Abstract
Background
Although Escherichia coli is the most frequently isolated microorganism in acute biliary tract infections with bacteremia, data regarding its virulence are limited.
Results
Information on cases of bacteremia in acute biliary tract infection in a retrospective study was collected from 2013 to 2015 at a tertiary care hospital in Japan. Factors related to the severity of infection were investigated, including patient background, phylogenetic typing, and virulence factors of E. coli, such as adhesion, invasion, toxins, and iron acquisition.
In total, 72 E. coli strains were identified in 71 cases, most of which primarily belonged to the B2 phylogroup (68.1%). The presence of the iutA gene (77.3% in the non-severe group, 46.4% in the severe group, P = 0.011) and the ibeA gene (9.1% in the non-severe group, and 35.7% in the severe group, P = 0.012) was significantly associated with the severity of infection. Among the patient characteristics, diabetes mellitus with organ involvement and alkaline phosphatase were different in the severe and non-severe groups.
Conclusions
We showed that bacteremic E. coli strains from acute biliary tract infections belonged to the virulent (B2) phylogroup. The prevalence of the iutA and ibeA genes between the two groups of bacteremia severity was significantly different.
Similar content being viewed by others
Background
Escherichia coli is the most frequently isolated microorganism in acute biliary tract infections [1, 2], and the associated bacteremia is mainly caused by E. coli [3]. Biliary tract infections normally start with the stasis of bile flow, and once intestinal bacteria flow into the bile duct, an acute biliary infection can develop. The causative organisms in bile cultures of acute biliary infections were shown to be polymicrobial [3, 4]. These pathogens were considered intestinal commensals of low virulence [5].
E. coli can be differentiated depending on its pathogenicity as commensal, which are considered avirulent; intestinal pathogenic; extraintestinal pathogenic, such as uropathogenic, neonate meningitis groups and sepsis-associated groups; and as avian pathogenic [6, 7].
Acute biliary infections, such as cholangitis and cholecystitis, can develop into a severe infection with bacteremia. In cases of severe infection, mortality can reach 10% [8]. This begs the question, if the causative organisms are considered to be avirulent, why did the patients suffer severe disease and even death?
We hypothesized that the causative E. coli were virulent, and this influenced the severity of acute biliary infection. Uropathogenic E. coli strains, which cause urinary tract infections, have been extensively studied, and have shown to express several virulence factors, such as those involved in adhesion (afaB/C, fimH, iha, papC, papG2, and sfaD/E), toxicity (cnf1, hlyA, sat, and usp), iron acquisition (fyuA, ironN, iucD and iutA), capsule synthesis (kpsMT2), and miscellaneous genes (cvaC, ibeA, ompT, tcpC, and traT). These virulence factors play important roles at each step of infection [9]. Studies on E. coli strains from bacteremia in biliary tract infections are however limited. A previous study showed different prevalences of 10 virulence factors (afa, cnf1, fimH, foc, hlyA, iutA, papG class I, papG class II, papG class III, and sfa) in Biliary pathogenic E. coli (BEC) strains compared in E. coli strains from blood cultures of patients with acute urinary tract infections [10]. BEC strains might exist and have unique traits as uropathogenic E. coli strains have.
Pathogenic E. coli express many common virulence factors even at different sites of infection, but an organ-specific strategy is needed to identify specific virulence factors. These common and/or different traits are now studied rigorously to understand pathogenesis and to cope with infection at different foci.
Our study aimed to analyze the relationship between the severity of biliary tract infections and the prevalence of the virulence factors of BEC isolates.
Results
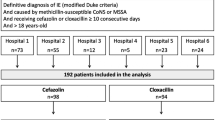
A total of 71 cases of bacteremic acute biliary tract infections (72 BEC isolates) were identified. In one of the patients, two E. coli isolates with different colony morphology were detected; we have included both isolates in the study.
The patients were grouped depending on their severity level, and the characteristics of the severe group (Pitt’s score ≥ 2) and the non-severe (score < 2) group were compared. Patient background, such as age, gender, and comorbidity were the same in the two groups, except for diabetes mellitus (DM) with organ involvement (Table 1). More than half of the patients in both groups presented abnormalities of the biliary tract and had experienced biliary tract infections in the past.
The laboratory data showed that the liver enzymes and biliary markers analyzed were elevated to the same degree in the two severe and non-severe groups, except for alkaline phosphatase (ALP), and the median white blood cell counts, which were higher in the non-severe group (Table 2).
