Abstract
Background
In Senegalese high-burden regions, the existing package of interventions is insufficient to reach the malaria elimination goal. Asymptomatic carriers of Plasmodium contribute significantly to malaria persistence and are not targeted by current interventions. The systematic treatment of all individuals in a community (mass drug administration, MDA) is a relevant intervention to tackle asymptomatic infections. The intervention can only be effective with a high participation of the population and, therefore, depends largely on its acceptability. This study aims to investigate the prospective acceptability of MDA in the Kedougou region to inform its potential use in a future strategy.
Methods
Following a 7-construct theoretical framework, prospective acceptability of MDA implemented in the rainy season was studied. In four villages, a sequential mixed design, from qualitative to quantitative, was used. In November 2021, interviews with healthcare professionals and focus groups with villagers were conducted. Findings from thematic analysis informed the development of a questionnaire administered to individuals aged ≥ 15 years in March 2022. Based on the questionnaire, an acceptability score was constructed and associations with socio-demographic factors were investigated using a linear mixed model.
Results
The 7 interviews, the 12 focus groups, and the questionnaire administered to 289 individuals demonstrated a good acceptability of MDA. Two potential barriers were identified: the contradiction of taking a medication without feeling sick and the occurrence of side effects; and four facilitators: the perception of malaria as a burden, a good understanding of MDA, a good perceived effectiveness, and the resulting economic benefits. The average acceptability score was 3.5 (range from -7 to + 7). Young adults aged 15 to 21 had a lower acceptability score compared to the other age groups, indicating an additional barrier to acceptability (β = -0.78 [-1.67;0.1]).
Conclusion
MDA is a priori acceptable to communities of Kedougou region in Senegal. Sensitization campaigns co-constructed with the communities, especially targeting young adults, are essential to ensure good acceptability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
In the last decades, Senegal made significant efforts to fight Plasmodium falciparum malaria, which remains a significant source of disease burden in three regions of the country [1, 2]. The strategy includes vector control and the use of rapid diagnostic tests (RDTs) and effective artemisinin-based combination therapy (i.e., artemether-lumefantrine) improved diagnosis and treatment, further strengthened by its deployment at community level (home-based case management or PECADOM) [1]. Additionally, seasonal malaria chemoprevention (SMC) for children under 10 years and intermittent preventive treatment (IPT) for pregnant women aim to prevent severe morbidity and mortality in these high-risk groups [3]. These interventions led to a 50% reduction in the mortality rate in a decade (from 4 deaths per 100,000 inhabitants in 2010 to 2 in 2021) [2, 4]. The prevalence among children under 5 years old decreased from 2.8% in 2012–2013 to 0.4% in 2017 [5, 6]. As a result, Senegal aims to eliminate malaria in 2030 [3]. Three regions (Kedougou, Kolda, Tambacounda) account for 80% of malaria cases, but represent only 11% of the national population [3]. The existing package of interventions needs to be reinforced in these three regions, where incidence stabilised in recent years [1, 2].
In Senegal, malaria is seasonal, with a high transmission period (from July to December in Kedougou) during the rainy season and a low transmission period during the dry season [3]. As in other settings, the persistence of Plasmodium parasites during low transmission seasons relies on asymptomatic carriers [7,8,9,10,11]. Several factors contribute to the development of asymptomatic carriage: transmission intensity, parasite (strain, multiplication rate), human intra-host (immunity, pyrogenic thresholds) and behavioural (health-seeking behaviour and access to healthcare) factors [12]. Asymptomatic carriers remain unaddressed by current strategies. Because they lack acute symptoms and harbour low density infections, they are rarely tested in routine and field tests are usually not sensitive enough to detect their infections (> 80% of infections detected by PCR remain undetected by microscopy or RDT) [13, 14]. Targeting asymptomatic carriage could contribute to reducing transmission. Addressing all Plasmodium infections beyond clinical cases is also a required step in the shift from malaria control to elimination.
Mass drug administration (MDA) is a possible intervention to treat asymptomatic infections [15]. It consists in a systematic treatment of all individuals of a community, regardless of the presence of malaria symptoms. MDA has proven effective in reducing malaria transmission in The Gambia and Myanmar and is recommended by the World Health Organization (WHO) to accelerate malaria elimination in low transmission settings [15,16,17,18]. The Senegalese National Malaria Control Programme considers implementing MDA in moderate to low prevalence regions, including Kedougou. A cluster randomised controlled trial was conducted in 2021 in Tambacounda region to evaluate the effectiveness of MDA to reduce carriage prevalence [19]. However, the effectiveness of this intervention depends largely on the participation of the population. A prerequisite is therefore to propose an acceptable intervention for the community.
Acceptability is a multifaceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experiential responses to the intervention [20]. Acceptability differs from the concept of adherence, which reflects the extent to which a person’s behaviour corresponds to the recommendations from a health care provider [21]. MDA acceptability varies across locations due to socio-cultural factors, beliefs, or experiences with the disease [22,23,24,25]. The aim of this study was to assess the prospective acceptability of MDA (i.e., without prior experience of the intervention) in the Kedougou region of Senegal.
Methods
Context of the study
The Kedougou region, in South Eastern Senegal, carries the largest malaria burden in the country (Fig. 1) [2, 3]. The acceptability study was nested within the MARS (Malaria Asymptomatic Reservoir in Sahel) cohort, which aimed to describe the reservoir of asymptomatic P. falciparum infections during the 2021–2022 epidemiological year (from 13 April 2021 to 30 March 2022). In Senegal, the MARS cohort was conducted in four villages (Baraboye, Hamady Herry, Ibel and Thiabedji), which presented high malaria incidence and active, motivated community health workers. They also presented different levels of accessibility to roads and to healthcare facilities and hosted diverse ethnic groups (Fulani or Malinke). The primary source of income in these villages is agriculture, mainly maize, cotton, or millet cultivation.
