Abstract
The world diabetes population quadrupled between 1980 and 2014 to 422 million and the enormous impact of Type 2 diabetes is recognised by the recent creation of national Type 2 diabetes prevention programmes. There is uncertainty about how to correctly risk stratify people for entry into prevention programmes, how combinations of multiple ‘at high risk’ glycemic categories predict outcome, and how the large recently defined ‘at risk’ population based on an elevated glycosylated haemoglobin (HbA1c) should be managed. We identified all 141,973 people at highest risk of diabetes in our population, and screened 10,000 of these with paired fasting plasma glucose and HbA1c for randomisation into a very large Type 2 diabetes prevention trial. Baseline discordance rate between highest risk categories was 45.6%, and 21.3–37.0% of highest risk glycaemic categories regressed to normality between paired baseline measurements (median 40 days apart). Accurate risk stratification using both fasting plasma glucose and HbA1c data, the use of paired baseline data, and awareness of diagnostic imprecision at diagnostic thresholds would avoid substantial overestimation of the true risk of Type 2 diabetes and the potential benefits (or otherwise) of intervention, in high risk subjects entering prevention trials and programmes.
Similar content being viewed by others
Introduction
The world diabetes population quadrupled between 1980 and 2014 to 422 million, with an estimated global prevalence in 2014 of 9.0% (95% credible interval 7.2–11.1%) in men and 7.9% (6.4–9.7%) in women1,2. The enormous impact of Type 2 diabetes is recognised by the calls for international focus on this issue1,3 and the need for more effective diabetes prevention strategies4,5.
The early Type 2 diabetes prevention trials showed a significant impact in reducing the risk of progression to Type 2 diabetes over 3 years in intensively managed research populations, largely with impaired glucose tolerance (IGT)6,7. Smaller, and more pragmatic studies, then tested the translatability of similar interventions8. Meta – analysis of these later studies suggested the probability of metabolic benefit in the short term, though with little evidence for immediate impact in Type 2 diabetes prevention, particularly in the less well studied (but very prevalent) high risk groups defined by HbA1c criteria8,9,10. The recent shift from glucose based to HbA1c based diagnostic criteria for diabetes has created new substantial populations with non - diabetic hyperglycemia (NDH; HbA1c ≥6.0%–<6.5%, ≥42–<48 mmol/mol), identified as at ‘high risk of Type 2 diabetes’, but where clinical trial evidence of diabetes prevention benefit from lifestyle intervention is very modest8,9,10,11. However, in 2015 the evidence base was seen as strong enough in the UK to mandate a national diabetes prevention programme in England, with entry to the short term intervention programme triggered largely by an NDH HbA1c diagnosis (HbA1c ≥6.0%–<6.5%, ≥42–<48 mmol/mol)12,13. Some concerns have been expressed in the UK about this ambitious national programme and this approach14,15. There is also a lack of current real world data on the prevalence, characteristics, and accessibility of the various at risk glycemic categories in a UK primary care population which makes planning more difficult12,13. The detailed, strongly evidence based, and multiagency USA national effort to develop an effective national programme for Type 2 diabetes prevention in the USA has also been described very recently16.
Entry to Type 2 diabetes prevention programmes in the UK is now commonly triggered by a single data point of an elevated HbA1c ≥6.0%–<6.5%, (≥42–<48 mmol/mol) (NDH). This approach largely ignores the rich longitudinal epidemiological data describing both HbA1c and fasting plasma glucose as continuous predictor variables for incident Type 2 diabetes risk, ignores the discordance between these glycemic categories, and ignores the substantial added value of combining both HbA1c and fasting plasma glucose in the accurate risk prediction for incident Type 2 diabetes17,18,19,20,21,22. This issue is important, as an estimated 10.7% of the adult population in England now have NDH23, and national guidance is that these patients (perhaps 4 million people in England) should now have targeted diet and lifestyle advice to reduce the risk of Type 2 diabetes 11. There may be capacity problems in delivering this.
To deliver effective intervention and diabetes prevention programmes, we need to understand the heterogeneity in the at risk populations entering prevention trials and programmes, and the opportunities for more accurate risk classification, risk stratification, in this and similar populations. The aim of this study is to describe the baseline characteristics and heterogeneity of the first 10,000 participants at ‘high risk of Type 2 diabetes’ in a UK population screened with paired fasting plasma glucose and HbA1c for randomisation into the largest current UK diabetes prevention trial.