Next, we compared the phylogenetic groups, ST lineages, and virulence factors of BEC by the severity level (Table 3). The most detected phylogenetic group was B2 in both groups (70.5% in non-severe, 64.3% in severe), and the proportion of each phylogenetic group between the severe and non-severe groups was similar. BEC isolates mainly belonged to the B2 phylogenetic group (68.1%), and to ST131 (23.6%) and the ST95 (19.4%) lineages, as detected by multi-locus sequencing typing (MLST). The extended-spectrum-beta-lactamase (ESBL)-producing isolates were detected 12 isolates, including 7 of ST131 lineage, and others were one each of ST10, ST95, ST354, ST648, and ST1196 lineages, respectively. The proportions of STs and prevalence of the ESBL-producing isolates were not significantly different between the two groups.
The presence of the iutA gene (77.3% in the non-severe group, 46.4% in the severe group, P = 0.011) and the ibeA gene (9.1% in non-severe group, and 35.7% in severe group, P = 0.012) were significantly associated with severity as determined by univariable analysis (Table 4), whereas patient characteristics were not significantly associated with severity.
The distribution of the iutA and the ibeA genes according to sequence types is shown in Table 5. Only one isolate (ST429) was both iutA and ibeA-positive. The ST131 (n = 17) and the ST73 (n = 5) isolates were all iutA-positive. Among the ibeA-positive isolates (n = 14), ST95 accounted for 35.7%.
Discussion
We found that factors as DM with organ involvement and values of ALP were different in the two groups analyzed. Hyperglycemia due to DM, which is a metabolic disorder, impairs leucocyte functions [11, 12], and it has been shown that DM is related to the severity or mortality of sepsis [13, 14]. However, opposite results have also been reported, for example, septic patients with DM develop acute respiratory failure with less frequency [15], and DM is not associated with the mortality of Enterobacterales bacteremia [16]. Importantly, DM without complications was associated with the 30-days mortality caused by Staphylococcus aureus bacteremia, while DM with complications was not [17]. Overall, the mechanism and effect on the severity of bacteremia are not clear, and a more detailed analysis on DM and the immune response in bacteremia would be needed.
ALP levels, which are related with cholestasis, are elevated in acute biliary tract infection and in other diseases such as primary biliary cholangitis, primary sclerosing cholangitis, and non-hepatobiliary disease, in a clinical setting [18]. ALP was measured according to the method of the Japan Society of Clinical Chemistry [19], which differ from that of the International Federation of Clinical Chemistry and Laboratory Medicine. The Japanese method is influenced by ALP derived from the small intestine, and therefore the ALP values observed in the severe and non-severe might be influenced by this, affecting the accuracy of the determination. Here, the values of each ALP fractions were not measured due to the retrospective characteristics of the study.
Next, we found BEC mainly belonged to the B2 phylogroup, the most frequent group among extra-intestinal pathogenic E. coli [6]. The sequence types of the isolates were diverse; however, no differences were found between the non-severe and severe groups.
Acute biliary tract infections are caused by obstruction/stasis of biliary flow and influx of intestinal microorganisms. The human intestinal tract has been recognized as a reservoir of extraintestinal pathogenic E. coli strains, such as uropathogenic E. coli [20]. Once E. coli translocate into the biliary tract due to stasis/obstruction, acute biliary tract infections can occur and induce bacteremia.
The intestinal E. coli population are known to express many virulence factors. Some of these factors are needed for persistent colonization of the gut, for example, E. coli is resistant to the effects of bile [21]. In response to bile stress, both commensal and pathogenic E. coli strains, and especially enteropathogenic E. coli strains, activate stress response pathways [22, 23], efflux pumps [24], and production of toxins [25] in the gut. As there are high concentrations of bile acid in the biliary tract, resistance against bile might play an important role in pathogenicity.
In our study, other virulence factors needed during infection, such as those related with iron acquisition, adhesion, and invasion, were analyzed.
In the present study, the iutA gene was found at significantly lower frequency in the E. coli detected in the severe group than in those of the non-severe group.