Study area in Kedougou region in Senegal. Sources: Geo Senegal Database 2023, Google Earth 2023 [51]. Author: EL
Description of the theoretical intervention: MDA in rainy season
The acceptability of a potential MDA intervention, which would be implemented during the rainy season, was studied. The season during which MDA is implemented defines its characteristics (aim, number of rounds, period of activity), which may influence its acceptability. The rainy season was chosen over the dry season because it coincided with the high transmission period and aligned with the protocol proposed by the randomized clinical trial in Tambacounda [19]. Recent MDA studies usually relied on dihydroartemisinin-piperaquine (DP) anti-malarial treatments, which involved a daily oral dose over three days and provided a prophylactic effect for one month [16, 17, 26]. Typical adverse event observed during DP-based MDA were nausea and vomiting [17, 18]. Implementing MDA during the rainy season requires conducting multiple monthly rounds to ensure that participants benefit from the prophylactic effect throughout the entire high transmission season [17]. In the following text, "MDA" will refer to the intervention involving monthly rounds of 3-day DP administered to the entire community over the high transmission season.
Study design
A sequential exploratory mixed-methods design from qualitative (QUAL) to quantitative (QUAN) method was used (Fig. 2). This article was written following the guidelines of the Mixed Methods Appraisal Tool [27]. In the QUAL component, MDA acceptability was studied among different subgroups of the population to inform the development of the QUAN questionnaire. The QUAN component aimed to measure the overall acceptability of the intervention in the youth and adult population. To provide clear information about the rationale and principles of the intervention, the questionnaire included descriptive images improved with QUAL findings.
The theoretical framework of acceptability
The theoretical framework of acceptability of healthcare interventions of Sekhon et al. was used [20]. This framework defines acceptability by seven constructs, which were adapted to the study and context: affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness, and self-efficacy.
Data collection instruments
MDA acceptability was assessed through focus groups with different subgroups of the population and interviews with healthcare professionals (QUAL). The QUAL study investigated MDA acceptability by gathering insights from individuals receiving and implementing the intervention. Population acceptability was measured using a QUAN acceptability questionnaire constructed based on findings from the focus group and interviews (QUAL → QUAN).
Focus groups
An interview guide for the focus groups was developed based on the conceptual framework of Sekhon et al. The focus groups were conducted from 21 to 26 November 2021 (i.e., during the rainy season) in the MARS study villages. Community health workers recruited participants using convenience sampling based on their availability (considering the ongoing harvest season) and proximity to the meeting location [28]. Villagers included in the MARS cohort were excluded from participation. To mitigate power dynamics, focus groups were structured by gender and age subgroups: male or female adults (i.e., aged 20 and above) and male or female young adults (i.e., under 20 years). Three focus groups were conducted per village: one with adult women, one with adult men and one with young adults (alternating between men and women). Each focus group included 10 participants, resulting in a total of 120 participants. A Senegalese sociologist and an experienced interpreter residing in the region conducted the focus group in Fula and Malinke. Audio recordings were made after obtaining oral consent from all participants.
Interviews
Using a specific interview guide based on the conceptual framework of Sekhon et al., seven interviews were conducted with healthcare professionals implementing malaria control strategies (community health workers, nurses from health posts, malaria control agents). Participants were selected through convenience sampling based on their proximity to the study villages. The interviews took place on 10 and 11 November 2021 in an office provided by health posts and were conducted in French by a French epidemiologist. Following oral consent from the participants, interviews were recorded.
Questionnaire construction
The quantitative questionnaire consisted of closed-ended questions with responses based on the Likert scale. Descriptive images and explanatory texts explaining the rationale and principles of MDA preceded the questions. The construction of the questionnaire involved four main steps:
-
(1) Development of the initial QUAN questionnaire in French: based on the conceptual framework of Sekhon et al. and a previous acceptability questionnaire, eight questions were formulated (one for general acceptability and one for each construct) [29]. Two images and a short paragraph were created to explain the concept of asymptomatic carriers and the principle of MDA.
-
(2) Improvement of the QUAN questionnaire based on QUAL findings: during focus groups, descriptive images were first presented, followed by the explanatory text. The aim was to evaluate image clarity, consistency with the text, and obtain suggestions for representation improvement. The complete QUAN questionnaire (closed-ended questions and descriptive images) was presented during interviews with healthcare professionals. The questionnaire was assessed for understandability and acceptability, and feedback was sought on whether any questions should be added or removed.
-
(3) Translation of the questionnaire into Fula and Malinke: trained research assistants living in the region translated the questionnaire. A first group of research assistants (two individuals for each language) translated the questionnaire from French to Fula or Malinke. A second group of research assistants, who only received the Fula or Malinke version, translated it back to French without prior knowledge of the original French version. Discrepancies observed allowed for corrections [30].
-
(4) Questionnaire testing during interviews with community members: the questionnaire was tested in two neighbouring villages independent of the MARS cohort: one Fulani and one Malinke (Fig. 1). In each village, a trained interviewer fluent in both local languages administered the questionnaire face-to-face, while an observer took notes on the villagers' reactions and comments. The community health worker recruited three villagers: a young adult, a woman and a man. The villagers were asked about the clarity of the images and questions. This testing phase allowed to (i) rephrase questions that were not sufficiently understandable, (ii) remove a question representing the affective attitude construct that was not understood, (iii) change the Likert scale from 5 to 3 responses (disagree, don't know, agree), (iv) reduce the number of images, and (v) improve the administration of the questionnaire.
The final questionnaire consisted of seven closed-ended questions: one for general acceptability and one for each construct of the conceptual framework (excluding affective attitude) (Fig. S1). One image explaining the principle of MDA accompanied the questions (Fig. S2).