Participants and Methods
The Norfolk Diabetes Prevention Study (NDPS; www.norfolkdiabetespreventionstudy.nhs.uk) is a 7 year programme funded by the UK National Institute of Health Research (NIHR RP-PG–0109–10013) and the full programme has been described elsewhere24. NDPS commenced in 2011 and reports in 2018. The programme tests the efficacy of an intensive 46 month lifestyle intervention in reducing the risk of transition to Type 2 diabetes for people with various ‘prediabetes’ or ‘non - diabetic hyperglycemia’ combinations11,17,18,23. The programme takes into account cost and workload pressures, and uses volunteer lay trainers with Type 2 diabetes to support the intervention, and randomises subjects with an elevated HbA1c (≥6%–<6.5%; ≥42–<48 mmol/mol) or impaired fasting glucose (IFG; fasting plasma glucose ≥5.6–<7.0 mmol/L) or combinations of these categories, but does not undertake oral glucose tolerance tests as a primary screening test to detect people with impaired glucose tolerance (IGT)11,17,18.
The classification and terminology for people at high risk of Type 2 diabetes based on a glucose or HbA1c that are elevated, but not into the diabetes diagnostic range, is complex and includes overlapping categories of prediabetes, impaired fasting glucose (IFG), impaired glucose tolerance (IGT), impaired glucose regulation (IGR), or non - diabetic hyperglycemia (NDH)11,17. In this paper, we restrict the term non - diabetic hyperglycemia (NDH) to participants with HbA1c ≥6%–<6.5% (≥42–<48 mmol/mol) and impaired fasting glucose (IFG) to participants with fasting plasma glucose of ≥6.1–<7.0 mmol/L or ≥5.6–<7.0 mmol/L depending on the classification criteria used11,17,18.
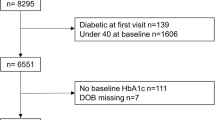
The programme identifies people at high risk of these categories through existing general practice (primary care) databases, and screens invited participants with paired baseline fasting plasma glucose and HbA1c to identify those suitable for randomisation. We contacted 194 general practices in Norfolk, Suffolk and North East Essex in England and by 1st March 2016, 135 practices were active collaborators, with a primary care population of 1.8 million. The NDPS used the existing NHS primary care electronic health record (EHR) software such as SystmOne or EMIS in each practice. All people without known diabetes in these practices were contacted if EHR data suggested they (a) were age ≥50 years with BMI ≥ 30 kg/m2 or (b) age ≥50 years and BMI ≥ 25 kg/m2 if there was also a recorded first degree family history of Type 2 diabetes, a history of coronary artery disease, or gestational diabetes or c) had any previous record of impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) or a fasting plasma glucose of ≥6.1–<7.0 mmol/L or (d) any previous record of HbA1c ≥6.0%–<6.5% (≥42–<48 mmol/mol) and a fasting glucose ≥5.6–<6.1 mmol/L. The mean prevalence of these categories on GP databases were 11% (a and b combined), 1.7% (c), and 2.7% (d) respectively. We contacted 141,973 people, inviting them to participate and 12,778 (9%) registered for participation, with the 10,000th consecutive participant completed on 1.3.16. After written informed consent, participants underwent venesection for fasting plasma glucose and HbA1c, and biometric and clinical data collection. Participants found to have any elevated fasting glucose or HbA1c in a randomisable category on initial testing were informed they had an abnormal (elevated) result and were invited to return for a repeat fasting plasma glucose and HbA1c measurement under the same conditions and at the same site, which was undertaken a median 40 days (interquartile range 27–69 days) later. Participants with a normal fasting plasma glucose (<5.6 mmol/l) or HbA1c <42 mmol/mol were not invited to return for a repeat sample. Randomisation into trial only occurred if paired baseline tests were concordant for glycemic category. In the early years of this programme (2011–2013), before changes to the new diagnostic criteria for diabetes based on HbA1c11,24 and changes in randomisation criteria in this programme, not all participants with an NDH level HbA1c, or a fasting plasma glucose ≥5.6–<6.1 mmol/L, had a repeat test as these categories (or combinations of categories) were not randomised into trials at the time. Fasting plasma glucose was measured by a hexokinase/G-6-PDH method (Architect c8000: Abbott Diagnostics, Maidenhead, UK). HbA1c was measured using Affinity high performance liquid chromatography (Hb9210: Menarini Diagnostics Ltd., Wokingham, UK). Weight, body mass index (BMI), body fat mass, visceral fat, and body fat percentage was measured using a Tanita body fat composition analyser (TANITA - Hoogoorddreef, 1101 BE, Amsterdam,The Netherlands. Model BC-420 MA). Data are shown as n (%) or mean and one standard deviation (SD). Probability for trend across all categories was calculated using linear regression, logistic regression, and Spearman correlation tests for continuous, binary and categorical variables respectively suing Stata software (Stata 14.1/SE. StataCorp. 2015. Stata Statistical Software,StataCorp LP). All subjects gave written informed consent to research participation after ethical review and approval from the National Research Ethics Service (NRES), Essex 1 Research Ethics Committee (10/H0301/55; 13.1.2011). All methods were performed in accordance with NRES permissions and after research governance approval form the sponsor organisation (Norfolk and Norwich University Hospital NHS Trust). In line with pre specified NDPS analysis plans, we undertook analysis of the first consecutive 10,000 patients screened.