The iutA gene encodes the aerobactin siderophore ferric receptor protein, facilitates iron acquisition by mediating the uptake of siderophores [26]. In a chicken infection model, iutA expression in extraintestinal pathogenic E. coli strains was at least 50-fold higher compared to in vitro grown bacteria [27]. In mammalian hosts, iron is tightly bound to various proteins, such as hemoproteins and ferritin [28], making free iron availability for pathogenic bacteria scarce. In biliary tract infections, bile is an iron-limiting environment [29]. Bile stress also causes increased expression of genes encoding virulence factors associated with iron scavenging in E. coli [30]. Therefore, E. coli strains harboring the iutA gene may become competitive in bile, 77.3% of the E. coli isolates from the non-severe group and approximately 50% of those from the severe group harbored the iutA gene.
It has been reported that iutA vaccine protect mice in a sepsis challenge model [31] and urinary tract infection model [32]. This may indicate that the iutA gene product might be easily recognized as an antigen by host immune systems, leading to the elimination of the E. coli strains harboring the iutA gene, in bile. Paradoxically, the iutA gene expression constitutes both an advantage and a disadvantage for E. coli as permits E. coli proliferation in the bile, but could also increase E. coli susceptibility to elimination as it can be recognized by the immune system. Excessive E. coli proliferation might cause an increase in inflammation and the patients might decline to a more severe condition. In this study, we analyzed E. coli isolates from blood cultures of patients with bacteremic biliary tract infection. We hypothesized that the lower frequency of the iutA gene in the isolates from the severe group might be due to the elimination of the iutA-expressing isolates by the immune system before they translocate to the blood. Further studies will be needed to accurately explain this hypothesis, as other virulence factors different than iutA might be needed for translocation through the barrier between bile and blood.
In contrast, E. coli strains containing the ibeA gene were found in a higher proportion in the severe group. The ibeA gene encodes a 50-kDa protein that participates in E. coli penetration in the microvascular endothelial cells of the human brain, allowing E. coli to cross the blood brain barrier. This virulence factor has an important role in neonatal meningitis [33, 34]. IbeA may also be essential for the invasion of intestinal epithelial cells and macrophages [35]. The ibeA-positive E. coli were detected among adherent-invasive E. coli isolates from pediatric Crohn's disease patients (positive rate: 81.8%) [36], bacteremic E. coli isolates that translocated from the gastrointestinal tract (27%) [37] and avian pathogenic E. coli isolates (26%) [38].
No information regarding the relationship between the ibeA and biliary tract epithelium cells has been reported; therefore, the mechanism by which the ibeA gene expression could contribute to the severity of acute biliary infection is unknown. However, it has been reported that E. coli in the gut can flood into the bile duct causing acute biliary tract infection, and that ibeA-positive E. coli strains show increased oxidative stress (H2O2) resistance [39] and persistence in macrophage [35]. These characteristics might be an advantageous as allows the proliferation of E. coli in the bile and confers oxidative stress resistance and the possibility to escape by gathering inside the macrophages and then passing into the blood.
IbeA inhibitors have been discovered to prevent invasion of human brain microvascular endothelial cells in vitro [40]. It would be worthwhile to investigate whether E. coli strains harboring ibeA can perform internalization, and whether ibeA is essential to invade from bile duct to vessels through in vitro experiments using ibeA inhibitors.
The prevalence of the iutA and the ibeA genes and related ST lineages were evaluated in this study. All the ST131 isolates were iutA-positive but ibeA-negative. ST131 is one of the major extraintestinal pathogenic E. coli global lineages and ST131 clade C epidemiologically emerged from clade B, approximately in the year 2002 [41]; a comparison between clades B and C showed that all clade B isolates were ibeA-positive, while all clade C were ibeA-negative [41]. Moreover, ibeA gene inactivation resulted in loss of early biofilm formation [41]. In Japan, ST131 clade C emerged around the year 2003 and by 2014, all the ESBL-producing ST131 isolates were from clade C [42]. As the isolates analyzed in this study were collected from 2013 to 2015, the ibeA prevalence among ST131 might have been affected by the epidemiological changes of clades but the rate of the ESBL-producers in our study was just 41.2% among the ST131 isolates. The proportion of ST lineage between the severe group and the non-severe group did not show differences and the relationship between ibeA prevalence and the severity of bacteremia was significant.
This study has several limitations. First, although cholangitis is a polymicrobial infection [3], we have investigated only one E. coli strain from each patient except for one patient without analyzing other E. coli strains found in the bile. This comparison might reveal whether ibeA-positive strains can more easily escape or invade into the blood compared to strains that remained in the bile. Second, this study was conducted at a single institution; a larger multi-center study is needed to assess potential bias in the epidemiology of phylogenetic patterns and virulence factors and to be able to detect statistically significant predictors. Third, the multivariable analysis of the data including both the iutA and the ibeA genes could not be performed because the sample size was too small for the analysis to be reliable.