Questionnaire administration
The questionnaire was administered during the dry season, from 21 to 30 March 2022, to members of households participating in the MARS cohort. Briefly, these 66 households were randomly selected in April 2021 from the Bandafassi Demographic and Health Surveillance System population census [31]. Household members who provided informed consent were included in the cohort and had been followed for 12 months at the time of the acceptability study. Experienced research assistants, fluent in local languages, administered the questionnaire face-to-face to all participants aged 15 years and older and staying for > 1 night in the household. Research assistants received training on both acceptability questionnaire and theoretical MDA intervention before administration. There were no exclusion criteria. The questionnaire included acceptability questions and collected socio-demographic information (age, sex, education) and household characteristics (construction materials, access to water, assets). The responses were collected on paper and then entered into a database by a trained and experienced operator.
Mobility monitoring
Community health workers conducted weekly household visits to document participant mobility on paper registers. Mobility was defined as spending at least one night away from the household. A trained operator then entered information into an Excel database.
Clinical malaria cases monitoring
Community health workers documented participants' clinical malaria cases, confirmed by RDTs, on paper registers between April 2021 and March 2022. A trained operator then entered information into an Excel database.
Analysis
Qualitative analysis
Following transcription of the audio recordings into French, a thematic content analysis was conducted based on the seven constructs of the theoretical framework of acceptability [32]. Focus group and interview analyses were carried out independently by the sociologist and the epidemiologist. A subsequent cross-analysis of the results was performed.
Quantitative analysis
Based on the questionnaire responses, an acceptability score was constructed: a value of + 1 was attributed to responses in favour of acceptability, 0 to “don't know” and -1 to responses against acceptability. The acceptability score ranged from −7 to + 7.
Questionnaire responses were combined with individual data from MARS cohort participants: age, gender, the highest level of education, history of clinical malaria episodes confirmed by RDT in the last rainy season, and the mean number of weeks per month spent away from the village during the last rainy season as an indicator of mobility. Descriptive data were available to characterize participants' households, including construction materials, access to water, and assets. A socio-economic variable was constructed from these household variables through hierarchical clustering, preceded by multiple component analysis [33, 34].
Factors associated with MDA acceptability score were analysed using a multilevel linear regression model with random intercepts at village and household levels. Analyses were conducted using R 4.0 and mgcv, FactoMineR and factoextra packages [35].
Integration of the results
The findings from the QUAL and QUAN components were listed and compared to identify concordant, discordant, or specific results to either the QUAN or QUAL analysis [36, 37].
Ethics and consent to participate
The National Ethics Committee for Health Research of Senegal approved the protocol of the MARS cohort study (N°0000052/MSAS/DPRS/CNERS) and a protocol amendment detailing the present acceptability study (N°000187/MSAS/CNERS/SP). Written informed consent was obtained from all participants before their participation in any research activity. A literate individual witnessed each consent. For participants under 18 years old, we obtained written informed consent from a parent or a legal guardian. Oral consent was obtained from all participants in the focus groups and interviews prior to their participation, witnessed by community health workers.
In the context of high malaria burden in Kedougou, where rumours can impact villagers' trust and participation in malaria control interventions, special attention was given to inform participants that this study focused on the acceptability of an intervention that had not yet been planned.
The results of this study were presented to villagers from the four study villages. This dissemination was done through a workshop organized and facilitated by a Senegalese sociologist who spoke Fula or with the assistance of an interpreter speaking Malinke. Workshops were organized according to age and gender (male, female, < 20 years, and ≥ 20 years) to facilitate participation and discussion.
Results
Qualitative findings
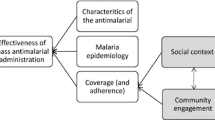
According to focus groups with villagers and interviews with healthcare professionals, MDA during the rainy season was well accepted. The reasons for this acceptability can be summarized in Fig. 3 based on their influence (green = favourable; red = unfavourable).
Villagers exhibited a clear understanding of the principle of MDA during the rainy season and the existence of asymptomatic carriers. The resonance with their own personal experiences enhanced this understanding.
“I am going to tell you a story: I was feeling fine, nothing wrong with me, I went to village S in search of work and they asked me to take a malaria test and when I did it, they told me I had malaria, the result was positive, even though I didn't have any symptoms. It’s just to show that you can actually have malaria without showing any signs.” – Man, focus group (FG).
The villagers understood the similarities between MDA and SMC interventions, which helped to understand MDA principles. They did not confuse the two interventions: SMC is indicated for children under 10 years old, whereas MDA encompasses all individuals in the village. MDA can be seen as an “expanded SMC” to the entire population.
“That's a really good idea. Before, we used to have SMC campaigns only for children, forgetting that, yes, the elderly are also here. Maybe they are the ones who are asymptomatic carriers and keep transmitting the disease to the children. And the fight that you're undertaking is a good fight. Now we'll be relieved to hear that, yes, SMC will cover the entire population and all households.” – Man, FG.
Another factor contributing to high acceptability was the cost–benefit balance, enhanced by the recognition of curative and prophylactic benefits of the MDA treatment.
“[I accept] To avoid getting infected without knowing it, when you take the treatment, it can serve as prevention or treatment if you are infected without knowing it.” – Young woman, FG.
Acute malaria can hinder working, especially physical farm labour. While diagnosis and treatment of uncomplicated malaria is available at community level with free testing and anti-malarial medicine, expenses related to treatment of severe cases or transportation to healthcare facilities remain. The economic gains resulting in participation in MDA were also perceived as a benefit.
“This is a very good idea, it's a very good strategy. I believe that during the rainy season, the amount we spend to treat family members who have malaria is a colossal expense.” – Man, FG.
Having to spend a morning at home instead of going to the fields to wait for the health worker’s delivery of anti-malarial treatment was a cost associated with participation in MDA. Yet, this cost did not appear to impact acceptability. The benefits of the anti-malarial treatment, particularly its prophylactic effect, outweighed this cost, enabling individuals to continue their economic activities.
“With good sensitization, we are ready to wait for the health worker on the day of his visit. It is in our best interest because it will help us protect ourselves against the disease.” – Woman, FG.
The belief that MDA effectively prevents malaria cases supported the perceived benefits of the intervention. Villagers observed a decrease in malaria cases among children receiving SMC and drew a parallel between SMC and MDA effectiveness.
