ABSTRACT
Type 2 diabetes is a major public health issue in most countries around the world. Efficacy trials have demonstrated that lifestyle modification programs can significantly reduce the risk of type 2 diabetes. Two key challenges are: [1] to develop programs that are more feasible for “real world” implementation and [2] to extend the global reach of such programs, particularly to resource-poor countries where the burden of diabetes is substantial. This paper describes the development, implementation, and evaluation of such “real world” programs in Finland and Australia, the exchange between the two countries, and the wider uptake of such programs. Drawing on the lessons from these linked case studies, we discuss the implications for improving the “spread” of diabetes prevention programs by more effective uptake of lifestyle change programs and related strategies for more resource-poor countries and settings.
Similar content being viewed by others
BACKGROUND
In Finland and Australia, as elsewhere in the world, the rapid increase in the prevalence of type 2 diabetes has become a major public health concern since the 1990s [1, 2]. Efficacy trials have now demonstrated that programs focused on modifying lifestyle can contribute to a significant reduction in diabetes risk [3–5]. Follow-up studies have demonstrated that lifestyle change can be sustained after formal delivery of the intervention is completed [6–8]. While these results have been impressive, the interventions evaluated in such trials have typically involved intensive, individualized counseling delivered by highly trained health professionals. These are major limitations for wider uptake of such programs by health care systems around the world, particularly in low- and middle-income countries, where the burden of diabetes is substantial and where the availability of such highly trained health professionals can be nonexistent in the public health sector. Evidence for the preconditions and determinants of program spread within and between countries and health systems is still quite limited.
Vandenbroucke contrasts two views of medical science: one emphasizes discovery and explanation; the other emphasizes the evaluation of interventions, their “scaling up” and wider uptake [9]. He concludes that these two views lead to quite different approaches to research into program development and their wider uptake. Drawing on Vandenbrouke’s writings, Batalden points out that the kind of evidence—and its ordering—required for the development of programs, or for interventions to be tested in efficacy trials, is quite different from that which is used for wider implementation and system uptake. In other words, system-level uptake requires broader evidence development and triangulation of evidence from case studies, expert opinion, and the circumstances of the local context and not just the findings from intervention trials ([10] and personal communication with Professor Dunbar). Randomized trials that have been conducted to demonstrate the efficacy of a new intervention typically emphasize internal validity, often at the expense of external validity and generalizability to other settings, populations, and countries. However, it is also the case that even where context and external validity are addressed, this will still not necessarily result in broader implementation of a program and system-wide uptake [10]. A variety of research methods and approaches are required to discover the knowledge and to build the evidence base required for implementation in other contexts and settings from where efficacy and effectiveness trials have been conducted [11, 12]. To support effective program implementation and “scaling up” of programs in different contexts also requires knowledge about scale and practical experience and knowledge from practitioners and implementers who are actually engaged in the implementation process [13]. The latter is essential for successful adoption.
The need to understand more about the process of “scaling up” of interventions has been highlighted by Gaglio and others: “Few intervention studies discuss details of how they translate theory into practice or how they integrate different modalities and collaborating institutions, but such integration is critical for project success”[14]. Everett Rogers [15], who originally proposed the theory of diffusion of innovations, which has recently been elaborated by Oldenburg and Glanz [16], identifies that the spread of innovations is critically influenced by a number of important factors, including (1) relative advantage over the status quo, (2) compatibility with values and behaviors, (3) lack of complexity, and (4) trialability and observable results. Furthermore, in a narrative meta-analysis of how innovations spread throughout health services, Greenhalgh and colleagues concluded that "knowledge depends for its circulation on interpersonal networks, and will only diffuse if these social features are taken into account and barriers overcome." Greenhalgh also developed a useful framework for the components of diffusion of innovation for complex interventions in health services [17].
This paper describes the development, implementation, and evaluation of two theory-driven, lifestyle modification programs for diabetes prevention which were conducted in “real world” settings in Finland and Australia, and their subsequent wider uptake. Drawing on lessons learned from these case studies, as well as the work of Rogers [15], Oldenburg and Glanz [16], and Greenhalgh [17], we aim to explain why there has been such an impressive exchange and uptake of the diabetes prevention programs between Finland and Australia over the past 10 years. We also briefly discuss the implications for improving the “spread” of such programs, globally. The process of successfully translating behavioral medicine and public health programs from research into policy and practice around the world requires a much more detailed examination if we are to maximize the public health impact of such approaches.