Conclusion
We determined that several BEC isolates belonged to the virulent group B2 and presented diverse STs. In the E. coli isolates from the biliary tract of the severe group, the presence of the iutA gene was less frequent than in the non-severe group, while that of the ibeA gene was higher.
Methods
Patients
This retrospective study was conducted at the University of Tokyo Hospital, a 1217-bed tertiary-care teaching hospital in Tokyo, Japan. Patients with acute biliary tract infection who also had E. coli isolates detected in their blood were included in the study from April 2013 to February 2015. Each patient in this study was included only once, even if the patients repeatedly suffered E. coli bacteremia with acute biliary tract infection. Patient data, including clinical symptoms and microbiological data were collected from the medical records.
Data collection and definitions
Patient data collected included age, sex, underlying disease (diabetes mellitus, malignancy with or without metastasis, lymphoma, and collagen disease), use of immunosuppressants, biliary tract abnormalities, such as insertion of an intrabiliary stent or surgery for biliary carcinoma, gastrointestinal tract abnormalities and past history of acute biliary infection and bacteremia. Gastrointestinal tract abnormalities were defined as stenosis of the gastrointestinal tract, and history of surgery with change of gastrointestinal route. History of residence in a nursing home and antibiotic use within three months before onset of bacteremia was also noted. Collected patient laboratory data included white blood cell counts, platelet counts, total bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma glutamyltransferase (g-GTP), and C-reactive protein (CRP). Cases in which E. coli was detected from blood cultures obtained within 48 h after admission were defined as community acquired infection, while cases different from those were considered hospital acquired infections.
Biliary tract infection was defined according to the Tokyo guideline [43]. Cholangitis was defined in cases where all the following criteria were positive: (1) generalized inflammation sign such as fever (more than 38.0 °C), elevation of inflammation indicators in blood tests (white blood cell counts < 4000/μL or more than 10,000/μL, and C-reactive protein 1 mg/dL or more), (2) signs of bile stasis such as jaundice (total bilirubin 2 mg/dL or more), elevation of liver function and biliary function tests (more than one-and-a-half times of the upper limit for normal values for alkaline phosphatase, gamma-glutamyltransferase, aspartate aminotransferase, or alanine aminotransferase, normal range; ALP 106–322 U/L (measured by the method of the Japan Society of Clinical Chemistry[19]), g-GTP 13–64 U/L in men and 9–32 U/L in women, AST 13–30 U/L, ALT 10–42 U/L in men and 7–23 U/L in women, respectively), and (3) imaging of biliary tract abnormalities, such as dilatation of the biliary tract or the presence of a stent, and constriction. Cholecystitis was defined as: (1) localized clinical signs such as Murphy’s sign and pain in right upper abdomen, (2) generalized inflammation such as fever and elevation of inflammation indicators in blood tests, and 3) typical findings, such as acute cholecystitis with echocardiography or CT scan. Severity was divided using the Pitt bacteremia score [44] as severe (score of 2 or more) and non-severe (score < 2).
Microbiological procedures
All isolates were identified using the Walkaway system (Siemens, Berlin, Germany) or matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (using the MALDI Biotyper; Bruker Daltonik, Germany).
The classification of the E. coli isolates into phylogenetic groups, such as A, B1, B2, C, D, E, and F, was performed by quadruplex polymerase chain reaction (PCR) method, as described by Clermont et al. [45]. For identification of E. coli sequence types (STs) 69, 73, 95, and 131, frequently detected in bacteremic isolates [46], the multilocus sequence typing PCR method [47] was used. Then, the un-typable isolates by the PCR method sequenced [48] were typed according to the EnteroBase web resource [49]. The prevalence of 20 virulence factors (afaB and afaC, cnf1, cvaC, fimH, fyuA, hlyA, ibeA, iha, iroN, iucD, iutA, kpsMT2, ompT, papC, papG2, sat, sfaD & sfaE, tcpC, traT, and usp) was screened by multiplex PCR using extracted E. coli genomic DNA according to previous reports [50,51,52,53,54,55,56].
