Abstract
Aims/hypothesis
Serum potassium has been found to be a significant predictor of diabetes risk, but the effect of dietary potassium on diabetes risk is not clear. We sought to determine if dietary potassium is associated with risk of incident type 2 diabetes in young adults.
Methods
We used data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Potassium intake was measured by (1) an average of three 24 h urinary potassium collections at the 5-year study visit, and (2) the CARDIA dietary assessment instrument at baseline. Incident type 2 diabetes cases were ascertained on the basis of use of diabetes medication and laboratory measurements. Analyses were adjusted for relevant confounders including intake of fruit and vegetables and other dietary factors.
Results
Of 1,066 participants with urinary potassium measurements, 99 (9.3%) developed diabetes over 15 years of follow-up. In multivariate models, adults in the lowest urinary potassium quintile were more than twice as likely to develop diabetes as their counterparts in the highest quintile (HR 2.45; 95% CI 1.08, 5.59). Of 4,754 participants with dietary history measurements, 373 (7.8%) developed diabetes over 20 years of follow-up. In multivariate models, African-Americans had a significantly increased risk of diabetes with lower potassium intake, which was not found in whites.
Conclusions/interpretation
Low dietary potassium is associated with increased risk of incident diabetes in African-Americans. Randomised clinical trials are needed to determine if potassium supplementation, from either dietary or pharmacological sources, could reduce the risk of diabetes, particularly in higher-risk populations.
Similar content being viewed by others
Introduction
The association between lower serum potassium and increased type 2 diabetes risk in the context of thiazide diuretic use has been well studied [1–3]. Recent studies have also found that lower serum potassium was associated with higher risk of diabetes independently of thiazide diuretic use [4, 5]. These studies raise the question of whether low dietary potassium contributes to the development of diabetes. Results of previous studies evaluating the association between dietary potassium intake and diabetes risk have been mixed [5–7]. These studies have used different populations, primarily white [6, 7], middle-aged populations [5–7], and have used different methods of measuring potassium intake, including diet histories [5, 6] and 24 h urinary potassium measurements [7]. Studies in younger adults, in whom diabetes prevention should ideally be focused, have not been performed. Also, studies using and comparing data from both diet histories and urinary excretion have not been carried out.
We hypothesised that low dietary potassium—as assessed by either 24 h urinary potassium or diet history—would be an independent predictor of incident diabetes in young adults. To test this hypothesis, we analysed data from the Coronary Artery Risk Development in Young Adults (CARDIA) Study (ClinicalTrials.gov NCT00005130), which measured 24 h urinary potassium in a subgroup of participants at the year 5 examination and dietary potassium intake with a detailed diet questionnaire in the entire cohort at the year 0 examination.
Methods
The CARDIA Study was designed to examine risk factors associated with development of cardiovascular disease in young adults. Baseline data from this prospective cohort study included 5,115 participants: men and women, African-American and white, between the ages of 18 and 30 years, recruited from four communities in the USA in 1985, with follow-up visits every 2–5 years for approximately 20 years [8]. This full cohort was used for our analyses using dietary potassium intake based on diet history as the main exposure. Of the full cohort, 24 h urine collections were collected on 3 consecutive days in a subset of 30% of study participants selected by sex/race group. This sub-cohort was used for analyses using urinary potassium as the main exposure. Institutional review boards at each of the participating institutions approved the study.
Exclusions
Of the 1,105 sub-study participants who were recruited to collect three consecutive 24 h urine specimens, we excluded five for whom all urinary potassium measures were missing, and 14 for whom urine collections were deemed by the study to be problematic because of an indeterminate length of collection. We excluded participants with prevalent diabetes at the time of the 24 h urine collections (1990 visit) as defined by use of diabetes medication or a fasting glucose ≥6.99 mmol/l (126 mg/dl) (n = 15). We further excluded participants with missing data (n = 4) or transgender sex (n = 1).
In analyses based on the entire cohort of 5,115 and using dietary potassium intake as the exposure, we excluded participants with prevalent diabetes at baseline (1985 visit), based on use of diabetes medication or fasting glucose ≥6.99 mmol/l (126 mg/dl) (n = 34), and those who did not attend any follow-up examinations (n = 186) or in whom diabetes status could not be determined (n = 2). We also excluded participants with extremes of energy intake (<2,510 kJ/day [<600 kcal/day] or >25,100 kJ/day [>6,000 kcal/day] for women, and <3,350 kJ/day (<800 kcal/day) or >33,470 kJ/day [>8,000 kcal/day] for men) (n = 124), those with missing information on other variables at baseline (n = 13), and those who had transgender sex (n = 2).