FROM EFFICACY TO BROADER UPTAKE OF LIFESTYLE INTERVENTION PROGRAMS FOR DIABETES PREVENTION IN FINLAND AND AUSTRALIA
The initial publication of the Da Qing IGT and Diabetes Study [4], the Finnish Diabetes Prevention Study [5] (FinDPS), and the US Diabetes Prevention Study [3] in 1997, 2001, and 2002 respectively, provided the first compelling evidence from RCTs for the efficacy of lifestyle interventions in preventing diabetes progression among high-risk individuals. Following the publication of these findings, a series of research, funding, and policy developments in Finland advanced diabetes prevention efforts in that country. Similar developments commenced in Australia soon after this. The various steps from awareness of the problem and potential solutions to program planning, implementation, evaluation, maintenance, and diffusion in Finland and Australia are summarized in Table 1.
From efficacy to broader uptake in Finland
From efficacy to implementation
The Good Ageing in Lahti Region (GOAL) Program is a community program to promote the health of an aging population in the Päijät-Häme Region in Finland, an area covering 14 municipalities and a total of 208,000 inhabitants, situated 100 km north of Helsinki. The program commenced in 2002, with a plan to integrate a longitudinal cohort study on population health and well-being and targeted interventions [18, 19]. These interventions were to be based on collaborative needs assessment with the municipalities. At the time, the first results from the Finnish efficacy trial on preventing type 2 diabetes with lifestyle changes, the FinDPS, [5] had just been published. The National Diabetes Association in Finland strongly advocated the implementation of the findings [20], and the national and local policy environment was favorably disposed to do this. The regional health care authority in Päijät-Häme Region decided that the first intervention to be conducted as part of the GOAL Program would be a “real world” evaluation of a group-based, lifestyle change program to prevent type 2 diabetes in the primary health care setting, and that this should be modeled on the intervention that had been evaluated in FinDPS [19, 21].
The program partners included the local municipalities and regional and local health care organizations as the eventual user system for the program. The Finnish National Public Health Institute (currently, the National Institute for Health and Welfare), the UKK Institute for Health Promotion, the Lahti University of Applied Sciences, and the University of Helsinki agreed to be the key players in the development, implementation, and evaluation of this new program. To maximize the eventual fit of the program within the local health care context, a group of user representatives from each municipality and relevant professional groups was established to assist with these steps. Their main task was to ensure that this new program, if it could be demonstrated to achieve similar outcomes to FinDPS, would be suitable for integration with currently available care and wider uptake in the health services.
The intervention was adapted from the FinDPS program, using the same five key lifestyle change objectives already strongly associated with evidence for prevention of type 2 diabetes [5]. These included: a decrease of total and saturated dietary fat, increase of dietary fiber and physical activity, and weight loss. However, the GOAL implementation trial differed from the FinDPS in a number of important ways. First, the participants in the GOAL trial were current primary health care patients (age 50 to 65 years) with identified risk factors (obesity, hypertension, elevated blood glucose or lipids), and their eligibility was based on the Finnish Diabetes Risk Score (FINDRISC) diabetes risk assessment questionnaire [22] rather than impairments in glucose tolerance.
Second, the GOAL trial was group-based and had much lower program intensity as defined by the number of counseling sessions and program duration: the program consisted of five 2-h group sessions delivered over 8 weeks and one booster session at 8 months. The protocol included no further contacts with the participants except for the outcome measurements at 1 and 3 years, when clinical risk factors, nutrition and physical activity, and psychosocial mediators were measured. In comparison, the FinDPS had a median number of 20 individual 30–60-min counseling sessions, with the median length of the intervention being 4 years (range, 1–6). Furthermore, 20% of the participants in the DPS were also on a very low caloric diet [7].
Third, the GOAL trial was a structured, task-oriented program strongly based on Health Action Process Approach, a social cognitive health behavior model [23], motivational, and self-regulation theories [24]. Specific behavior change techniques included self-monitoring of behavior, goal setting, and planning for behavior change and maintenance, feedback, and relapse management. Information provision was limited to factors necessary for the use of these techniques. The sessions were supported by printed materials for facilitators and participants. Existing, free of charge health education leaflets were used especially for dietary advice, and food and physical activity diaries as well as goal setting and planning sheets were adapted from earlier studies [25]. Materials for relapse management were developed specifically for this intervention. More detailed descriptions of the program can be found in our previous papers [19, 21] and at http://www.palmenia.helsinki.fi/ikihyva/InEnglish.html.
Another very important feature of program development was that program feasibility and acceptability in the real world were key considerations in the program planning, and a number of the core research questions focused on the participants’ health behavior change processes in order to identify factors that would predict success and long-term sustainability [10, 26–30]. To promote future program sustainability, nurses who were currently employed in the region were assigned to deliver the GOAL program as part of their existing work. All facilitators received a standardized, 2-day training program with written materials and practical exercises in group facilitation. A nutritionist and municipal sports officers co-facilitated the relevant sessions on diet and physical activity. A nutritionist was hired (because none was available for preventive care in the region) and was assigned the tasks of coordinating the groups and supporting the nurse facilitators.