Results
Clinical characteristics
The baseline characteristics of the first 10,000 screened participants are shown stratified by glycemic category (Tables 1 and 2), and by age and body mass index (Table 3).
2,172 (21.7%) participants had non - diabetic hyperglycemia (HbA1c ≥6.0%–<6.5%; ≥42–<48 mmol/mol). They were significantly older, and had significantly different anthropometric data, compared to those with a normal HbA1c <6. 0% (<42 mmol/mol) (Table 1).
967 (9.7%) had impaired fasting glucose (IFG; ≥6.1–<7.0 mmol/L), and 2,651 (26.5%) had the broader definition of impaired fasting glucose (fasting plasma glucose ≥5.6–<7.0 mmol/L; Table 2). The two IFG subcategories (fasting plasma glucose ≥5.6–≤6.0 mmol/L, or ≥6.1–<7.0 mmol/l) did not differ significantly from each other in any clinical or anthropometric data (Table 2).
The prevalence of participants with non - diabetic hyperglycemia (NDH; HbA1c ≥6%–<6.5%, ≥42–<48 mmol/mol) and/or IFG (fasting plasma glucose ≥6.1–<7.0 mmol/L) by age and BMI category is summarised (Table 3). This shows a combined population (n = 2,515; 25.2%) potentially eligible for randomisation into NDPS intervention trials. The commonest age group to attend for screening was 65–69 years old (n = 2,149; 21.5%), the commonest BMI group was 30–35 kg/m2 (n = 3, 813; 38.1%), and 29% of this combined age and BMI defined category had either NDH or IFG (Table 3).
Discordance between glycemic categories
The distribution of glycemic categories is shown in Table 4. Only 6,057 (60.6%) had an entirely normal combination of HbA1c <6.0% (<42 mmol/mol) and a fasting plasma glucose <5.6 mmol/L. Only 487 (4.9%) of this population had both NDH (HbA1c ≥ 6.0%–<6.5%; ≥42–<48 mmol/mol) and IFG (fasting plasma glucose ≥6.1–<7.0 mmol/L) on first screening (Table 4).
There was substantial discordance between glycemic categories (Tables 4–6) as 1,274 of the 2,651 participants (48.1%) with impaired fasting glucose (fasting plasma glucose ≥5.6 to <7.0 mmol/L) had a normal HbA1c (<6.0%,; <42 mmol/mol), and 306 of 967 participants (31.6%) with impaired fasting glucose (fasting plasma glucose ≥6.1–<7.0 mmol/L) had a normal HbA1c (<6. 0%; <42 mmol/mol). In addition, 990 of the 2,172 participants (45.6%) with NDH (HbA1c ≥ 6.0%–<6.5%, >42–<48 mmol/mol) had a normal fasting glucose (<5.6 mmol/L).
Screen detected Type 2 diabetes
The prevalence of screen detected Type 2 diabetes is shown (Tables 1 and 2).
Reproducibility of glycemic category at repeat confirmatory baseline sampling (Tables 5–8)
Of these 10,000 participants, 2,483 (24.8%) were eligible for a repeat fasting plasma glucose and HbA1c as a confirmatory baseline test prior to randomisation into an intervention trials.
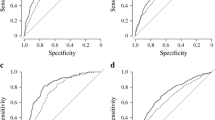
After a median 40 days later (interquartile range 27–69 days) and prior to any programme intervention, repeat baseline confirmatory testing showed that 36.1% of 950 participants with IFG (fasting plasma glucose ≥6.1–<7.0 mmol/L) now recorded a fasting plasma glucose of <6.1 mmol/L (Table 5). In addition, 21.3% of 1,463 participants with NDH (HbA1c ≥ 6.0%–<6.5%, ≥42–<48 mmol/mol) now recorded a normal HbA1c (<6%, <42 mmol/mol) on repeat baseline testing (Table 6).