Incident type 2 diabetes mellitus
We identified incident cases of diabetes if any of the following conditions were met: (1) use of diabetes medication (assessed at every visit); (2) a fasting blood glucose level of ≥6.99 mmol/l (126 mg/dl) (measured at visits in 1992, 1995, 2000, 2005); (3) 2 h post-challenge glucose ≥11.1 mmol/l (200 mg/dl) (performed at the 1995 and 2005 visits); and/or (4) a HbA1c ≥6.5% (48 mmol/mol) (assessed at the 2005 visit). Serum glucose was measured at year 0 using the hexokinase ultraviolet method by the American Bio-Science Laboratories (Van Nuys, CA, USA) and at years 7, 10, 15 and 20 using hexokinase coupled to glucose-6-phosphate dehydrogenase by Linco Research (St Louis, MO, USA). HbA1c samples were sent to the University of Minnesota (Minneapolis, MN, USA) and were measured using the Tosoh G7 high-performance liquid chromatography instrument.
Urinary and dietary potassium
Participants selected to participate in the sub-cohort study received instructions regarding the collection of three consecutive 24 h urine specimens and were given all the materials for collections. Urinary potassium samples were sent to the American Health Foundation and were analysed using potentiometric methods on a Kodak Ektachem 400. A urinary potassium concentration was determined for each participant by averaging their measurements from the three collections. Two urinary potassium concentrations that were implausibly high were recoded as missing. If one measurement was missing, then the two available measurements were averaged (n = 149); if two were missing, then the single available measurement was used instead of a mean (n = 28).
Dietary potassium intake (mg/day) was assessed at the baseline visit (1985) in the entire cohort and subsequently in the 1992 and 2005 visits. A nutritionist administered a quantitative food frequency diet survey to participants with over 700 items, which was based on the Western Electric Study. This survey examined participants’ diet history in depth, reviewing participants’ food intake history over a reference period of the preceding month [9, 10]. In our primary analyses, we used data on dietary potassium intake from the baseline (year 0) examination. In sensitivity analyses, we averaged the dietary potassium measurement from the 1985 and 1992 visits.
Covariates
Other covariates used in this study were measured at year 0 and year 5. Covariates examined include average of three 24 h urinary creatinine measures (for analyses using urinary potassium only), age, sex, race, BMI, family history of diabetes, systolic blood pressure (average of second and third measurements), physical activity level, and education level. Diet variables included energy intake and intake of sweetened beverages, saturated fat and dietary fibre, all of which were derived from the same quantitative food frequency diet survey as was used for dietary potassium intake, and were included for analyses using dietary potassium only. All covariates were from the baseline visit for the respective analyses, i.e. 1990 (year 5) for analyses using urinary potassium and 1985 (year 0) for analyses using dietary potassium.
For measurements of systolic blood pressure, participants rested for 5 min in a quiet room, after which blood pressure was measured three times at 1 min intervals using a random-zero cuff sphygmomanometer. The average of the second and third readings was used in the analyses. Height and weight were measured with the participant wearing light clothing and no shoes. BMI was computed as weight (kg) divided by height (m) squared. Age, sex, race, years of education, smoking status and number of cigarettes smoked per day, and family history of diabetes were self-reported. Alcohol intake (ml/day) was computed from self-reported frequency of beer, wine and liquor consumed per week [11]. A physical activity score was computed from the CARDIA Physical Activity History, a modified version of the Minnesota Leisure Time Activity Questionnaire [12]. Urinary creatinine was measured with colorimetric methods by the American Health Foundation, and analyses were performed on a Kodak Ektachem 400. Intake of sweetened beverages was calculated as the sum of intake of sweetened soft drinks, sweetened fruit drinks, sweetened tea and sweetened coffee, the amount of which were all derived from the quantitative food frequency diet survey described above.