When compared to those in the original FinDPS efficacy trial, participants in the GOAL implementation trial were almost as likely to adopt the nutrition targets, but less likely to achieve the physical activity and weight loss objectives. Nevertheless, the program achieved favorable outcomes for several clinical risk factors. Diabetes risk, as measured by glucose tolerance at follow-up, was associated with attainment of the lifestyle objectives by individuals. Although the weight loss outcome was more modest than that observed in the FinDPS, it was well maintained at 3-year follow-up. Furthermore, conversion to type 2 diabetes among those with elevated blood glucose at baseline was 12%, falling between the FinDPS intervention and control groups [31]. Process evaluation showed that increase of self-efficacy and planning during the intervention predicted changes in lifestyle [10, 26]. Furthermore, increased self-efficacy in the first 3 months of the intervention also predicted reduction in waist circumference at 3-year follow-up [27].
From implementation to broader uptake
After a successful testing period, measures were taken to maximize the sustainability of the program in routine care. Two upstream factors were critical for this effort: (1) strong leadership of the regional health care in advocating the program and (2) national policy supporting broad uptake of evidence-based programs, and, as a direct implication of this, funding received from the Ministry of Social Affairs and Health. However, during the lifestyle implementation trial, it had also become evident that in order to make preventive practices more effective and to support the broader uptake of the program, other professional groups needed to be integrated in a more systematic way. In the trial, at-risk patients were predominantly identified by the nurses, and patients who were only seen by doctors were less systematically screened. Another problem was post-counseling follow-up, which was not organized. Hence, some patients reverted to their preprogram risk factor routine, while others were lost to follow-up after the study. In order to create a proactive approach instead of the prevailing reactive approach, a more comprehensive focus on the way in which preventive health services were organized was required. For this purpose, another intervention project—i.e., a trial to implement Current Care Guidelines (CCG) that focused on preventing cardiovascular diseases (CVD) in the health care system—was also started within the GOAL Program with funding from the Academy of Finland Health Services Research Program (2003–2007). This project became another key element in building the sustainability of the GOAL lifestyle intervention program.
Within the CCG trial, health care professionals worked together to establish and implement evidence-based care processes for prevention of CVD, based on national guidelines on treatment of hypertension, dyslipidemia, adult obesity, and smoking and nicotine dependency. These included three integrated processes: identification of patients at risk, lifestyle counseling, and follow-up. All processes defined criteria and measures that were to be used as well as division of responsibilities between different professionals and the patient. Evaluation of the patient’s risk status is performed at baseline and at 12 months. Patients still struggling to adopt a healthy lifestyle at follow-up are encouraged to participate in biannual booster group sessions and receive a referral to oral glucose tolerance test; those with normal glucose tolerance (NGT) receiving the test after 3 years, those with impaired glucose tolerance (IGT) or impaired fasting glucose after 1 year. Patients who have developed type 2 diabetes or who require risk-lowering pharmacotherapy are referred to medical care. In practice, every health care center has established medical care processes for diabetes, hypertension, and dyslipidemia. Implementation of the process was supported with an education and training component of the CCG intervention, and the Ministry of Social Affairs and Health funded the development of an online database for risk screening and lifestyle counseling materials for the health care professionals. During the intervention, relevant training programs were established, and electronic patient registries were modified to allow recording of lifestyle change outcomes.
When the CCG intervention came to its end in 2006, regional and local health care authorities took responsibility for organizing structural and administrative changes necessary for system-wide uptake of the process that now had evolved into a regional, comprehensive, and integrated process for preventing type 2 diabetes and CVD. Finally, in the beginning of 2008, the process was integrated into the routine processes of the region’s primary health care organizations. Furthermore, the online database with updated versions of risk-screening measures and tools for lifestyle counseling, and the ongoing training programs for group facilitators have now been institutionalized. Also, the electronic patient record has been modified to allow registration of risk status and lifestyle data in addition to clinical risk factors. This allows the effectiveness of the preventive process to be evaluated.
In Päijät-Häme, the process prevails in routine preventive care for adults, and with the success established, its implementation has also been observed across other regions of Finland. Furthermore, with an initiative from the Päijät-Häme health care, the group counseling model has now been adapted and will be pilot tested for parents with overweight and obese children.
From efficacy to broader uptake in Australia
From efficacy to implementation
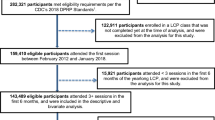
The Greater Green Triangle Diabetes Prevention Program (GGT DPP) was funded by the Australian Government as a national demonstration intervention project in 2004. It was adapted from the Finnish GOAL program (described in the previous section) as a result of collaborative links and exchanges between senior researchers from the then Finnish Public Health Institute and the Australian Greater Green Triangle (GGT) University Department of Rural Health located in southeastern Australia. Drawing on evidence from the GOAL program, this diabetes prevention program was modified in the Australian context (see Table 1). Stakeholders, especially General Practitioners (GPs) and practice managers, were consulted for their practical advice on implementation. A major difference from the GOAL trial was the addition of the Hospital Anxiety and Depression Scale (HADS)—a 14-item instrument used to measure anxiety and depression. Another major difference was that the study nurses who facilitated the group program were employed in a part-time capacity, exclusively for that purpose. In Australia, this was the only feasible practice since nurses are generally independent entrepreneurs, i.e., they are allied with and not employed by the General Practices.