Statistical analysis
The two-tailed Fisher’s exact test was used for analysis of categorical data. Non-parametric data were analyzed using the Mann–Whitney U test. Values of P < 0.05 were considered significant. The variables that showed P < 0.05 in the virulence factor-encoding genes were entered a multivariable analysis using the multinomial logistic model. All statistical analyses were performed using JMP Pro version 11 software (SAS Institute, Cary, NC, USA).
Ethical considerations
This study was approved by the research ethics committee at the University of Tokyo Hospital. Obtaining written informed consent from each patient was waived because it was an observational retrospective study. The data were analyzed anonymously.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gu XX, Zhang MP, Zhao YF, Huang GM. Clinical and microbiological characteristics of patients with biliary disease. World J Gastroenterol. 2020;26(14):1638–46.
Kruis T, Guse-Jaschuck S, Siegmund B, Adam T, Epple HJ. Use of microbiological and patient data for choice of empirical antibiotic therapy in acute cholangitis. BMC Gastroenterol. 2020;20(1):65.
Weber A, Schneider J, Wagenpfeil S, Winkle P, Riedel J, Wantia N, et al. Spectrum of pathogens in acute cholangitis in patients with and without biliary endoprosthesis. J Infect. 2013;67(2):111–21.
Rerknimitr R, Fogel EL, Kalayci C, Esber E, Lehman GA, Sherman S. Microbiology of bile in patients with cholangitis or cholestasis with and without plastic biliary endoprosthesis. Gastrointest Endosc. 2002;56(6):885–9.
Leimbach A, Hacker J, Dobrindt U. E. coli as an all-rounder: the thin line between commensalism and pathogenicity. Curr Top Microbiol Immunol. 2013;358:3–32.
Sarowska J, Futoma-Koloch B, Jama-Kmiecik A, Frej-Madrzak M, Ksiazczyk M, Bugla-Ploskonska G, et al. Virulence factors, prevalence and potential transmission of extraintestinal pathogenic Escherichia coli isolated from different sources: recent reports. Gut Pathog. 2019;11:10.
Croxen MA, Finlay BB. Molecular mechanisms of Escherichia coli pathogenicity. Nat Rev Microbiol. 2010;8(1):26–38.
Lee JG. Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol. 2009;6(9):533–41.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–84.
Wang MC, Tseng CC, Chen CY, Wu JJ, Huang JJ. The role of bacterial virulence and host factors in patients with Escherichia coli bacteremia who have acute cholangitis or upper urinary tract infection. Clin Infect Dis. 2002;35(10):1161–6.
Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14(1):29–34.
Stegenga ME, van der Crabben SN, Blumer RM, Levi M, Meijers JC, Serlie MJ, et al. Hyperglycemia enhances coagulation and reduces neutrophil degranulation, whereas hyperinsulinemia inhibits fibrinolysis during human endotoxemia. Blood. 2008;112(1):82–9.
Laupland KB, Gregson DB, Zygun DA, Doig CJ, Mortis G, Church DL. Severe bloodstream infections: a population-based assessment. Crit Care Med. 2004;32(4):992–7.
Thomsen RW, Hundborg HH, Lervang HH, Johnsen SP, Schonheyder HC, Sorensen HT. Diabetes mellitus as a risk and prognostic factor for community-acquired bacteremia due to enterobacteria: a 10-year, population-based study among adults. Clin Infect Dis. 2005;40(4):628–31.
Esper AM, Moss M, Martin GS. The effect of diabetes mellitus on organ dysfunction with sepsis: an epidemiological study. Crit Care. 2009;13(1):R18.
Peralta G, Sanchez MB, Roiz MP, Garrido JC, Teira R, Mateos F. Diabetes does not affect outcome in patients with Enterobacteriaceae bacteremia. BMC Infect Dis. 2009;9:94.
Hansen MU, Gotland N, Mejer N, Petersen A, Larsen AR, Benfield T, et al. Diabetes increases the risk of disease and death due to Staphylococcus aureus bacteremia. A matched case–control and cohort study. Infect Dis (Lond). 2017;49(9):689–97.
Kwo PY, Cohen SM, Lim JK. ACG clinical guideline: evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112(1):18–35.
JSCC JSoCCc. JSCC document: recommendation for measuring enzyme activity in human serum (ALP). Jpn J Clin Chem. 1990;19:209–27.
Manges AR, Johnson JR. Reservoirs of extraintestinal pathogenic Escherichia coli. Microbiol Spectr. 2015;3(5).