Statistical analysis
Distributions of dietary potassium intake and urinary potassium were approximately normal. We compared baseline characteristics of participants by race as well as by category of urinary potassium or dietary potassium intake using Student’s t tests, one-way ANOVA, or χ2 tests. We used Cox proportional hazards regression with forward selection modelling to assess the associations between either urinary potassium or dietary potassium intake with the risk of incident diabetes, using the highest quintile of urinary or dietary potassium as the reference group. We assessed statistical interactions of the main exposures with sex and race. Tests of significance were two-tailed with an α level of 0.05. We performed all analyses using SAS, version 9.2 (SAS Institute, Cary, NC, USA).
Sensitivity analyses were performed to assess the robustness of our findings for both urinary and dietary potassium analyses. Smoking and alcohol consumption were added as covariates to the models for both analyses. We categorised age, BMI, education and hypertension status, rather than using continuous variables in models for both analyses. For both analyses, we excluded participants taking diuretics at any of the examinations, as use of diuretics may affect participants’ diet and urinary excretion of potassium. For dietary analyses, we included potassium supplements with the dietary potassium intake from the 1985 visit as the main exposure. We averaged the dietary potassium intake measures from both the 1985 and 1992 visits to create an ‘averaged baseline’ for follow-up through 2005 to attempt to take into account some of the variability that can occur with dietary intake patterns of our nutrient of interest. The correlation of diet history of potassium intake at the baseline visit with urinary potassium at the year 5 visit was calculated, in the sub-cohort that had both measurements. Finally, in order to determine whether or not the effect of dietary potassium on diabetes risk was a reflection of intake of fruit and vegetables, we included total daily intake of fruit and vegetables in the model, derived from the quantitative food frequency diet survey described above using the highest quintile as the reference group.
Results
Urinary potassium analyses
We included 1,066 participants in the analyses of urinary potassium and risk of incident diabetes. The mean (SD) age, BMI and urinary potassium level of all included participants were 30 (3.6) years, 26.9 (6.4) kg/m2 and 55.0 (23.5) mg/24 h, respectively. A total of 55% of participants were African-American, 57% were women, 21% had a family history of diabetes, and 34% had a high school education or less (Table 1). Among these participants, 99 (9%) developed diabetes over the 15-year follow-up period, corresponding to a crude incidence rate of 7.21 per 1,000 person-years (Table 2).
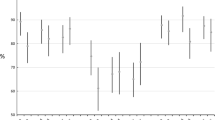
In unadjusted analyses, urinary potassium levels did not differ significantly between those who developed diabetes and those who did not (mean [SD] 51.6 [21.5] and 55.4 [23.7] mmol/day, respectively, p = 0.12). In unadjusted analyses, compared with their counterparts in the highest quintile of urinary potassium, those in the lowest to higher quintiles had HRs (95% CI) of incident diabetes of 1.70 (0.89, 3.24), 1.32 (0.67, 2.61), 1.16 (0.58, 2.31) and 1.64 (0.86, 3.12) (p trend = 0.10) (Table 3). There was no statistically significant interaction between urinary potassium and either race (p = 0.91) or sex (p = 0.73).
In multivariate models after adjustment for potential confounders, the association between urinary potassium and risk of incident diabetes strengthened and was statistically significant: compared with their counterparts in the highest quintile of potassium intake, those in the lowest quintile were more than twice as likely to develop diabetes (HR 2.45; 95% CI 1.08, 5.59; p for trend = 0.04) (Table 3). Urinary creatinine, used as a surrogate marker for kidney function, and, to a lesser extent, BMI seemed to account for the statistically significant association, thus acting as negative confounders. In all sensitivity analyses, we observed similar associations. When participants who had taken diuretics at any examination were excluded (n = 98, 9.2%), this association was strengthened. Compared with their counterparts in the highest quintile of urinary potassium, those in the lowest to higher quintile had adjusted HR (95% CI) of incident diabetes of 3.57 (1.33, 9.58), 2.72 (1.09, 6.77), 1.74 (0.75, 4.05) and 2.09 (0.97, 4.48), respectively.