“I believe there is an example because since we started giving medicine to children, we have noticed that they no longer have malaria, so, this is a clear example that we should use, based on the effectiveness of SMC in preventing malaria in children.” – Man, FG.
Despite these facilitating factors, opinions diverged when considering the entire village population would participate in MDA. Some participants were confident that all villagers would participate in the intervention, while others had a more nuanced opinion and identified certain categories of people, especially the elderly, who might be reluctant to participate.
“Not everyone will accept, the grandfathers for example.”—Young woman, FG.
Participants mentioned several reasons for refusals. They underlined the contradiction between taking medication and not feeling sick.
“No, I won't accept taking medication without being sick. (...) Since I'm not sick, I won't take any medication. I won't be motivated to take the medication.” - Young man, FG.
“I think the grandfathers will refuse because they will believe that they are not sick.” - Young woman, FG
The side effects of anti-malarial treatments could also limit participation in the intervention. This barrier came from the villagers' experiences during SMC.
“Some people will refuse because during the SMC campaigns, some children took tablets and experienced side effects, such as the child being less active, feeling sluggish, and having diarrhoea.” - Man, FG.
There is a synergistic effect linking the contradiction of taking medication without obvious malaria symptoms to the occurrence of side effects due to medication intake.
“Some people will also refuse because they believe that taking tablets without being sick will make them vomit. And vomiting will make them sick.” - Woman, FG.
To minimise refusals, participants emphasised the importance of sensitization to explain the concept of asymptomatic carriers, the principle of MDA and its benefits. In this context, sensitization referred to community mobilisation and education during public meetings addressed to the entire population.
“It requires sensitization and making people understand that there are asymptomatic carriers who are present and transmit the disease to others without knowing. Now, we need to sensitise them to tell them the importance of the project.” - Man, FG.
During interviews, healthcare professionals shared their personal opinions on the acceptability of MDA for both themselves and the population. From their professional perspective, MDA is an acceptable intervention. Consistent with the findings from focus groups, this acceptability was due to a good understanding of the intervention, which was seen as an “expanded SMC” for the entire population, and a good perceived effectiveness resulting from previous SMC campaigns. Healthcare professionals also believe that implementing MDA would benefit them by reducing malaria cases in the month following treatment, thereby alleviating their workload.
“No, it's not a problem because it's just one round during the month. It doesn't pose much of a problem because if you've reached everyone, it means less work for you in terms of malaria cases at the clinic.”—Healthcare professional, interview (I).
Additionally, taking an anti-malarial drug in the absence of symptoms was acceptable for healthcare professionals because of the prophylactic effect.
“[I would accept taking an antimalarial treatment even if I'm not sick.] Yes, if it's for prevention.”—Healthcare professional, I.
When healthcare professionals evaluated the acceptability of MDA from the population's perspective, they highlighted the economic benefits, consistently with focus groups findings. They also referred to the heavy malaria burden in the villages, a highly prevalent disease, potentially severe or even fatal, causing significant suffering among the population.
“Well, I don't think it will be a problem because malaria causes a lot, a lot, a lot of damage.”—Healthcare professional, I.
The occurrence of side effects was also perceived as a barrier. This burden was emphasized by the cost associated to the treatments to manage side effects.
“The mother refuses, saying 'If the child gets sick, I will be the one spending my money. So, I prefer not to give it to him.”—Healthcare professional, I.
The main barrier to acceptability anticipated by both the population and healthcare professionals was the population's lack of understanding of the intervention's principle. Rumours against health interventions could exacerbate this issue.
“Due to the rumours, some people will see it differently. ‘These are not treatments for malaria. These are treatments provided by them, for this or that [purpose].’ It's like the corona pandemic [...] until now, some people doubt the vaccine. Maybe that will be the problem.”—Healthcare professional, I.
Like the population, healthcare professionals repeatedly suggested sensitization as a solution to overcome this barrier.
“If people are willing to listen to those who are sensitising them, with sensitization and communication, I think it can really satisfy them.”—Healthcare professional, I.
Quantitative results
In March 2022, out of the 637 participants attending the final MARS cohort visit, 306 individuals were aged 15 or older. Complete acceptability data was available for 289 individuals (95%) (Fig. 4). Participants had an average age of 36 years, with a majority of women (57%) (Table 1). Nearly half of the participants had no formal education (54%), a quarter completed primary school (23%), and a fifth completed secondary school (18%). A quarter of the participants (23%) reported a history of diagnosed malaria in 2021. Most participants did not travel during the 2021 rainy season. The households were classified into four socio-economic profiles (Figs. S3 and S4).
The overall acceptability of MDA was good, with 91% of participants declaring that they would agree to take the treatment during the rainy season (Q.1, 91% agreed, n = 266). This acceptability can be attributed to the perceived effectiveness of the intervention (Q.7, 93% agreed, n = 272), the perceived benefits of the intervention during the rainy season due to the prophylactic effect of the treatment (Q.4, 91% agreed, n = 266), and the low cost in terms of time required to participate in the intervention (Q.5, 88% agreed, n = 256). Yet, half of the participants indicated that they would refuse to participate due to concerns about side effects (Q.2, 48% agreed, n = 144), and 41% were reluctant to take a treatment without feeling sick (Q.6, 41% agreed, n = 134). Lastly, more than half of the participants were uncertain about the participation of the entire population in the village (Q.3, 55% declared “I don’t know”, n = 160) (Fig. 5).
The average acceptability score was 3.5 (95% CI [3.1, 3.8], range: −7 to + 7). Although the difference was not significant according to first order risk of 0.05, young adults aged 15 to 21 had a lower score compared to other age groups (β = −0.78 [−1.67;0.1]). Acceptability score was two points lower for women with primary education (β = −2 [−3.32; −0.75]) compared to women with lower or higher education achievements and to men. Participants who had a history of RDT-confirmed malaria during the previous rainy season had a 0.66-point higher acceptability score (95% CI [0.02; 1.31]) compared to those who did not have malaria. Mobility outside the village during the rainy season and the socioeconomic level of the household were not associated with the acceptability score (Table 1).
