was supported by grants from the Sigrid Juselius Foundation, Folkhälsan Research Foundation, Signe and Ane Gyllenberg Foundation, Swedish Cultural Foundation in Finland, Finnish Diabetes Research Foundation, Foundation for Life and Health in Finland, Finnish Medical Society, Paavo Nurmi Foundation, Helsinki University Central Hospital Research Foundation, Perklén Foundation, Ollqvist Foundation, Närpes Health Care Foundation and Ahokas Foundation. The study was also supported by the Municipal Heath Care Center and Hospital in Jakobstad and Health Care Centers in Vasa, Närpes and Korsholm. The skilful assistance of the Botnia Study Group is gratefully acknowledged.
The MPP was supported by grants from the Swedish Research Council (including Linné grant 31475113580), the Heart and Lung Foundation, the Diabetes Research Society, a Nordic Center of Excellence Grant in Disease Genetics, the Diabetes Program at the Lund University, the European Foundation for the Study of Diabetes, the Påhlsson Foundation, the Craaford Foundation, the Novo Nordisk Foundation, the European Network of Genomic and Genetic Epidemiology and the Wallenberg Foundation.
DM is supported by a Canada Research Chair.
Duality of interest
LG has been a consultant for and served on advisory boards for Tethys Bioscience, Sanofi-Aventis, GlaxoSmithKline, Eli Lilly, Merck and Novartis; also he has lectured at meetings organised by Novartis, GlaxoSmithKline and Sanofi-Aventis and received grant support from Novartis. VL received consulting fees from Tethys Bioscience. All other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Contribution statement
All authors have made substantial contributions to the manuscript. AA, DM, PA, JD, VL and LG contributed to the study concept and design. Acquisition of data was carried out by AA, DM, MA, BI, PN, TT, VL and LG. Data analyses and interpretation were performed by AA, DM, PA, MA, TT, VL and LG. The manuscript was drafted by AA and DM. The manuscript was critically reviewed for important intellectual content by PA, MA, JD, BI, PN, TT, VL and LG. All authors have approved the final draft for publication. DM and LG had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 59 kb)
ESM Table 1
(PDF 16 kb)
ESM Table 2
(PDF 21 kb)
ESM Table 3
(PDF 22 kb)
ESM Table 4
(PDF 20 kb)
ESM Table 5
(PDF 21 kb)
ESM Table 6
(PDF 27 kb)
ESM Table 7
(PDF 20 kb)
ESM Table 8
(PDF 21 kb)
ESM Table 9
(PDF 20 kb)
ESM Fig. 1
(PDF 20 kb)
ESM Fig. 2
(PDF 75 kb)
Rights and permissions
About this article
Cite this article
Alyass, A., Almgren, P., Akerlund, M. et al. Modelling of OGTT curve identifies 1 h plasma glucose level as a strong predictor of incident type 2 diabetes: results from two prospective cohorts. Diabetologia 58, 87–97 (2015). https://doi.org/10.1007/s00125-014-3390-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3390-x