Diet history of potassium intake analyses
We included 4,754 participants in the analyses of dietary potassium intake and risk of incident diabetes. The mean (SD) age, BMI and dietary potassium intake of all included participants were 25 (3.6) years, 24.5 (5.1) kg/m2 and 3,661 (1,735) mg/day respectively, with a mean (SD) energy intake of 11,757 (5,561) kJ/day (2,810 kcal/day); 50% were African-American, 55% were women, 14% had a family history of diabetes, and 38% had a high school education or less (Table 1). Age, BMI and both systolic and diastolic blood pressure were all fairly similar among participants with varied potassium intakes. However, participants in the highest potassium intake quintile compared with those in the lowest potassium intake quintile had slightly more education, lower average daily energy intake, reduced saturated fat intake, reduced intake of sweetened beverages, higher intake of fibre, fruit and vegetables, and higher physical activity scores, with similar patterns in African-Americans and whites (not shown).
Among these participants, 373 (8%) developed diabetes during a 20-year follow-up period, corresponding to a crude incidence rate of 4.68 per 1,000 person-years (Table 2). Those who developed diabetes had a lower mean intake of dietary potassium compared with those who did not (3,393 vs 3,684 mg/day; p = 0.002), the difference in mean daily intakes between the groups being roughly equivalent to the amount of potassium in one cup of fruit such as mango or nectarine. The risk of incident diabetes was significantly higher among participants in the lowest quintile of potassium intake compared with those in the highest quintile of potassium intake (p = 0.0008). In the analyses in which adjustment was made only for total daily energy intake, there was a significant inverse association between dietary potassium intake and risk of incident diabetes. HR (95% CI) of incident diabetes for participants in the lowest quintile of dietary potassium intake to the higher quintiles were 1.76 (1.26, 2.45), 1.56 (1.12, 2.19), 1.28 (0.91, 1.80) and 1.13 (0.80, 1.60), compared with the highest quintile of potassium intake (p trend = 0.003) (Table 3).
We found a significant interaction of dietary potassium with race (p = 0.001), but not with sex (p = 0.15). Multivariate analyses were therefore stratified by race. There was no increased risk of diabetes among whites who had lower dietary potassium intake, and rather there seemed to be a non-linear decreased risk of diabetes with lower potassium intake in this group. Compared with whites in the highest quintile of dietary potassium intake, those in the lowest to higher quintiles had an adjusted HR (95% CI) of incident diabetes of 0.81 (0.39, 1.71), 0.45 (0.23, 0.87), 0.36 (0.19, 0.68) and 0.59 (0.35, 1.00), respectively (Table 3). However, among African-Americans, we did find a significant, although non-linear, association between lower dietary potassium intake and increased risk of incident diabetes. Compared with African-Americans in the highest quintile of dietary potassium intake, those in the lowest to higher quintiles had adjusted HR (95% CI) of incident diabetes of 1.53 (0.80, 2.90), 1.80 (0.97, 3.33), 1.93 (1.06, 3.49) and 1.38 (0.75, 2.52), respectively (Table 3).
In all sensitivity analyses, we found similar results to those described above. Analysis of a model including total fruit and vegetable intake revealed a stronger association between lower dietary potassium intake and increased risk of diabetes in African-Americans, while the addition of this covariate did not change the opposite association found between dietary potassium and diabetes risk in whites. Compared with African-Americans in the highest quintile of dietary potassium, with adjustment for fruit and vegetable intake, those in the lowest to higher quintiles had adjusted HR (95% CI) of incident diabetes of 1.72 (0.87, 3.42), 1.99 (1.04, 3.78), 2.10 (1.14, 3.87) and 1.46 (0.79, 2.68), respectively. Compared with whites in the highest quintile of potassium intake, with adjustment for total fruit and vegetable intake, those in the lowest to higher quintiles had adjusted HR (95% CI) of incident diabetes of 0.95 (0.43, 2.07), 0.51 (0.25, 1.02), 0.38 (0.20, 0.74) and 0.64 (0.37, 1.08), respectively.
We evaluated the correlation between urinary potassium measurements at the year 5 examination and diet history of potassium intake at the year 0 examination and found the Pearson correlation coefficient (n = 1,042) to be equal to 0.26 (p < 0.0001).
Discussion
Data from this longitudinal study of a cohort of young adults of mixed races support the following conclusions. (1) Greater intake of dietary potassium seems to be associated with traits of an overall healthier lifestyle based on univariate associations. (2) There are significant associations between dietary potassium intake, measured both by urinary potassium and diet history, and risk of incident diabetes in multivariate models. (3) Lower urinary potassium is associated with increased risk of incident diabetes. (4) Lower dietary potassium, as assessed by diet questionnaire, is associated with increased risk of incident diabetes in unadjusted analyses and is associated with increased risk of incident diabetes in multivariate models in African-Americans. (5) The significant association between dietary potassium intake and diabetes risk is not simply a reflection of increased intake of fruit and vegetables and is independent of other dietary and lifestyle factors.