Integration of QUAL and QUAN findings
The results of both QUAL and QUAN studies supported MDA acceptability (Table 2). The questionnaire, developed based on interviews and focus groups, confirmed and generalized determinants in favour of acceptability: the perceived effectiveness of MDA due to SMC experience and the overall benefits, such as prophylaxis, outweighed time cost. It also highlighted the same barriers as the QUAL study: mixed trust in the participation of the entire population, the burden of side effects, and the inconsistency between taking medication and the absence of symptoms. Of note, two constructs of acceptability (affective attitude and intervention coherence) could only be studied in the QUAL surveys.
The QUAN analysis quantified several factors associated with lower acceptability, particularly age. The lower acceptability among young adults aged 15–21 years was consistent with the focus group findings: young adults were the only ones expressing clearly their refusal to participate. The QUAN analysis also identified specific determinants that were not studied in QUAL, such as the effect of a history of malaria or women with primary education. Finally, while focus groups participants repeatedly expressed the idea that elderly individuals were likely to refuse the intervention, elderly participants in the QUAN study did not present a lower acceptability score compared to the other age groups.
Discussion
This study demonstrated that MDA during the rainy season was acceptable to the population and healthcare professionals in Kedougou. The contradiction between taking medication and not feeling sick, and the potential occurrence of side effects, were the main barriers identified. The time dedicated to the intervention interfering with professional activities generating incomes and domestic work represented a cost for the participants. Yet, four facilitating factors balanced this cost: (i) the perception of malaria as a burden and suffering for the population, (ii) a good understanding of the intervention, (iii) the good perceived effectiveness of MDA to prevent malaria, and (iv) the resulting economic benefits due to reduced healthcare expenses and improved ability to engage in professional activities due to better health.
Inadequacy with the representation of care has been identified as a barrier in two prospective acceptability studies of MDA in Zambia and Namibia [24, 38]. The occurrence of side effects was frequently observed as an obstacle to participation, but only in retrospective acceptability studies [23,24,25, 38,39,40,41,42,43]. Facilitating factors, such as understanding the concept of asymptomatic carriers and the prophylactic benefits of the intervention, were previously associated with better acceptability in prospective acceptability studies [24, 38]. Recognizing malaria as a significant health problem, understanding the concept of the intervention, and believing that the intervention would have a beneficial effect, particularly economically, were factors only identified in retrospective studies [42, 43]. It is hypothesized in this study that previous experience with SMC in children enabled participants to project themselves more realistically in the potential intervention, and thus highlighting factors found in both prospective and retrospective studies. This study is the first to report MDA acceptability in a context of SMC implementation. Interestingly, MDA interventions against neglected tropical diseases such as lymphatic filariasis were also implemented in 2021 in Kedougou region, but participants did not draw a parallel with these interventions [44].
Socio-demographic determinants of acceptability
Two population subgroups with lower acceptability were identified: young adults aged 15 to 21 and women with primary education. Few studies have examined the acceptability of young adults under the age of 18. A retrospective acceptability study in The Gambia identified 18–25-year-olds as having lower participation or adherence to MDA due to their occupational mobility [23]. This study pointed at a different reason: the contradiction between having to take medication while not feeling sick. During the feedback workshops, the feeling of invincibility due to youth or engagement in sports activities and religious fatalism were also mentioned as reasons for the lower acceptability. This age group likely is a major contributor to malaria persistence: young adults aged 15 to 21 represent 15% of the population, experience 25% of clinical malaria cases, and 34% are asymptomatic carriers during the rainy season [45]. Yet, young adults are not targeted by specific malaria control strategies, which focus on high-risk populations (children under 10 years and pregnant women). Their participation to MDA is likely a key element of success, and special attention should be given to their acceptability.
Women with primary education also presented lower acceptability. During the feedback workshops, women of all ages were questioned about their understanding of this result. They mentioned, regardless of their level of education, that women are responsible for household duties such as cleaning, meal preparation, and childcare. Women who cannot be replaced or seconded in their household may refuse to participate out of fear that disabling side effects would hinder the completion of these essential tasks. Knowledge about the potential side effects caused by anti-malarial treatment and free and easy access to treatments managing side effects could address this barrier.
Acceptability among individuals aged > 45 years
The results of this study were inconsistent regarding the acceptability of older individuals. Participants in focus groups, who tended to be younger than 45, repeatedly suggested that elderly people may present lower acceptability. Several reasons were mentioned in the QUAL study and feedback workshops: i) the contradiction between taking medication and not feeling sick, ii) reliance on traditional medicine, or iii) their role in household duties. Yet, the quantitative study did not reveal a lower acceptability score among individuals over 45 years old.
The literature also provides conflicting results regarding the acceptability and participation of older individuals in MDA [24, 25, 41, 46]. Either participants in the QUAL study mistakenly anticipated the behaviour of older individuals, or older individuals may be less likely to express their refusal to participate during the questionnaire. A more in-depth study of the acceptability among older individuals is necessary because, even though they represent a small proportion of the general population (< 5% are over 60 years old), they often have a role as opinion leaders, particularly men, due to their status as heads of households.
Mobility
Mobility during the previous rainy season was not identified as a determinant of acceptability. Yet, retrospectively, mobility was identified as the primary barrier to participation in the MDA trial in The Gambia [47]. This discrepancy could be explained by the fact that the rainy season corresponds to the agricultural season when travel frequency is low.