At the same baseline sampling interval, participants with newly detected Type 2 diabetes at first testing, 39% of 251 participants with Type 2 diabetes based on fasting plasma glucose ≥7.0 mmol/L, and 21.1% of 394 participants with Type 2 diabetes based on HbA1c 6.5% (≥48 mmol/L) now recorded a non - diabetes range repeat measurement (Tables 5 and 6).
A small proportion of participants with NDH (HbA1c ≥ 6%–<6.5%, ≥42–<48 mmol/mol) or IFG (fasting plasma glucose ≥6.1–<7.0 mmol/L) at first baseline measurement recorded a diabetes range repeat baseline measurement (7.1% and 11.9% respectively; Tables 5 and 6).
The biochemical differences between subgroups who apparently regressed, progressed, or remained in the same glycemic category between paired baseline samples are shown (Tables 7 and 8). There were highly significant differences in mean HbA1c and fasting plasma glucose at first baseline sampling between these categories, with the ‘regression’ groups having significantly lower mean plasma glucose and HbA1c than ‘progression’ group (Tables 7 and 8).
Predictability of concordance in baseline results for an initially abnormal (42–47 mmol/mol) HbA1c
In the population with NDH, the probability of regression to a normal HbA1c result on repeat baseline testing was highly dependent on the initial HbA1c value (Table 9). For those with an initial HbA1c of 42 mmol/mol, 40.5% (95% CI 35.6–45.6) regressed to a normal baseline result, compared to 1.1% (95% CI 0–6.1) for those with an initial HbA1c of 47 mmol/mol. Participants with an NDH HbA1c of 45, 46, or 47 mmol/mol all had a >90% chance of having a concordant NDH HbA1c on repeat baseline testing. For those below this value (42, 43, or 44 mmol/mol), subcategorising by fasting plasma glucose data at baseline gave added value in predicting NDH HbA1c concordance. For example, although 40.5% (95% CI 35.6–45.6) of those an initial HbA1c of 42 mmol/mol regressed to normal on repeat baseline testing, this value was only 17% in those with an additionally elevated fasting plasma glucose (6.1–6.9 mmol/l), but 57% in those with an additionally normal fasting plasma glucose (4.5–4.9 mmol/l).
Discussion
There are two principal findings relevant to normal clinical practice and clinical prevention programmes in these data.
Firstly, we found that the NDH population (HbA1c ≥ 6.0%–<6.5%; ≥42–<48 mmol/mol), were very heterogenous with a very high rate of discordance between high risk glycemic categories. Nearly half of the high risk NDH subjects (now the dominant high risk glycemic category in current clinical practice in many countries), had a completely normal fasting plasma glucose (<5.6 mmol/L) and would be at much lower risk of Type 2 diabetes than the smaller group with two combined high risk categories. This heterogeneity has been described in cross sectional and epidemiological studies, but not in the context of a mass population screening programme for risk stratification and entry to a very large diabetes prevention trial.
Secondly, we found that about one - quarter of the population with a biochemical high risk glycemic category (NDH or IFG) recorded a normal result on repeat baseline measurement a median 40 days later, making it difficult to give participants an accurate risk estimate and correct randomisation pathway. This reinforces the need for paired baseline concordant data before giving a diagnosis of NDH. For NDH participants with an HbA1c of 45–47 mmol/mol inclusive, there was a more than 90% likelihood of a repeat baseline result also showing NDH range HbA1c and this allows confidence in correct diagnosis and risk categorisation for these subjects. For NDH participants with HbA1c of 42–44 mmol/mol, there is a high rate of regression to normal on repeat baseline testing, and subcategorization by fasting plasma glucose data allows more accurate risk stratification and diagnosis. The groups that regressed to normal between baseline testing also had a significantly lower mean HbA1c and fasting plasma glucose, closer to the lower diagnostic threshold, than those that did not regress. These data suggest clinicians need to be more aware of the diagnostic imprecision of a single data point close to these thresholds, and the need to avoid a lifelong misdiagnosis.