Begley M, Gahan CG, Hill C. The interaction between bacteria and bile. FEMS Microbiol Rev. 2005;29(4):625–51.
Joffre E, Nicklasson M, Alvarez-Carretero S, Xiao X, Sun L, Nookaew I, et al. The bile salt glycocholate induces global changes in gene and protein expression and activates virulence in enterotoxigenic Escherichia coli. Sci Rep. 2019;9(1):108.
Rodriguez-Beltran J, Rodriguez-Rojas A, Guelfo JR, Couce A, Blazquez J. The Escherichia coli SOS gene dinF protects against oxidative stress and bile salts. PLoS ONE. 2012;7(4):e34791.
Rosenberg EY, Bertenthal D, Nilles ML, Bertrand KP, Nikaido H. Bile salts and fatty acids induce the expression of Escherichia coli AcrAB multidrug efflux pump through their interaction with Rob regulatory protein. Mol Microbiol. 2003;48(6):1609–19.
Bustamante P, Vidal R. Repertoire and diversity of toxin–antitoxin systems of Crohn’s disease-associated adherent-invasive Escherichia coli. New insight of this emergent E. coli pathotype. Front Microbiol. 2020;11:807.
Robinson AE, Heffernan JR, Henderson JP. The iron hand of uropathogenic Escherichia coli: the role of transition metal control in virulence. Future Microbiol. 2018;13:745–56.
Chouikha I, Bree A, Moulin-Schouleur M, Gilot P, Germon P. Differential expression of iutA and ibeA in the early stages of infection by extra-intestinal pathogenic E. coli. Microbes Infect. 2008;10(4):432–8.
Miethke M, Marahiel MA. Siderophore-based iron acquisition and pathogen control. Microbiol Mol Biol Rev. 2007;71(3):413–51.
Urdaneta V, Casadesus J. Interactions between bacteria and bile salts in the gastrointestinal and hepatobiliary tracts. Front Med (Lausanne). 2017;4:163.
Hamner S, McInnerney K, Williamson K, Franklin MJ, Ford TE. Bile salts affect expression of Escherichia coli O157:H7 genes for virulence and iron acquisition, and promote growth under iron limiting conditions. PLoS ONE. 2013;8(9):e74647.
Mellata M, Mitchell NM, Schodel F, Curtiss RR, Pier GB. Novel vaccine antigen combinations elicit protective immune responses against Escherichia coli sepsis. Vaccine. 2016;34(5):656–62.
Forsyth VS, Himpsl SD, Smith SN, Sarkissian CA, Mike LA, Stocki JA, et al. Optimization of an experimental vaccine to prevent Escherichia coli urinary tract infection. mbio. 2020;11(2).
Huang SH, Wan ZS, Chen YH, Jong AY, Kim KS. Further characterization of Escherichia coli brain microvascular endothelial cell invasion gene ibeA by deletion, complementation, and protein expression. J Infect Dis. 2001;183(7):1071–8.
Huang SH, Chen YH, Fu Q, Stins M, Wang Y, Wass C, et al. Identification and characterization of an Escherichia coli invasion gene locus, ibeB, required for penetration of brain microvascular endothelial cells. Infect Immun. 1999;67(5):2103–9.
Cieza RJ, Hu J, Ross BN, Sbrana E, Torres AG. The IbeA invasin of adherent-invasive Escherichia coli mediates interaction with intestinal epithelia and macrophages. Infect Immun. 2015;83(5):1904–18.
Conte MP, Longhi C, Marazzato M, Conte AL, Aleandri M, Lepanto MS, et al. Adherent-invasive Escherichia coli (AIEC) in pediatric Crohn’s disease patients: phenotypic and genetic pathogenic features. BMC Res Notes. 2014;7:748.
Mahjoub-Messai F, Bidet P, Caro V, Diancourt L, Biran V, Aujard Y, et al. Escherichia coli isolates causing bacteremia via gut translocation and urinary tract infection in young infants exhibit different virulence genotypes. J Infect Dis. 2011;203(12):1844–9.
Germon P, Chen YH, He L, Blanco JE, Bree A, Schouler C, et al. ibeA, a virulence factor of avian pathogenic Escherichia coli. Microbiology (Reading). 2005;151(Pt 4):1179–86.
Flechard M, Cortes MA, Reperant M, Germon P. New role for the ibeA gene in H2O2 stress resistance of Escherichia coli. J Bacteriol. 2012;194(17):4550–60.
