Abstract
Background
Carriers of persistent asymptomatic Plasmodium falciparum infections constitute an infectious reservoir that maintains malaria transmission. Understanding the extent of carriage and characteristics of carriers specific to endemic areas could guide use of interventions to reduce infectious reservoir.
Methods
In eastern Gambia, an all-age cohort from four villages was followed up from 2012 to 2016. Each year, cross-sectional surveys were conducted at the end of the malaria transmission season (January) and just before the start of the next one (June) to determine asymptomatic P. falciparum carriage. Passive case detection was conducted during each transmission season (August to January) to determine incidence of clinical malaria. Association between carriage at the end of the season and at start of the next one and the risk factors for this were assessed. Effect of carriage before start of the season on risk of clinical malaria during the season was also examined.
Results
A total of 1403 individuals—1154 from a semi-urban village and 249 from three rural villages were enrolled; median age was 12 years (interquartile range [IQR] 6, 30) and 12 years (IQR 7, 27) respectively. In adjusted analysis, asymptomatic P. falciparum carriage at the end of a transmission season and carriage just before start of the next one were strongly associated (adjusted odds ratio [aOR] = 19.99; 95% CI 12.57–31.77, p < 0.001). The odds of persistent carriage (i.e. infected both in January and in June) were higher in rural villages (aOR = 13.0; 95% CI 6.33–26.88, p < 0.001) and in children aged 5–15 years (aOR = 5.03; 95% CI 2.47–10.23, p = < 0.001). In the rural villages, carriage before start of the season was associated with a lower risk of clinical malaria during the season (incidence risk ratio [IRR] 0.48, 95% CI 0.27–0.81, p = 0.007).
Conclusions
Asymptomatic P. falciparum carriage at the end of a transmission season strongly predicted carriage just before start of the next one. Interventions that clear persistent asymptomatic infections when targeted at the subpopulation with high risk of carriage may reduce the infectious reservoir responsible for launching seasonal transmission.
Similar content being viewed by others
Background
Although malaria burden across sub-Saharan Africa has decreased significantly over the last two decades owing to the scale-up of control interventions [1, 2], malaria transmission has not been interrupted in most endemic areas despite high coverage of control interventions [3]. In endemic settings where clinical immunity to malaria is maintained, a high proportion of infections are clinically silent [4, 5] and, therefore, tend to persist untreated [6]. Such infections remain a constant source of infection to mosquitoes, thus maintaining transmission and hindering control efforts and the progress towards malaria elimination [7, 8].
In the Sahel sub-region, Plasmodium falciparum remains the predominant malaria species [9] with transmission occurring mainly during and around the 3 to 4 wet season months and almost ceasing during the long dry season due to diminished mosquito population [10, 11]. A subset of individuals infected at the end of each transmission season however could remain infected without any symptom for several months of the dry season until the start of the following wet season [12], when they probably infect newly emerging mosquitoes thus initiating the yearly seasonal malaria transmission in the community [6, 12]. Across different transmission settings, only few studies have assessed the dynamics of persistent P. falciparum carriage [13, 14], thus the extent of carriage and characteristics of carriers are not defined in most endemic areas. As these would likely vary according to the transmission setting [13], identifying risk factors or subgroups associated with persistent P. falciparum carriage specific to each setting could guide the targeting of interventions to reduce the human reservoir of infection.
Chronic carriage of multiclonal asymptomatic P. falciparum infections has been shown to confer protection against subsequent episodes of clinical malaria [15,16,17,18,19], probably being the result of exposure-dependent enhancement of acquired immunity [20]. Therefore, while clearing persistent asymptomatic infections with effective treatment would reduce the infectious reservoir and possibly transmission, it may increase the risk of clinical malaria in individuals cleared of infection [21]. Nevertheless, other studies have reported an increased risk of clinical malaria in chronic asymptomatic carriers [22,23,24]. These discordant findings suggest the effect of chronic asymptomatic carriage on protective immunity may vary by transmission setting.