These are novel observations in the context of stratifying for entry into a diabetes prevention trial or clinical prevention programme, and have significant implication for clinical practice.These data suggest the majority of people with NDH entering clinical prevention programmes are at much lower risk than assumed as they also have a normal fasting glucose, or regress to normal within days of testing. These data are relevant to primary care clinicians and planners, as an estimated 10.7% of the adult population in England now have NDH23 and UK national guidance is that all of these patients (perhaps 4 million people in England) should have targeted diet and lifestyle advice to reduce the risk of Type 2 diabetes11. It remains unclear who will deliver this and where clinical resources are limited it seem sensible to identify those at genuinely highest risk using paired baseline data and both fasting glucose and HbA1c who are most likely to benefit from an intervention. This approach to risk assessment is similar to that used in mild hypertension or dyslipidaemia, with the use of multiple variables and repeat measurements to determine intervention and possible benefit. This additional glucose categorisation also appears to have cardiovascular risk assessment benefits in this population25. This approach may also have value in capacity planning for other national prevention initiatives16.
The diagnostic cut point of HbA1c ≥6.5% (≥48 mmol/mol) for diabetes is supplanting glucose based criteria11,17,18. This policy shift generates a new large high risk population with HbA1c >6%–<6.5% (≥42–<48 mmol/mol)11,18, categorised as ‘high risk’ for type 2 diabetes and eligible for intensive lifestyle intervention11. There is little trial outcome data for diabetes prevention benefit in this large ‘high risk’ population with an isolated elevated HbA1c and a normal fasting plasma glucose, and yet this is the largest population entering the NHS England national prevention programme, although other national models use a range of glycemic and biometric entry points16. Treating this entire population23 as a homogenous group ignores the rich epidemiological data describing the added value of further risk stratification using both HbA1c and fasting glucose in predicting Type 2 diabetes incidence, and the discordance between the various ‘at risk’ categories. The sub categorisation of the ‘high risk’ NDH population with HbA1c ≥6.0%–<6.5% (≥42 to <48 mmol/mol) by fasting glucose identifies subgroups at very different absolute and relative risks of Type 2 diabetes6,7,17. The presence of a normal fasting plasma in the ‘high risk’ population with HbA1c ≥6.0%–<6.5% (≥42–<48 mmol/mol) identifies a subgroup at a lower annual risk of progression to Type 2 diabetes, at perhaps only 1–2.5%19,20,21,22, while the combination of a ‘high risk’ HbA1c ≥6%–<6.5% (≥42–<48 mmol/mol) and an elevated fasting plasma glucose identifies a subgroup at a much higher relative and absolute risk of incident type 2 diabetes17,18,19,20,21,22. This suggests a difference in progression rates of between perhaps 4.5% over 3 years for those with NDH and a normal fasting plasma glucose, and perhaps up to 24% for those with NDH and an elevated fasting plasma glucose17,18,19,20,21,22. As the absolute and relative risk of Type 2 diabetes in NDH can be so much better defined with an additional fasting glucose data, it seems clinically sensible to make a more accurate risk estimate by using additional fasting glucose data, and focussing on highest risk NDH groups, rather than a blanket application of an intervention dose in all subjects.
We found a high proportion (21.3%) of participants with NDH had a normal HbA1c result (<6%, <42 mmol/mol) on repeat baseline testing, and 36.1% with IFG (6.1–6.9 mmol/L) had a fasting plasma glucose <6.1 mmol/L after a median 40 days, and before any trial intervention. This very rapid short term regression is a relatively novel observation in a clinical prevention trial, and raises questions about the using a single glycemic data point for entry to prevention programmes, and how to interpret later clinical end points if many participants in fact had regressed to normal within weeks of first measurement. This observation may in part reflect self - intervention and lifestyle changes triggered by a first abnormal result26, or some regression to the mean. Groups that showed very short term regression or progression were characterised by a mean HbA1c or fasting plasma glucose closer to relevant diagnostic thresholds, and these changes may also reflect normal assay variance across this threshold. Regression of an abnormal glucose category to normal after very many years follow up (with or without an intervention), is well described27,28,29,30, but not very short term regression of an abnormal baseline HbA1c or fasting plasma glucose data to normal for subjects entering a prevention trial or programme, beforeintervention. This means that as well as one half of the NDH patients having a normal fasting glucose about one quarter also return to normal after a few days on repeat testing. It is not possible to assume that those who regress to normal are still at the same high risk, as persistently abnormal glucose categories have a higher predictive value for Type 2 diabetes than isolated measurements that regress31,32. However, the true risk of Type 2 diabetes or adverse cardiovascular outcomes experienced by this unusual population with discordant baseline results remains to be seen, and will be available with very long term follow up and accurate outcome data planned after the end of the programme in 2018. These data also show clearly the diagnostic value in the current policy of using paired concordant baseline data in diagnosing diabetes as only 78.9% of those with screen detected Type 2 diabetes (≥6.5%, ≥48 mmol/L) had a diabetes range HbA1c a median of 40 days later.