Several studies have evaluated the association between serum potassium and glucose metabolism, particularly in the context of thiazide use, but fewer studies have evaluated the association between dietary potassium and glucose metabolism and diabetes risk. Studies using hyperglycaemic clamps found that experimentally induced potassium depletion was associated with a decrease in pancreatic beta cell sensitivity to hyperglycaemia with a reduction in insulin release [13, 14]. Epidemiological studies and secondary analyses of hypertension trial data have found, generally, that thiazide use is associated with increased risk of diabetes [1, 15] and that the potassium depletion resulting from thiazide use may be the mediator of this increased risk [2, 3]. A recent secondary analysis of the Atherosclerosis Risk in Communities (ARIC) Study found a significant association between low normal serum potassium and increased diabetes risk independent of diuretic use [5].
The association between dietary potassium and serum potassium is not straightforward, as serum potassium levels are tightly controlled through homeostatic mechanisms to maintain cellular function. However, dietary potassium does influence total body potassium and presumably serum potassium to some extent [16]. The mechanism through which dietary potassium may affect glucose metabolism and diabetes risk has not been studied, but may be related to the effects of serum potassium on glucose metabolism.
Other studies evaluating the association between dietary potassium and diabetes risk have had mixed results, depending on the measurement of dietary potassium used, as well as the study population. One study, carried out in a Finnish, primarily white, population, found no significant association between urinary potassium and risk of diabetes [7]. A study based on the ARIC Study cohort, a biracial middle-aged cohort, did find significant associations between serum potassium and diabetes risk, but found no significant association between dietary potassium, as measured by a 61-item food-frequency questionnaire, and diabetes risk [5] A study using data from the Nurses’ Health Study, a female, primarily white cohort which is much larger than CARDIA and the other two cohorts described above, did find a significant association between dietary potassium intake, as measured by a similar 61-item semi-quantitative food frequency questionnaire, and diabetes risk, with adjustment for other traditional risk factors, but this association was diminished when other dietary measures were included in the model [6]. Whether these studies varied in their results because of the different populations examined or the different methods of measuring dietary potassium is not clear.
Some other studies have found significant associations between the intake of fruit and vegetables and risk of diabetes. One epidemiological study found that increased adherence to a DASH (Dietary Approaches to Stop Hypertension) diet, which is rich in fruit and vegetables and high in potassium, was associated with a lowered risk of diabetes [17]. A recent meta-analysis and review, which evaluated the association between the intake of fruit and vegetables and the risk of incident diabetes, did find a significant association between greater intake of leafy green vegetables, which are potassium-rich, and lower risk of diabetes [18]. However, this study was not able to examine the specific micronutrients that contributed to this association. This review also found that there were very few studies that looked adequately at the association between intake of particular fruits and vegetables and diabetes risk.
Finally, our finding of a statistical interaction between dietary potassium intake and race could be expected. Past studies have found that, compared with their white counterparts, African-Americans consume less potassium in their diet, excrete less potassium in their urine, and display a greater blood pressure-lowering response to potassium supplementation [16, 19–21]. In addition, a recent study of the ARIC cohort found that the association between low-normal serum potassium and increased diabetes risk was stronger in African-Americans than whites and that serum potassium was a significant mediator of the association between race and diabetes risk [22]. The mechanism leading to this differential effect of potassium—dietary or serum—on diabetes risk is not clear and deserves further study. The finding that there seemed to be a reduced incidence of diabetes among whites with lower intakes of dietary potassium was not expected and also needs further study.