Potential study participants were screened by the study nurses, using the self-administered eight-item FINDRISC questionnaire [22] in reception areas of General Practices in three rural areas. Using the same selection criteria as the GOAL study, 343 individuals were identified as being at high risk for type 2 diabetes, with FINDRISC scores of 12 or higher, and recruited for the trial. The structure of the group sessions was similar to the GOAL study, with five sessions conducted fortnightly and the sixth session held 8 months after the first. The lifestyle intervention imbeds the Health Action Process Approach model, motivational and self-regulation theories within the content of the sessions, and the overall goals of the program are similar to the FinDPS: decreased fat and saturated fat, increased fiber and physical activity, and modest weight loss. At 12-month follow-up, participants reported significant improvements in waist, weight, and other clinical variables. In contrast to the GOAL program, GGT DPP participants achieved better weight loss, with 75% achieving some waist reduction and 68% achieving weight reduction. Of the participants who had impaired values at baseline, 2.2% developed type 2 diabetes during the intervention. [32, 33]. The use of the HADS to identify depression demonstrated it to be a predictor of early dropout from the program, although those who completed the program improved their depression scores. At 3-year follow-up, participants maintained the majority of the previously observed gains, except for HADS [34].
From implementation to broader uptake
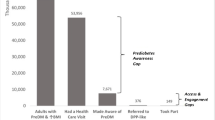
The results of the GGT DPP were presented to the Australian Government’s Office of Prime Minister and Cabinet, the Australian Department of Health and Ageing, and the State Government of the Victorian Office of the Premier by the Australian–Finnish team in face-to-face meetings. The Victorian Office of the Premier was the lead jurisdiction in Australia at that time for all Australian Governments (Council of Australian Governments (COAG)) on diabetes prevention. At the end of 2006, it issued a consultation document identifying GGT DPP as the only evidence-based intervention in Australia in this area. COAG formally agreed to a proposed AUD $200 million fund for diabetes prevention to develop an Australian version of the FINDRISC score (Australian Type 2 Diabetes Risk Assessment Tool (AUSDRISK)) and national standards for group-based lifestyle modification programs that would build on the extensively developed and published experience from Australia and Finland.
The Federal Government introduced incentives for GPs to identify people at risk for diabetes and allied health staff to deliver group-based, lifestyle modification programs for people aged 40–49 years. The Victorian government introduced the Life! Taking action on diabetes program which is currently being made available to and being evaluated with 25,000 residents over 50 years of age throughout the Australian state of Victoria. This program uses community-based facilitators (e.g., nurses, diabetes educators, dieticians) who receive 3 days of intensive training, along with support materials and self-learning tasks.
The structure of the new Life! program has evolved from the GOAL and GGT DPP program. Participants in the Life! program are first screened using the AUSDRISK test; those eligible to join have a minimum score of 15 and confirmed exclusion of type 2 diabetes. Referral to the program by the GP includes measures of height, weight, waist circumference, blood pressure, and cholesterol. The Life! program comprises six structured group sessions, each about 2 h in duration, conducted by trained facilitators in community settings. Participants are provided a workbook that includes materials for use in the group sessions as well as take-home tasks. Sessions 1 and 2 focus on risk perception, outcome confidence, and self-efficacy. Sessions 3 and 4 include visits from dieticians and exercise physiologists to provide information and assist with goal setting and creating individual plans for eating behavior and physical activity goals. Sessions 5 and 6 are review sessions to assist long-term maintenance of behavior change.
Life! facilitators are trained to support group participants in the behavior change process. The training consists of an orientation day, self-learning period, a 2-day workshop, and annual training review and quality assurance. The supporting material includes a facilitator manual, DVD, workshop activities, and training evaluation tools. Feedback about the progress of the program to the funding bodies is provided through regular evaluation reports and measurements. The Life! program is one of the world’s largest systematic, government-funded diabetes prevention programs. Details about the intervention, training, and implementation are provided in the Diabetes Prevention in Practice book prepared for the Dresden World Congress in Diabetes Prevention [35].