Biochemical measurements for diagnosis or monitoring such as HbA1c need to be interpreted with an understanding of Uncertainty of Measurement (UoM), which includes the Total Analytical Error (TAE) and Biological Variation. Components of TAE are the analytical imprecision and bias of the method, and Sigma-Metrics (SM) provides a benchmark on which a process can be characterised and incorporates both imprecision and bias and the SM targets for HbA1c have been published33. The methods used in NDPS conform to quality standards and methods standardised to the International Federation of Clinical Chemistry and Laboratory Medicine Reference measurement procedure, and the analytical imprecision has been shown to be <3% CV and within-individual biological variation is relatively small compared to the between-person variation34,35 in people without diabetes. Based on UoM, a change of >4 mmol/mol in measured HbA1c reflects a true change in glycemic category and a difference of 6.0% to 6.5% (42 to 48 mmol/mol) in a repeat measurement may simply be accounted for by UoM. This uncertainty needs to be acknowledged when categorizing participants, and reinforces the value of paired confirmatory data for glycemic categorization particularly for participants with results close to a diagnostic threshold. In addition, there are less commonly acknowledged contributions of lifestyle and genetic variance to glycation and HbA1c variability (independent of glycemic profiles)36, as are the effects of aging related impairment in insulin release and advanced glycation end products (AGE) on insulin sensitivity37,38,39.
One strength of this study is that these 10,000 subjects were drawn from a large ‘at risk of Type 2 diabetes’ population identified on routine primary care databases, using the simplest of database search terms (age, BMI and/or glycaemic data). This approach is easily translatable to most primary care systems, and is similar both to approaches used in many case finding prevention trials and to the NHS England national diabetes prevention programme. The population studied are also relatively homogenous in terms of age banding and ethnicity, and all biochemical and biometric measurements were undertaken in the same laboratory, and by a small number of trained observers. Although the 10,000 subjects described in this study are drawn from a larger approached sample, it is not possible to comment on any differences between the consented 10,000 and those who did not respond to initial contact. This population is a self - selecting sample to some degree therefore, although likely to be similar to the sort of participants who would self - select to participate in any clinical prevention programme or diet and lifestyle diabetes prevention programme, and has validity in terms of populations entering prevention programmes. The data in this paper can not necessarily be translated to other populations with different ethnicities or identified through other screening strategies, although the suggested approach to correct risk stratification should be applied to all populations. We are unable to be clearer on the mechanisms behind our novel observation of short term regression to normality in NDH after 40 days at baseline, and before any entry into the trial intervention. If this regression was apparent with only a few days between paired baseline measurements this would makes it more likely to be related to UoM in assay measurements, rather than participants making changes in lifestyle between paired baseline measurements, but the interval between paired results was a median 40 days. One further limitation of this study is that we have only paired baseline data for entry to trial, and not at the several interval testing time points during 40 month follow up, so we are not aware if this short term regression to normality in paired samples is also apparent in HbA1c and glucose data collected at interval (non - end point) tests – clearly if this was the case, it would have very major implications for accurate end point determination in both prevention trials and programmes.
These current data suggest very many people entering national prevention programmes or trials based solely on a single elevated HbA1c are in fact at much lower risk than is assumed. Risk categorization using both fasting plasma glucose and HbA1c data, the use of paired baseline data prior to entry into clinical or research programmes, and awareness of diagnostic imprecision would mitigate some of these difficulties, and avoid overestimation of risk and a lifelong misdiagnosis. This policy would also allow a more focussed risk estimation to identify those truly at highest risk of Type 2 diabetes, and most likely to benefit from intervention. These data add to the literature on the over diagnosis of risk (with associated stigma and increased anxiety) and overstatement of potential benefit, particularly in populations withisolated NDH where trial evidence of diabetes prevention benefit form lifestyle intervention is modest14,15,39.
References
NCD Risk Factor Collaboration [NCD-RisC]. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. Lancet 387, 1513–1530 (2016).
Public Health England. Diabetes prevalence model (APHO) http://www.yhpho.org.uk/resource/view.aspx?RID = 81090 (accessed March 12, 2015).
World Health Organisation Global action plan for the prevention and control of non - communicable diseases 2013–2020. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1 (2013).