This study has several limitations that deserve mention. The first is that the accuracy of both measures of potassium is limited, and we base our analyses on the measurement of these variables at one time point, rather than multiple time points. It has been found that 24 h urinary potassium measurements are highly correlated with dietary intake, with Pearson correlation coefficients of ~0.8 [16, 23, 24]. Potassium measurement by this method has also been found to be more reliable than diet history questionnaires [24]. However, 24 h urine collections are difficult to perform and are often inaccurate because of over- or under-collection [25]. Information on energy and nutrient intake based on diet questionnaires is also limited in its accuracy and reliability, with reliability coefficients of close to 0.5 based on one study [26], and is subject to bias based on various traits of the participants [27, 28]. In CARDIA in particular, it has been found that there may be differential misclassification in nutrient and energy reporting based on race [29]. In this study, we were unable to correlate dietary potassium intake and urinary potassium measurements directly, as a diet questionnaire was not administered at the 1990 visit, the visit at which 24 h urine samples were collected. However, the correlation between these two measurements, taken 5 years apart, was still significant.
The measurement that we use to adjust for renal function in the analyses involving urinary potassium was urinary creatinine, which is not the most accurate measure for this; however, other measures of renal function were not available to us at this time point.
Other limitations include the small sample size for the analyses, particularly those involving urinary potassium; however, we did have three 24 h measures in most of this sub-sample, which should make these exposure measures fairly accurate. The small sample size for these analyses could have limited our ability to detect a significant interaction between urinary potassium and race if one is indeed present, as is suggested by the analyses with diet history of potassium intake. Although the accuracy of the diet history questionnaire may be less than that of urinary potassium measures, we did have a larger sample size for these analyses. We were also not able to compare our findings on the association between dietary potassium intake and risk of diabetes with that of serum potassium and risk of diabetes, an association that has been found to be fairly strong in other cohorts, as serum potassium was not measured in this cohort [4, 5].
Strengths of this study include the mixed races of participants in this cohort, availability of biological measurements, extensive data on potential confounders, and long duration of follow-up which offered the opportunity to study long-term risk. Although the results we obtained from these analyses did not show a clear linear or dose–response relationship between dietary potassium and diabetes risk, the significant associations that we found using two different measures of dietary potassium, based on self-report as well as a biological marker, we believe, indicate that further study should be carried out to better define this association. Further studies would be best performed either in larger cohorts, with more precise self-report measures of dietary intake, or as clinical trials.
This study indicates that dietary potassium intake may affect risk of diabetes, particularly in African-Americans. Further study is needed to confirm these results in other populations and to determine if there is a direct causal association. Randomised clinical trials are needed to determine if potassium supplementation, either through dietary or pharmacological sources, could reduce the risk of diabetes, particularly in higher-risk populations.
References
Elliott WJ, Meyer PM (2007) Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 369:201–207
Zillich AJ, Garg J, Basu S, Bakris GL, Carter BL (2006) Thiazide diuretics, potassium, and the development of diabetes: a quantitative review. Hypertension 48:219–224
Shafi T, Appel LJ, Miller ER, Klag MJ, Parekh RS (2008) Changes in serum potassium mediate thiazide-induced diabetes. Hypertension 52:1022–1029
Heianza Y, Hara S, Arase Y et al (2011) Low serum potassium levels and risk of type 2 diabetes: the Toranomon Hospital Health Management Center Study 1 (TOPICS 1). Diabetologia 54:762–766
Chatterjee R, Yeh HC, Shafi T et al (2010) Serum and dietary potassium and risk of incident type 2 diabetes mellitus: the Atherosclerosis Risk in Communities (ARIC) study. Arch Intern Med 170:1745–1751
Colditz GA, Manson JE, Stampfer MJ, Rosner B, Willett WC, Speizer FE (1992) Diet and risk of clinical diabetes in women. Am J Clin Nutr 55:1018–1023
Hu G, Jousilahti P, Peltonen M, Lindström J, Tuomilehto J (2005) Urinary sodium and potassium excretion and the risk of type 2 diabetes: a prospective study in Finland. Diabetologia 48:1477–1483