From sensitization to community engagement
Villagers and healthcare professionals mentioned repeatedly that sensitization was an essential activity to ensure good acceptability of MDA. Sensitization sessions can provide information about the concept of asymptomatic carriage, the principles of the intervention and its benefits, which are facilitating factors. It can also help address two barriers: inform and justify taking preventive medication despite the absence of symptoms and help to distinguish medication side effects from other symptoms and their management. Additionally, sensitization could prevent and address rumours that can have a detrimental effect on participation [48]. Prospective and retrospective studies all highlight the importance of sensitization and underline how the perception of having receive sufficient information about the intervention is a major driver of acceptability [23, 38, 39]. These sensitization sessions need to be conducted repeatedly before and during the intervention through various communication channels (including community meetings, door-to-door visits, radio) [40].
Sensitization aimed specifically towards young adults and women responsible for household duties could address the reasons for their lower acceptability. Sensitization campaigns construct collaboratively with and through communities could address young adults and women barriers to participation [49, 50]. It could help to identify relevant knowledge and messages to be address and suitable communication channels adapted to each subgroup of the population [43, 44]. Numerous studies highlight the importance of community engagement in MDA acceptability [25, 42, 43, 46].
Strengths and limitations of the study
This research is the first to study MDA acceptability prospectively by combining a sequential QUAL > QUAN exploratory mixed methods design with the theoretical framework of Sekhon et al. and presents a robust and reproducible methodology to study the prospective acceptability. This methodology was applied to a large sample and yielded meaningful results relative to the local context and to the existing literature, improving the understanding of acceptability drivers and the identification of population subgroups reluctant to participate.
Studying acceptability prospectively faces a clear limit: stated intentions might differ significantly from actual behaviours. A pre-post-acceptability study of MDA indicated that initially, 26% of participants expressed reluctance to participate in the MDA intervention [22]. In this study, the long-term implementation of SMC in the region over nearly 10 years likely enabled participants to realistically envision the proposed intervention, highlighting drivers of acceptability that were previously only explored in retrospective studies.
Another limit stems from the need to rely on face-to-face interviews to administer questionnaires in a context of low literacy, which is a known source of social desirability bias. However, questionnaires were administered by local research assistants who were not health personnel.
Finally, during the cohort study, sensitization addressed to all inhabitants were conducted regarding the concept of asymptomatic carriage within the villages, but were generally attended to by heads of households. These individuals may have developed a better understanding of asymptomatic carriage, which is a facilitating factor for acceptability of intervention. Acceptability may therefore be overestimated in QUAL and QUAN components. The lesser acceptability among young adults and women, may also highlight cohort participants least exposed to these messages.
Conclusion
MDA for malaria was acceptable for the population in Kedougou in Senegal. Sensitization activities are essential to ensure good acceptability and maximize the participation of the population in MDA. Specifically, young adults exhibited a lower acceptability while they represent a key population subgroup for local malaria dynamics. It is, therefore, important to engage them and the entire community in the design of future elimination interventions.
Availability of data and materials
Data are available upon request from the corresponding author.
Abbreviations
- RDTs:
-
Rapid diagnostic tests
- SMC:
-
Seasonal malaria chemoprevention
- IPT:
-
Intermittent preventive treatment
- MDA:
-
Mass drug administration
- QUAL:
-
Qualitative
- QUAN:
-
Quantitative
- FG:
-
Focus group
References
WHO. World malaria report 2023. Geneva: World Health Organization; 2023.
National Malaria Control Programme – Senegal. Annual epidemiological bulletin 2021 on malaria in Senegal. Available from: Unpublished data
National Malaria Control Programme, Ministry of Health and Social Action. National Strategic Plan for Malaria Control in Senegal 2021–2025. Dakar, 2020. https://senegal-cocreation.com/wp-content/uploads/2021/02/PSN_PNLP_Senegal_Version-finale_-Fevrier-2021.pdf. Accessed 2 Sep 2024.
National Malaria Control Programme – Senegal. Annual epidemiological bulletin 2019 on malaria in Senegal. 2020. https://pnlp.sn/bulletin-epidemiologique-annuel/. Accessed 2 Sep 2024.
National Agency of Statistics and Demography. Senegal: Continuous Demographic and Health Survey (DHS) 2017. Dakar, 2018. https://dhsprogram.com/publications/publication-fr345-dhs-final-reports.cfm.Accessed 2 Sep 2024.
National Agency of Statistics and Demography. Malaria indicator survey (MIS) in Senegal 2020–2021. Dakar, 2022. https://dhsprogram.com/publications/publication-MIS38-MIS-Final-Reports.cfm. Accessed 2 Sep 2024.
Ahmad A, Mohammed NI, Joof F, Affara M, Jawara M, Abubakar I, et al. Asymptomatic Plasmodium falciparum carriage and clinical disease: a 5-year community-based longitudinal study in the Gambia. Malar J. 2023;22:82.
Tadesse FG, van den Hoogen L, Lanke K, Schildkraut J, Tetteh K, Aseffa A, et al. The shape of the iceberg: quantification of submicroscopic Plasmodium falciparum and Plasmodium vivax parasitaemia and gametocytaemia in five low endemic settings in Ethiopia. Malar J. 2017;16:99.
Coulibaly D, Travassos MA, Tolo Y, Laurens MB, Kone AK, Traore K, et al. Spatio-temporal dynamics of asymptomatic malaria: bridging the gap between annual malaria resurgences in a Sahelian Environment. Am J Trop Med Hyg. 2017;97:1761–9.
Babiker HA, Abdel-Muhsin AM, Ranford-Cartwright LC, Satti G, Walliker D. Characteristics of Plasmodium falciparum parasites that survive the lengthy dry season in eastern Sudan where malaria transmission is markedly seasonal. Am J Trop Med Hyg. 1998;59:582–90.
Zwetyenga J, Rogier C, Spiegel A, Fontenille D, Trape JF, Mercereau-Puijalon O. A cohort study of Plasmodium falciparum diversity during the dry season in Ndiop, a Senegalese village with seasonal, mesoendemic malaria. Trans R Soc Trop Med Hyg. 1999;93:375–80.
Galatas B, Bassat Q, Mayor A. Malaria parasites in the asymptomatic: looking for the hay in the haystack. Trends Parasitol. 2016;32:296–308.