Comment. Reducing global diabetes burden by implementing solutions and identifying gaps: a Lancet Commission. Lancet 387, 1494–95. (2016)
Editorial. Beat diabetes: an urgent call for global action. Lancet 387, 1483 (2016).
Schwarz, P. E., Greaves, C. E., Lindstrom, J., Yates, T. & Davies, M. J. Nonpharmacological interventions for the prevention of Type 2 diabetes. Nat. Rev Endocrinol 8, 363–373 (2012).
Gillies, C. L. et al. Pharmacological and lifestyle interventions to prevent or delay Type 2 diabetes in people with impaired glucose tolerance: systematic review and meta – analysis. BMJ 334, 299–304 (2007).
Dunkley, A. J. et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: a systematic review and meta-analysis. Diabetes Care 37, 922–933 (2014).
Mudaliar, U. et al. Cardiometabolic risk factor changes observed in Diabetes Prevention Programs in US Settings: A Systematic Review and Metaanalysis. PLOS Medicine 13, 1–17 (2016).
Sattar, N., Logue, J. & Preiss, D. Research digest: weight loss to prevent and treat diabetes. Lancet Diabetes and Endocrinology 4, 817 (2016).
National Institute for Health and Clinical Excellence. Public health draft guidance. Preventing type 2 diabetes: risk identification and interventions for individuals at high risk. National Institute for Health and Clinical Excellence, London; Available from https://www.nice.org.uk/guidance/ph38 (2012).
Maruthappu, M., Sood, H. & Keogh, B. Radically upgrading diabetes prevention in England. Lancet Diabetes and Endocrinology 3, 312–313 (2015).
Torjesen, I. NHS England rolls out world’s first national diabetes prevention programme. BMJ 352, i1669 (2016).
Barry, E., Roberts, S., Finer, S., Vijayaraghavan, S. & Greenhalgh, T. Time to question the NHS diabetes prevention programme. BMJ 351, h4717 (2015).
Barry, E. et al. Efficacy and effectiveness of screen and treat policies in the prevention of type 2 diabetes. BMJ 356, i6538 (2017).
Ely, E. K. et al. National effort to prevent Type 2 diabetes: Participant – level evaluation of CDCs national diabetes prevention programme. Diabetes Care 40, 1331–1341 (2017).
Forouhi, N. et al. The threshold for diagnosing impaired fasting glucose: a position statement by the European Diabetes Epidemiology Group. Diabetologia 49, 822–827 (2006).
Morris, D. H. et al. Progression rates from HbA1c 6.0–6.4% and other prediabetes definitions to type 2 diabetes: a meta-analysis. Diabetologia 56, 1489–1493 (2013).
Chamnan, P. et al. Incidence of Type 2 diabetes using proposed HbA1c diagnostic criteria in the European prospective investigation of cancer – Norfolk cohort: implications for preventive strategies. Diabetes Care 34, 950–956 (2011).
Lipska, K. J. et al. Elevated HbA1c and fasting plasma glucose in predicting diabetes incidence among older adults: are two better than one? Diabetes Care 36, 3923–3929 (2013).
Heianza Y. et al. HbA1c 5·7–6·4% and impaired fasting plasma glucose for diagnosis of prediabetes and risk of progression to diabetes in Japan (TOPICS 3): a longitudinal cohort study. Lancet 378–385 (2011).
Shottker, B., Raum, E. & Rothenbacher, D. Prognostic value of HbA1c and fasting plasma glucose for incident diabetes and implications for screening. Eur J Epidemiology 26, 779–787 (2011).
National Cardiovascular Intelligence Network, “NHS Diabetes Prevention Programme (NHS DPP) Non-diabetic hyperglycemia. About Public Health England,” London; www.gov.uk/phe (2015).
Pascale, M. et al. The Norfolk Diabetes Prevention Study [NDPS]: a 46 month multi - centre, randomised, controlled parallel group trial of a lifestyle intervention [with or without additional support from lay lifestyle mentors with Type 2 diabetes] to prevent transition to Type 2 diabetes in high risk groups with non - diabetic hyperglycemia, or impaired fasting glucose. BMC Public Health. 17, 31, https://doi.org/10.1186/s12889-016-3929-5 (2017).
Giráldez-García, C. et al. Cardiometabolic Risk Profiles in Patients With Impaired Fasting Glucose and/or Hemoglobin A1c 5.7% to 6.4%: Evidence for a Gradient According to Diagnostic Criteria: The PREDAPS Study. Medicine (Baltimore). 94, e1935 (2015).