KEY ELEMENTS INVOLVED IN THE DEVELOPMENT, IMPLEMENTATION, AND EVALUATION OF EACH PROGRAM
Table 2 summarizes the key elements associated with each of the diabetes prevention programs in Finland and Australia in relation to setting, organizations, funding, target population, and program elements. For example, the lead institutions of both the Finnish and Australians programs were both closely linked with strategic regional, national, operational, and research partners. Close collaborative exchanges between the Australian and Finnish teams were another critical success factor for developing an effective exchange process. Importantly, both institutions were in receipt of program funding for the stages of program development, implementation, and evaluation. The target populations for each program were also similar, that is, those screened for high risk for type 2 diabetes, and in the case of the GOAL and GGT DPP programs, the participants were also living in primarily rural or semi-urban settings. Both programs had the same, clearly defined, session objectives with a strong theoretical basis, and similar delivery conditions and training for the program facilitators. Table 2 summarizes the success factors that were critical to the development of strong, evidence-based programs and their subsequent adoption and wider uptake.
DISCUSSION
These two linked case studies illustrate the steps by which programs based on groundbreaking efficacy trials were first translated into implementation trials in Finland and then Australia, and their subsequent development and broader uptake in each country. They provide insights into some of the key factors that facilitate and inhibit successful adoption of programs by program implementers, as well as how such programs require refinement in order to be suitably “scaled up” for further development, adaptation, and implementation in different countries and settings.
Drawing on the critical factors for spread of innovations between different cultures and contexts that were outlined by the theory of diffusion of innovations [15–17] and further specified for innovation spread throughout health services, we discuss the exchange and uptake of the diabetes prevention programs between Finland and Australia over the past 10 years.
Relative advantage over the status quo
In Finland, the implementation trials were able to pinpoint some of the crucial shortcomings in preventive practices that professionals could easily identify as causes of frustration in their own work—as some key people from within the health care system put it: “nobody knows who is doing what (and how) to whom with which criteria, in our system.” A common shared feeling was that practice change was necessary and inevitable, and implementation of feasible, evidence-based risk screening and intervention came as a welcome answer to this need. Before the FINDRISC, screening for the risk of diabetes had used the oral glucose tolerance test, which required blood sampling over 2 h. Uptake had always been low. The advent of the FINDRISC instrument allowed large numbers of people to be screened rapidly. Also, between the FinDPS randomized trial and the GOAL implementation trial, there was considerable thought given to how the most up-to-date theories on bringing about behavioral change in diet and physical activity could be applied to a six group session intervention.
Compatibility with values and behaviors
The importance of diabetes prevention was well understood by health professionals—and increasingly by both policy makers and politicians—in both countries. The question was how it could be incorporated into the routine workflow of health professionals and existing health systems. The use of FINDRISC and AUSDRISK, administered by specially trained nurses, who, along with other health professionals, could also facilitate the group sessions, were compatible with the existing primary care systems of both countries. Primary care physicians and their staff had little difficulty seeing the benefits for their patients and understanding that there would be little negative impact on their workload. Lifestyle counseling was already being conducted by many nurses and other health professionals, but it was being performed on an individual basis which many professionals found time-consuming and problematic to conduct. With the uptake of the FINDRISC, the health care system was not equipped for offering individual intervention to all those identified as they might have earlier, and this factor increased the perceived need for group counseling. “With the numbers of patients at risk for diabetes, we just have to move from individual counseling to groups” was a statement often heard from nurses coming to facilitator training in Finland.
Lack of complexity
Recruitment of participants by the nurses and the relatively small but important supporting role of GPs maximized the high uptake of the program in Australia. The health professional facilitator model helped to define specific tasks and objectives for the content of the sessions, and the overall model for preventive practices defined professional roles. Credibility of the program and ease of referral were enablers for physicians to encourage patients to join the programs. They were asked to refer patients for screening and reinforce the lifestyle change message. A structured counseling program and easy access to all materials promoted adoption of the program among facilitators.
Trialability and observable results
The GOAL and the GGT DPP were designed and conducted in alignment with research standards. Results of both studies were published in the scientific literature. Results from the GOAL program were reported to regional and local policy makers in Päijät-Häme Province, and a comprehensive report describing the path from research to policy was distributed to public provincial health services organizations nationwide. Further, the Australian results were presented to senior policy makers at the federal- and state-level by an Australian–Finnish team. For the policy makers, it is likely that the presence of the Finnish researchers added to the perception of receiving objective advice. That FINDRISC had been trialed in Australia almost certainly hastened the development of the Australian version, AUSDRISK.
A major stumbling block in extrapolating the research findings from trials to effective program implementation and wider uptake into health services and other community settings is to acquire commitment from governments and related bodies for program sustainability. This requires leadership, appropriate policy, funding, and other key supports. Another challenge is to ensure that the findings of the researchers, including their tacit knowledge of what works, do not get lost during the process of policy making. Fortunately, in this particular instance, policy makers in both Finland and Australia were already primed to identify appropriate programs to implement. Hence, there was already a favorable environment in which to demonstrate the outcomes of the programs. The role of the researchers and program implementers in Australia and Finland was to assist policy makers to choose the best options based on the evidence that had been recently generated.