Benié EMA, Silué KD, Ding XC, Yeo I, Assamoi JB, Tuo K, et al. Accuracy of a rapid diagnosis test, microscopy and loop-mediated isothermal amplification in the detection of asymptomatic infections in Korhogo. Northern Côte d’Ivoire Malar J. 2022;21:111.
Wang B, Han SS, Cho C, Han JH, Cheng Y, Lee SK, et al. Comparison of microscopy, nested-PCR, and Real-Time-PCR assays using high-throughput screening of pooled samples for diagnosis of malaria in asymptomatic carriers from areas of endemicity in Myanmar. J Clin Microbiol. 2014;52:1838–45.
WHO. Global malaria programme a framework for malaria elimination. Geneva: World Health Organization; 2017.
Landier J, Parker DM, Thu AM, Lwin KM, Delmas G, Nosten FH, et al. Effect of generalised access to early diagnosis and treatment and targeted mass drug administration on Plasmodium falciparum malaria in Eastern Myanmar: an observational study of a regional elimination programme. Lancet. 2018;391:1916–26.
Dabira ED, Soumare HM, Conteh B, Ceesay F, Ndiath MO, Bradley J, et al. Mass drug administration of ivermectin and dihydroartemisinin–piperaquine against malaria in settings with high coverage of standard control interventions: a cluster-randomised controlled trial in The Gambia. Lancet Infect Dis. 2022;22:519–28.
von Seidlein L, Peto TJ, Landier J, Nguyen TN, Tripura R, Phommasone K, et al. The impact of targeted malaria elimination with mass drug administrations on falciparum malaria in Southeast Asia: a cluster randomised trial. PLoS Med. 2019;16: e1002745.
ClinicalTrials.gov. Study Details - Mass drug administration of dihydroartemisinin-piperaquine + single low-dose primaquine to accelerate toward elimination activitiesClinicalTrials.gov. Accessed on September 2, 2024. https://clinicaltrials.gov/study/NCT04864444
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17:88.
WHO. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Aung PL, Soe MT, Soe TN, Oo TL, Aung PP, Khin A, et al. The acceptability of targeted mass treatment with primaquine for local elimination of vivax malaria in a northern Myanmar township: a mixed-methods study. Parasit Vectors. 2021;14:549.
Fehr A, Nieto-Sanchez C, Muela J, Jaiteh F, Ceesay O, Maneh E, et al. From informed consent to adherence: factors influencing involvement in mass drug administration with ivermectin for malaria elimination in the Gambia. Malar J. 2021;20:198.
Roberts KW, Smith Gueye C, Baltzell K, Ntuku H, McCreesh P, Maglior A, et al. Community acceptance of reactive focal mass drug administration and reactive focal vector control using indoor residual spraying, a mixed-methods study in Zambezi region. Namibia Malar J. 2021;20:162.
Galatas B, Nhantumbo H, Soares R, Djive H, Murato I, Simone W, et al. Community acceptability to antimalarial mass drug administrations in Magude district, Southern Mozambique: a mixed methods study. PLoS ONE. 2021;16: e0249080.
Chotsiri P, Zongo I, Milligan P, Compaore YD, Somé AF, Chandramohan D, et al. Optimal dosing of dihydroartemisinin-piperaquine for seasonal malaria chemoprevention in young children. Nat Commun. 2019;10:480.
Mixed Methods Appraisal Tool (MMAT) Version 2018 User Guide | NCCMT. https://www.nccmt.ca/knowledge-repositories/search/232%20(accessed%20May%202017. Accessed 2 Sep 2024.
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42:533–44.
Louart S, Hedible GB, Ridde V. What is acceptability of health innovations? Example of pulse oximeter integrated into PCIME management in primary health centers in West Africa. Dakar, Senegal; 2015.
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104.
Pison G, Douillot L, Kante AM, Ndiaye O, Diouf PN, Senghor P, et al. Health & demographic surveillance system profile: bandafassi health and demographic surveillance system (Bandafassi HDSS). Senegal Int J Epidemiol. 2014;43:739–48.
Ritchie J, Spencer L. Qualitative data analysis for applied policy research analyzing qualitative data. Oxfordshire: Routledge; 1994.
Garenne M. Traditional Wealth, modern Goods, and demographic Behavior in Rural Senegal. World Dev. 2015;72:267–76.
Coste M. The poor and the healthy: unpacking health capability in rural Senegal. Working paper. 2023;
R: The R Project for Statistical Computing. https://www.r-project.org/. Accessed 18 Aug 2023.
Kaur N, Vedel I, El Sherif R, Pluye P. Practical mixed methods strategies used to integrate qualitative and quantitative methods in community-based primary health care research. Fam Pract. 2019;36:666–71.
Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res. 2006;16:377–94.
Silumbe K, Finn TP, Jennings T, Sikombe C, Chiyende E, Hamainza B, et al. Assessment of the acceptability of testing and treatment during a mass drug administration trial for malaria in Zambia using mixed methods. Am J Trop Med Hyg. 2020;103(2):28–36.
Peto TJ, Tripura R, Sanann N, Adhikari B, Callery J, Droogleever M, et al. The feasibility and acceptability of mass drug administration for malaria in Cambodia: a mixed-methods study. Trans R Soc Trop Med Hyg. 2018;112:264–71.
Dial NJ, Ceesay SJ, Gosling RD, D’Alessandro U, Baltzell KA. A qualitative study to assess community barriers to malaria mass drug administration trials in the Gambia. Malar J. 2014;13:47.
Nguyen TN, Thu PNH, Hung NT, Son DH, Tien NT, Van Dung N, et al. Community perceptions of targeted anti-malarial mass drug administrations in two provinces in Vietnam: a quantitative survey. Malar J. 2017;16(1):17.
Wanzira H, Naiga S, Mulebeke R, Bukenya F, Nabukenya M, Omoding O, et al. Community facilitators and barriers to a successful implementation of mass drug administration and indoor residual spraying for malaria prevention in Uganda: a qualitative study. Malar J. 2018;17:474.