Cutter GR, Burke GL, Dyer AR et al (1991) Cardiovascular risk factors in young adults. The CARDIA baseline monograph. Control Clin Trials 12:1S–77S
Shekelle RB, Shryock AM, Paul O et al (1981) Diet, serum cholesterol, and death from coronary heart disease. The Western Electric study. N Engl J Med 304:65–70
McDonald A, van Horn L, Slattery M et al (1991) The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc 91:1104–1112
Dyer AR, Cutter GR, Liu KQ et al (1990) Alcohol intake and blood pressure in young adults: the CARDIA Study. J Clin Epidemiol 43:1–13
Jacobs DR Jr, Hahn LP, Haskell WL, Pirie P, Sidney S (1989) Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Health program. J Cardiopulm Rehabil 9:448–459
Rowe JW, Tobin JD, Rosa RM, Andres R (1980) Effect of experimental potassium deficiency on glucose and insulin metabolism. Metabolism 29:498–502
Helderman JH, Elahi D, Andersen DK et al (1983) Prevention of the glucose intolerance of thiazide diuretics by maintenance of body potassium. Diabetes 32:106–111
Taylor EN, Hu FB, Curhan GC (2006) Antihypertensive medications and the risk of incident type 2 diabetes. Diabetes Care 29:1065–1070
Panel on Dietary Reference Intakes for Electrolytes and Water (2004) Chapter 5. Potassium dietary reference intakes for water, potassium, sodium, chloride, and sulfate. The National Academies Press, Washington DC, pp 186–268
Liese AD, Nichols M, Sun X, D'Agostino RB Jr, Haffner SM (2009) Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care 32:1434–1436
Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ (2010) Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 341:c4229
Minor DS, Wofford MR, Jones DW (2008) Racial and ethnic differences in hypertension. Curr Atheroscler Rep 10:121–127
Turban S, Miller ER, Ange B, Appel LJ (2008) Racial differences in urinary potassium excretion. J Am Soc Nephrol 19:1396–1402
Whelton PK, He J, Cutler JA et al (1997) Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA 277:1624–1632
Chatterjee R, Yeh HC, Shafi T et al (2011) Serum potassium and the racial disparity in diabetes risk: the Atherosclerosis Risk in Communities (ARIC) Study1,2. Am J Clin Nutr 93:1087–1091
Tasevska N, Runswick SA, Bingham SA (2006) Urinary potassium is as reliable as urinary nitrogen for use as a recovery biomarker in dietary studies of free living individuals. J Nutr 136:1334–1340
Bingham SA, Day NE (1997) Using biochemical markers to assess the validity of prospective dietary assessment methods and the effect of energy adjustment. Am J Clin Nutr 65:1130S–1137S
Cote AM, Firoz T, Mattman A, Lam EM, von Dadelszen P, Magee LA (2008) The 24-hour urine collection: gold standard or historical practice? Am J Obstet Gynecol 199(625):e621–e626
Bidulescu A, Chambless LE, Siega-Riz AM, Zeisel SH, Heiss G (2009) Repeatability and measurement error in the assessment of choline and betaine dietary intake: the Atherosclerosis Risk in Communities (ARIC) Study. Nutr J 8:14
Livingstone MB, Black AE (2003) Markers of the validity of reported energy intake. J Nutr 133(Suppl 3):895S–920S.3
Freedman LS, Schatzkin A, Midthune D, Kipnis V (2011) Dealing with dietary measurement error in nutritional cohort studies. JNCI 103:1086–1092
Liu K, Slattery M, Jacobs D Jr et al (1994) A study of the reliability and comparative validity of the cardia dietary history. Ethn Dis 4:15–27
Acknowledgements
We would like to acknowledge the CARDIA participants and the CARDIA Coordinating Center for their administrative support. We also acknowledge M. Pletcher of the University of California, San Francisco, for his review and thoughtful comments on the manuscript. We acknowledge the YALTA R01 HL 53560 program for measuring HbA1c.
Funding
The CARDIA Study and this research were funded by contracts N01-HC-48047 through 48050 and N01-HC-95095 from the National Heart, Lung, and Blood Institute, National Institutes of Health. H.C. Yeh and F.L. Brancati are supported by the NIDDK Diabetes Research and Training Center (P60 DK079637). F.L. Brancati is supported by a grant from the NIDDK, Bethesda, MD (K24 DK62222).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
RC conceived the idea, interpreted data, drafted the manuscript, and takes full responsibility for the content of this article. LC analysed and interpreted the data and revised the draft for important intellectual content. H-CY interpreted the data and revised the draft for important intellectual content. CA, MD and KL interpreted the data and revised the draft for important intellectual content. FB helped to conceive the idea, interpreted the data, and revised the draft for important intellectual content. All the authors listed above gave final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chatterjee, R., Colangelo, L.A., Yeh, H.C. et al. Potassium intake and risk of incident type 2 diabetes mellitus: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Diabetologia 55, 1295–1303 (2012). https://doi.org/10.1007/s00125-012-2487-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2487-3