The concept of linkage and exchange has been used to describe the transfer process by which researchers, implementers, and policy makers work together collaboratively and in partnership, so that the former can provide the evidence base for the latter [36]. This is at least as much a social as a technical exercise. Human interaction is important in ensuring the uptake of the results of research by decision makers. Close involvement with the policy makers by the Australian researchers went beyond mere presentation of the facts. Many detailed discussions of the options to configure the implementation specifically for the Victorian health system occurred through face-to-face meetings; we propose this to be an essential part of the process if policy makers are to make best use of the results of research. By contrast, these same detailed discussions did not occur to the same extent at the national level; nationally coordinated implementation has been more poorly configured, and the uptake rate has been lower.
Other critical success factors
In both countries, there was a supportive atmosphere for policy change in relation to chronic conditions like diabetes. In Finland, the Government supported regional uptake after the implementation trials; in Australia, within a year of the completion of the implementation trial, the COAG decided to prioritize diabetes prevention, nationally, and more funding has been provided for this purpose in recent years. In practice, all these followed from interaction between the research teams and the policy makers. In Finland, the Ministry of Social Affairs and Health was represented in the GOAL Program steering committee; in Australia, the COAG set up a committee and invited the GGT team to join it, who in turn invited a COAG representative into the project management steering committee. In both countries, several key people involved in the projects also participated in different expert committees over the years where they were able to share early results and advocate the programs. Key nongovernment organizations, such as Diabetes Australia Victoria and the Finnish Diabetes Association, have also been important advocates for diabetes prevention. Champions and opinion leaders arose quite quickly among the health care managers and health professionals involved in the implementation in both countries, such as the general practitioners in Australia, in whose practices the trial was conducted. Their views spread widely. It is also likely that the strong theoretical basis of GOAL aided portability.
Barriers and obstacles
Despite the many factors promoting success, there were also barriers to overcome. Mostly, these were factors that promoted early adoption but later turned into barriers for maintenance. In Finland, one such factor was external project funding within a limited time frame: while it lowered the threshold for the municipalities to participate and allowed swift program development and implementation, it also challenged system-wide uptake as municipalities were tempted to start new developmental projects in different problem areas with new external funding instead of committing to program maintenance in which they needed to use their own funding. To overcome this barrier required dedication from key stakeholders in the regional health care management and support from the research team.
Another such factor was the nature of the intervention program. While the structure and ready-made materials lowered the threshold for adoption, the facilitators discovered that it requires a different kind of preparation than the rather professional-driven individual counselling nurses were used to giving [37], and required specific interactive skills that they did not necessarily feel they mastered adequately. To solve these problems, the role of the program dietician was extended from support in dietary issues to more general support to facilitators. In both countries, one of the major focus areas in further training was improvement of facilitators’ skills and self-efficacy in interaction. With the training, support, and increasing practical experience, they also gained more confidence.
Why did it take almost 10 years for the program to start spreading to other regions within Finland? A National Development Program for the Prevention and Care of Diabetes (DEHKO 2000–2010) was launched almost simultaneously with the GOAL Program, and many regions participated to prevent type 2 diabetes, the FinD2D (2003–2010) [38]. While the program was remarkably successful in raising awareness about diabetes prevention and in advocating risk screening, instead of providing one or several focused approaches for the intervention, it described over 300 different kinds of interventions used. Many regions have now decided to focus on and integrate the GOAL intervention into the preventive processes they implemented during the D2D.
In summary, the successful exchange of results of randomized trials and implementation trials between Finland and Australia, followed by a national rollout in both countries, resulted from a number of factors. In both countries, diabetes was seen as a health issue of rapidly increasing importance, and the proposed programs had good policy salience in both countries. The primary care systems were broadly compatible, and health professionals understood the importance of the problem. The development of the FINDRISC score and the sound psychosocial theories underpinning the group intervention were also important. A key feature for facilitating the relatively quick transfer and adoption of the program from the FinDPS efficacy trial to Finland and Australia was the extensive interaction between program leaders, researchers, practitioners, and policy makers within and between the two respective countries. They shared tacit knowledge that had not been published formally in peer-reviewed publications, and the interactions generated many of the recommendations that have been incorporated into subsequent iterations of the program.
Looking forward to the future, it is pertinent to consider the further adaptation and translation of this program approach and delivery system to other countries, particularly low- and middle-income countries. It is important to consider how this approach might be enhanced by linking with other group-based or peer support programs, information and communications technology, and other methods that are not as dependent on delivery systems that require a well-funded and well-resourced health system. Advice on implementation has already been provided by the authors to potential program implementers in India, Malaysia, Sri Lanka, China, and South Africa, and a number of new programs are currently being developed, implemented, and evaluated (Table 3). It has been recently estimated that more than 70% of those with diabetes in the world now live in developing countries, and this proportion is increasing annually. Yet, the number of studies formally evaluating the prevention of diabetes and its complications in developing countries is minimal [39]. Therefore, there is an important opportunity to formally investigate whether the kinds of programs that have been developed and extensively evaluated in Finland and Australia over the last 10 years can be appropriately adapted for effective implementation and “scaling up” in low- and middle-income countries.