Adhikari B, Phommasone K, Kommarasy P, Soundala X, Souvanthong P, Pongvongsa T, et al. Why do people participate in mass anti-malarial administration? findings from a qualitative study in Nong District, Savannakhet Province, Lao PDR (Laos). Malar J. 2018;17:15.
Fuller BB, Harris V, Parker C, Martinez A, Toubali E, Ebene BC, et al. Contextual determinants of mass drug administration performance: modelling fourteen years of lymphatic filariasis treatments in West Africa. PLoS Negl Trop Dis. 2023;17: e0011146.
Landier J. Seasonal dynamics of Plasmodium falciparum asymptomatic reservoir in Sahelian Africa. Bangkok, Thailand: The Royal Society London; 2022.
De Martin S, von Seidlein L, Deen JL, Pinder M, Walraven G, Greenwood B. Community perceptions of a mass administration of an antimalarial drug combination in The Gambia. Trop Med Int Health. 2001;6:442–8.
Dierickx S, Gryseels C, Mwesigwa J, O’Neill S, Bannister-Tyrell M, Ronse M, et al. Factors associated with non-participation and non-adherence in directly observed mass drug administration for malaria in The Gambia. PLoS ONE. 2016;11: e0148627.
Peto TJ, Debackere M, Etienne W, Vernaeve L, Tripura R, Falq G, et al. Community participation during two mass anti-malarial administrations in Cambodia: lessons from a joint workshop. Malar J. 2018. https://doi.org/10.1186/s12936-018-2202-z.
Tangseefa D, Monthathip K, Tuenpakdee N, König A, Kajeechiwa L, Thwin MM, et al. ‘Nine Dimensions’: a multidisciplinary approach for community engagement in a complex postwar border region as part of the targeted malaria examination in Karen/Kayin State. Myanmar Wellcome Open Res. 2018;3:116.
Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee Task, Force on the Principles of Community Engagement. Principles of Community Engagement. 2nd Edn. 2011. (NIH Publication). https://www.atsdr.cdc.gov/communityengagement/index.html. Accessed 2 Sep 2024.
Géo Sénégal. Digital Elevation Model 30 m. https://www.geosenegal.gouv.sn/-Modeles-numeriques-de-terrain-30-m-.html. Accessed 2 Sep 2024.
Acknowledgements
We would like to express our deep gratitude to all the participants in this study, as well as the entire population of the villages of Thiabedji, Ibel, Hamady Herry, and Baraboye, for their involvement in this project and their continuous support in the fight against malaria. Their warm welcome has been invaluable. We would like to extend our special thanks to Moussa Ba, Sadio Kante, Moussa Sadiakhou, Ousmane Camara, and the nurses at the health posts in Bandafassi and Thiabedji, whose support and dedication have been crucial to the success of this project. We are also grateful to all the research assistants for their commitment to this study. Lastly, we express our deep appreciation to Professor Adama Faye, the director of ISED, for graciously hosting EL at the institute and for his essential contribution to securing ISSPAM funding. We also thank Fatoumata Bintou Balde for her implication in the dissemination workshops.
Funding
The project leading to this publication has received funding from the Excellence Initiative of Aix-Marseille University—A*MIDEX, a French “Investissements d’Avenir” programme: the MARS project (A*Midex International 2018). EL was supported by an individual grant from the French government under the France 2030 investment plan, as part of the Initiative d'Excellence d'Aix-Marseille Université—A*MIDEX—Institute of Public Health Sciences of Aix-Marseille (AMX-20-IET-014).
Author information
Authors and Affiliations
Contributions
EL, VR, and JL conceived the study objectives and the methodological approach, and secured funding for the study. EL developed the interview guide for interviews with healthcare workers, conducted them, transcribed the audio recordings, and realised the thematic analysis. EL and AN developed the interview guide for focus groups with the population with contribution of NMS. AN conducted the focus group discussions with an interpreter, transcribed the audio recordings, and realised the thematic analysis under the supervision of NMS. EL conducted the cross-analysis of individual interviews and focus group discussions. EL, AN, VR, JL, EB and NMS interpreted the qualitative findings. EL, VR, and JL designed the quantitative questionnaire. EL improved the questionnaire based on the qualitative findings. VR and JL reviewed the questionnaire. EL organised and supervised the translation of the quantitative questionnaire and conducted the questionnaire pre-testing with the assistance of a trained interviewer. EL and JL trained the interviewers and supervised the administration of the quantitative questionnaire. EL supervised the data entry for the quantitative data. EL, VR, JL, and JG designed the quantitative data analysis plan. EL conducted the quantitative analyses. EL, VR, JL, EB, and JG interpreted the quantitative findings. EL created the figures and drafted the initial version of the article. All authors reviewed the article and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12936_2024_5078_MOESM1_ESM.docx
Additional file 1: S1 Figure. Acceptability questionnaire in Fulaand in Malinke. S2 Figure. Descriptive images and explanatory text supporting the questionnaire. S3 Figure. Construction of the household socio-economic variable. A) Results of the multiple correspondence analysis. B) Dendrogram. C) Results of the hierarchical cluster analysis. S4 Figure. Description of households’ socio-economic categories. The lowest standard of living category represented households with thatched roofs and earthen walls, with few equipment except for transportation, and little external financial assistance from family members. The intermediate standard of living category corresponded to households with cement floors, corrugated iron roofs, or cement walls. They had more equipment such as private car and beds. In this category, the proportion of households receiving external financial assistance from family members was higher. The classification distinguished two types of agricultural households: those with small cattle only, and those with both small cattle and cows
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Legendre, E., Ndiaye, A., Sougou, N.M. et al. Prospective acceptability of mass drug administration for malaria in Kedougou region in Senegal: a mixed method study. Malar J 23, 279 (2024). https://doi.org/10.1186/s12936-024-05078-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-05078-8