Xu X, Zhang L, Cai Y, Liu D, Shang Z, Ren Q, et al. Inhibitor discovery for the E. coli meningitis virulence factor IbeA from homology modeling and virtual screening. J Comput Aided Mol Des. 2020;34(1):11–25.
Duprilot M, Baron A, Blanquart F, Dion S, Pouget C, Letteron P, et al. Success of Escherichia coli O25b:H4 sequence type 131 Clade C associated with a decrease in virulence. Infect Immun. 2020;88(12).
Matsumura Y, Pitout JDD, Peirano G, DeVinney R, Noguchi T, Yamamoto M, et al. Rapid identification of different Escherichia coli sequence type 131 Clades. Antimicrob Agents Chemother. 2017;61(8).
Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):41–54.
Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial Infections. Ann Intern Med. 2004;140(1):26–32.
Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep. 2013;5(1):58–65.
Kallonen T, Brodrick HJ, Harris SR, Corander J, Brown NM, Martin V, et al. Systematic longitudinal survey of invasive Escherichia coli in England demonstrates a stable population structure only transiently disturbed by the emergence of ST131. Genome Res. 2017;27:1437–49.
Doumith M, Day M, Ciesielczuk H, Hope R, Underwood A, Reynolds R, et al. Rapid identification of major Escherichia coli sequence types causing urinary tract and bloodstream infections. J Clin Microbiol. 2015;53(1):160–6.
Wirth T, Falush D, Lan R, Colles F, Mensa P, Wieler LH, et al. Sex and virulence in Escherichia coli: an evolutionary perspective. Mol Microbiol. 2006;60(5):1136–51.
Alikhan NF, Zhou Z, Sergeant MJ, Achtman M. A genomic overview of the population structure of Salmonella. PLoS Genet. 2018;14(4):e1007261.
Johnson JR, Brown JJ. A novel multiply primed polymerase chain reaction assay for identification of variant papG genes encoding the Gal(alpha 1–4)Gal-binding PapG adhesins of Escherichia coli. J Infect Dis. 1996;173(4):920–6.
Johnson JR, Stell AL. Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J Infect Dis. 2000;181(1):261–72.
Nakano M, Yamamoto S, Terai A, Ogawa O, Makino SI, Hayashi H, et al. Structural and sequence diversity of the pathogenicity island of uropathogenic Escherichia coli which encodes the USP protein. FEMS Microbiol Lett. 2001;205(1):71–6.
Ananias M, Yano T. Serogroups and virulence genotypes of Escherichia coli isolated from patients with sepsis. Braz J Med Biol Res. 2008;41(10):877–83.
Cirl C, Wieser A, Yadav M, Duerr S, Schubert S, Fischer H, et al. Subversion of Toll-like receptor signaling by a unique family of bacterial Toll/interleukin-1 receptor domain-containing proteins. Nat Med. 2008;14(4):399–406.
Rodriguez-Bano J, Mingorance J, Fernandez-Romero N, Serrano L, Lopez-Cerero L, Pascual A, et al. Virulence profiles of bacteremic extended-spectrum beta-lactamase-producing Escherichia coli: association with epidemiological and clinical features. PLoS ONE. 2012;7(9):e44238.
Dissanayake DR, Octavia S, Lan R. Population structure and virulence content of avian pathogenic Escherichia coli isolated from outbreaks in Sri Lanka. Vet Microbiol. 2014;168(2–4):403–12.
Acknowledgements
Not applicable.
Funding
This work was supported by JSPS KAKENHI Grant Number JP18K16171. The funding agencies did not have a role in the design of the study or the collection, analysis, and interpretation of data.
Author information
Authors and Affiliations
Contributions
MI designed this study, acquired and analyzed the patients’ data, and was a major contributor in writing the manuscript. MI and TK performed PCR to analyze virulence of E. coli. FF and TH identified and collected the E. coli strains. KT made database of bacteremia, YO, SO and KM revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee at the University of Tokyo Hospital. Obtaining written informed consent from each patient was waived because it was an observational retrospective study. The data were analyzed anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ikeda, M., Kobayashi, T., Fujimoto, F. et al. The prevalence of the iutA and ibeA genes in Escherichia coli isolates from severe and non-severe patients with bacteremic acute biliary tract infection is significantly different. Gut Pathog 13, 32 (2021). https://doi.org/10.1186/s13099-021-00429-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-021-00429-1