REFERENCES
Lammi, N., Taskinen, O., Moltchanova, E., et al. (2007). A high incidence of type 1 diabetes and an alarming increase in the incidence of type 2 diabetes among young adults in Finland between 1992 and 1996. Diabetologia, 50, 1393–1400.
Murray, C. J. L., & Lopez, A. D. (Eds.). (1996). The global burden of disease: a comprehensive assessment of mortality and disability from disease, injuries, and risk factors in 1990 and projected to 2020. Cambridge: Harvard University Press.
Knowler, W., Barrett-Connor, E., Fowler, S., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine, 346(6), 393–403.
Pan, X. R., Li, G. W., Hu, Y. H., et al. (1997). Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care, 20(4), 537–544.
Tuomilehto, J., Lindstrom, J., Eriksson, J. G., et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England Journal of Medicine, 344(18), 1343–1350.
Li, G., Zhang, P., Wang, J., et al. (2008). The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet, 371(9626), 1783–1789.
Lindstrom, J., Ilanne-Parikka, P., Peltonen, M., et al. (2006). Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet, 368(9548), 1673–1679.
Ratner, R. E., & for the Diabetes Prevention Program Research Group. (2006). An update on the Diabetes Prevention Program. Endocrine Practice, 12(Suppl 1), 20–24.
Vandenbroucke, J. P. (2008). Observational research, randomised trials, and two views of medical science. PLoS Medicine, 5(3), e67.
Hankonen, N., Absetz, P., Haukkala, A., & Uutela, A. (2009). Socioeconomic status and psychosocial mechanisms of lifestyle change in a type 2 diabetes prevention trial. Annals of Behavioural Medicine, 38(2), 1418–1420.
Davies, H., Nutley, S., & Walter, I. (2008). Why knowledge transfer is misconceived for applied social research. Journal of Health Services Research & Policy, 13, 188–190.
Fisher, E. (2008). The importance of context in understanding behavior and promoting health. Annals of Behavioral Medicine, 35, 3–18.
Conklin, A., Hallsworth, M., Hatziandreu, E., & Grant, J. (2008). Briefing on linkage and exchange: facilitating diffusion of innovation in health services. Santa Monica: RAND Corp.
Gaglio, B., Smith, T. L., Estabrooks, P. A., Ritzwoller, D. P., Ferro, E. F., & Glasgow, R. E. (2010). Using theory and technology to design a practical and generalizable smoking reduction intervention. Health Promotion Practice, 11(5), 675–684.
Rogers, E. (2003). Diffusion of innovations. Fifth edition. New York: Free Press.
Oldenburg, B., & Glanz, K. (2008). Diffusion of innovations. In K. Glanz, B. Rimer, & K. Viswanath (Eds.), Health behavior and health education: Theory, research and practice. San Francisco: Wiley.
Greenhalgh, T., Stramer, K., Bratan, T., Byrne, E., Mohammad, Y., & Russell, J. (2008). Introduction of shared electronic records: multi-site case study using diffusion of innovation theory. British Medical Journal, 337, a1786.
Fogelholm, M., Valve, R., Absetz, P., et al. (2006). Rural–urban differences in health and health behaviour: a baseline description of a community health promotion program for the elderly. Scandinavian Journal of Public Health, 34(6), 632–640.
Uutela, A., Absetz, P., Nissinen, A., Valve, R., Talja, M., & Fogelholm, M. (2004). Health psychological theory in promoting population health in Paijat-Hame, Finland: first steps toward a type 2 diabetes prevention study. Journal of Health Psychology, 9(1), 73–84.
Saaristo, T., Peltonen, M., Keinanen-Kiukaanniemi, S., et al. (2007). National type 2 diabetes prevention programme in Finland: FIN-D2D. International Journal of Circumpolar Health Promotion Practice, 66, 101–112.
Absetz, P., Valve, R., Oldenburg, B., et al. (2007). Type 2 diabetes prevention in the "real world": one-year results of the GOAL implementation trial. Diabetes Care, 30(10), 2465–2470.
Lindstrom, J., & Tuomilehto, J. (2003). The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care, 26(3), 725–731.
Schwarzer, R., & Renner, B. (2000). Social–cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychology, 19, 487–495.
Gollwitzer, P. (1999). Implementation intentions. Strong effects of simple plans. American Psychologist, 54, 493–503.