Youngs, W., Gillibrand, W. P. & Phillips, S. The impact of a prediabetes diagnosis on behaviour change: an integrative literature review. Practical Diabetes 33, 5–6 (2016).
Sasaki, A., Suzuki, T. & Horiuchi, N. Development of diabetes in Japanese subjects with impaired glucose tolerance: a seven year follow up study. Diabetologia 22, 154–157 (1982).
Morsiani, M. et al. Pavels dynamic screening for diabetes type 2.: 14 years results in a district of northern Italy. Med Interne 23, 13–17 (1985).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. Diabetes Prevention Program Research Group. N. Engl. J Med 346, 393–403 (2002).
Forouhi, N. G., Luan, J., Hennings, S. & Wareham, N. J. Incidence of Type 2 diabetes in England and its association with baseline impaired fasting glucose: the Ely study 1990–2000. Diabet Med 24, 200–207 (2007).
Inoue, K., Inoue, M., Matsumoto, M. & Akimoto, K. Persistent fasting hyperglycemia is more predictive of type 2 diabetes than transient fasting hyperglycemia. Diabetic Med 29, 75–81 (2012).
Li, G. et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 371, 1783–1789 (2008).
Weykamp, C. et al. IFCC Task Force on Implementation of HbA1c Standardization. Investigation of 2 models to set and evaluate quality targets for HbA1c: biological variation and sigma-metrics. Clin Chem. 61, 752–759 (2015).
John, W. G. et al. Multicentre evaluation of the Premier Hb9210 HbA1c analyser. Clin Chem Lab Med. 53, 319–327 (2015).
Lenters-Westra, E., Røraas, T., Schindhelm, R. K., Slingerland, R. J. & Sandberg, S. Biological variation of Hemoglobin A1c: consequences for the diagnosis of diabetes mellitus. Clinical Chemistry 60, 1570–1572 (2014).
Jansen, H. et al. Determinants of HbA1c in nondiabetic Dutch adults: genetic loci and clinical and lifestyle parameters, and their interactions in the Lifelines Cohort Study. J Intern Med 273, 283–293 (2013).
Santulli, G. et al. Age related impairment in insulin release: the essential role of B(2) adrenergic receptor. Diabetes 61, 692–701 (2012).
Cassese, A. et al. In skeletal muscle, advanced glycation end products (AGEs) inhibit insulin action and induce the formation of multi molecular complexes including the receptor for AGEs. J Biol Chem 283, 36088–99 (2008).
Yudkin J. S. & Montori V. M. The epidemic of pre-diabetes: the medicine and the politics. BMJ 349, g4485. Erratum in: BMJ. 2014;349: g4683 (2014).
Acknowledgements
We would like to acknowledge the contribution of Aliceon Blair, Andrew Goldson, Sara Auckland, Debbie Thompson and Sarah Wilson in delivering this programme. This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Reference Number RP – PG − 0109 − 10013). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Additional funding came from the NIHR Clinical Research Network (Eastern) and the Norfolk and Norwich University Hospital NHS Trust. The funding source(s) had no role in data collection, writing or any version of this manuscript. We are grateful to the NIHR CRN for supporting this programme. This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Reference Number RP – PG − 0109−10013). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
M.J.S. took the lead in writing this paper, and all revisions, designed the programme, and is C.I. for the NDPS programme and guarantor for this paper. T.E.-S. undertook data analysis of completed dataset, and helped draft and revise the paper, M.O.B. helped design the original programme and helped draft and revise the paper, A.C. drafted the statistical analysis plan for the whole programme, is trial statistician, undertook statistical analysis of the full dataset, and helped draft and revise the paper, K.K.D. helped design the original programme and helped draft and revise the paper, C.F. helped with data collection, programme infrastructure and accrual, and helped draft and revise the paper, A.H. helped design the original programme and helped draft and revise the paper, W.G.J. helped design the original programme and helped draft and revise the paper, G.R. helped with programme structure and delivery and helped draft and revise the paper, L.S. undertook initial drafts and data analysis of this paper, J.T. helped design the original programme and helped draft and revise the paper, M.P. is NDPS programme manager and helped deliver the programme, and helped draft and revise the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sampson, M., Elwell-Sutton, T., Bachmann, M.O. et al. Discordance in glycemic categories and regression to normality at baseline in 10,000 people in a Type 2 diabetes prevention trial. Sci Rep 8, 6240 (2018). https://doi.org/10.1038/s41598-018-24662-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-24662-y
- Springer Nature Limited