Lindahl, B., Nilsson, T., Jansson, J.-H., Asplund, K., & Hallmans, G. (1999). Improved fibrinolysis by intense lifestyle intervention. A randomised trial in subjects with impaired glucose tolerance. Journal of Internal Medicine, 246, 105–112.
Hankonen, N., Absetz, P., Renner, B., Ghisletta, P., & Uutela, A. (2010). Gender differences in social cognitive determinants of exercise adoption. Psychology & Health, 25(1), 55–69.
Hankonen, N., Vollmann, M., Renner, B., & Absetz, P. (2010). What is setting the stage for abdominal obesity reduction? A comparison between personality and health-related social cognitions. Journal of Behavioral Medicine, 33(5), 415–422.
Jallinoja, P., Pajari, P., & Absetz, P. (2008). Repertoires of lifestyle change and self-responsibility among participants in an intervention to prevent type 2 diabetes. Scandinavian Journal of Caring Sciences, 22, 455–462.
Jallinoja, P., Pajari, P., & Absetz, P. (2010). Negotiated pleasures in health-seeking lifestyles of participants of a health promoting intervention. Health: An Interdisciplinary Journal of The Social Study of Health, Illness and Medicine, 14(2), 115–130.
Yoshida, S., Hankonen, N., & Absetz, P. (2006). Facilitators’ self-fulfillment predicts successful weight change in life-style counseling program. International Journal of Behavioral Medicine, 13, (Suppl., 292).
Absetz, P., Oldenburg, B., Hankonen, N., et al. (2009). Type 2 diabetes prevention in the real world. Diabetes Care, 32(8), 1418–1420.
Kilkkinen, A., Heistaro, S., Laatikainen, T., et al. (2007). Prevention of type 2 diabetes in a primary health care setting: Interim results from the Greater Green Triangle (GGT) Diabetes Prevention Project. Diabetes Research and Clinical Practice, 76(3), 460–462.
Laatikainen, T., Dunbar, J., Chapman, A., et al. (2007). Prevention of type 2 diabetes by lifestyle intervention in an Australian primary health care setting: Greater Green Triangle (GGT) Diabetes Prevention Project. BMC Public Health, 7(1), 249.
Dunbar, J. A., Davis-Lameloise, N., Philpot, B., et al. (2010). Sustained gains from a diabetes prevention program and the role of telephone support. International Journal of Diabetes Mellitus, 2(2), 95–100.
Schwarz, P., Reddy, P., Greaves, C., Dunbar, J., & Schwarz, J. (2010). Diabetes prevention in practice. Dresden: Tumaini Institute for Prevention Management.
Goering, P., Butterill, D., Jacobson, N., & Sturtevant, D. (2003). Linkage and exchange at the organizational level: a model of collaboration between research and policy. Journal of Health Services Research & Policy, 8(suppl_2), 14–19.
Kiuru, P., Poskiparta, M., Kettunen, T., Saltevo, J., & Liimatainen, L. (2004). Advice-giving styles by Finnish nurses in dietary counseling concerning type 2 diabetes care. Journal of Health Communication, 9(4), 337–354.
Saaristo, T., Moilanen, L., Korpi-Hyövälti, E., et al. (2010). Lifestyle intervention for prevention of type 2 diabetes in primary health care: one-year follow-up of the Finnish National Diabetes Prevention Program (FIN-D2D). Diabetes Care, 33(10), 2146–2151.
Rawal, L. B., Tapp, R. J., Williams, E. D., Chan, C., S Y, Oldenburg, B (2011) Prevention of type 2 diabetes and its complications in developing countries: a review. International Journal of Behavioral Medicine (in press).
Acknowledgements
The GOAL Lifestyle Implementation Trial was funded by the Academy of Finland (Program for Health Promotion), the Social Insurance Agency, and the Ministry of Social Affairs and Health. The Greater Green Triangle DPP study was funded by The Australian Government Department of Health and Ageing. Life! Taking Action on Diabetes is funded by the Department of Health Victoria and managed by Diabetes Australia Victoria.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Implications
Practice: Evidence from efficacy trials of lifestyle interventions for the prevention of type 2 diabetes supports translation into implementation trials and further scaling up for widespread adaptation in other countries.
Policy: Resources should now be directed towards the more widespread uptake and implementation of lifestyle interventions for individuals at high risk for diabetes. Financial and organizational support is of particular importance to maximize effective translation.
Research: Research should be directed towards the more formalized evaluation of the key elements involved in the cultural tailoring and adaptation of programs to different settings and countries.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Oldenburg, B., Absetz, P., Dunbar, J.A. et al. The spread and uptake of diabetes prevention programs around the world: a case study from Finland and Australia. Behav. Med. Pract. Policy Res. 1, 270–282 (2011). https://doi.org/10.1007/s13142-011-0046-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-011-0046-y