In eastern Gambia, persistent carriage of asymptomatic P. falciparum infections, associated risk factors and the effect of carriage on clinical malaria was assessed.
Methods
Study setting and participants selection
The malaria burden in The Gambia has decreased significantly over the last 20 years [9, 25], although there is still substantial and heterogeneous residual transmission, particularly in the eastern part of the country [26]. Transmission is almost exclusively by P. falciparum species and highly seasonal occurring mainly during the rainy season between July to October and shortly after (November to December) [26]. Several control interventions are routinely implemented by the National Malaria Control Programme, namely insecticide-treated nets (ITN), indoor residual spraying (IRS), intermittent preventive treatment during pregnancy (IPTp) and prompt diagnosis and treatment with artemisinin-based combination therapy (ACT); seasonal malaria chemoprevention (SMC) for children 3–59 months old was introduced in 2014.
In the Upper River Region (URR) in eastern part of the country, four villages were selected by convenience sampling: Gambissara (GMB) with a population of about 13,000 (henceforth referred to as semi-urban village) and three smaller villages surrounding it namely Sare-Bondo (SBD), Fula Morie-Boche (FMB) and Sare-Jawbeh (SJB) with approximate populations of 200, 340 and 150, respectively (henceforth collectively referred to as rural villages). In the semi-urban village, compounds were selected randomly from a list of compounds in the ongoing health demographic surveillance system (HDSS) while in the rural villages all compounds were invited to participate. Within selected compounds, approximately 10 individuals were selected by simple random sampling. Individuals that consented (plus assent if applicable) were enrolled and assigned a unique study identification number and an identification card bearing the participant’s photo and study number. Infants less than 6 months old were excluded from the selection.
Study conduct
Between 2012 and 2016, two cross-sectional surveys per year in relation to the malaria transmission season were carried out: one just before start (June) and the other at the end (January) of the season (for the year 2016, start of season survey was not conducted due to logistical challenges). Only individuals enrolled into the study were sampled at every survey; demographic and clinical information which included history of fever and symptoms suggestive of clinical malaria in the previous 48 h and at time of survey was collected using a structured questionnaire. Axillary temperature was measured by a digital clinical thermometer. A malaria rapid diagnostic test (RDT) (SD Bioline®) was performed for participants with suspected clinical malaria based on clinical assessment and if positive were treated according to the national guidelines.
A blood sample was collected by fingerpick for microscopy and for measuring haemoglobin. Thick blood films were stained with 2.5% buffered Giemsa (PH 7.2) for 10–15 min, dried and read independently by two microscopists. If a slide was positive, parasites were counted against 500 white blood cells (WBCs) and parasite densities estimated assuming 8000 WBC per µl. Slides were considered negative after examining 200 high power fields. If the estimation of the parasite count between the two independent microscopists differed by ≥ 20% or if readings were discrepant for positivity, a third microscopist resolved the discrepancy. Asymptomatic P. falciparum carriage was defined as asexual parasitaemia of any density detected by microscopy without symptoms suggestive of clinical malaria within the previous 48 h or at time of assessment during survey. Haemoglobin was measured using a HemoCue® photometer (Ångelholm, Sweden) according to manufacturer’s instruction. A study clinic in the health centre of the study area was established where all study participants sought medical care for any illness during the study period. During each malaria transmission season (August to January), a passive case detection (PCD) system was established where suspected cases of clinical malaria were clinically assessed and systematically screened with malaria RDT (SD Bioline®). Positive cases were treated according to the national treatment guidelines. Usage of ITN was assessed by asking all participants attending the study clinic, regardless of their illness, if they had slept under an ITN the previous night.
Sample size
Sample size was based on desired precision for malaria prevalence at the end of the season (January). Assuming this would range between 5 and 10% in the semi urban village and 15% and 20% in the rural villages based on previous pilot survey (Okebe et al., pers. commun.), 1000 individuals in the semi-urban village allowed for estimation of prevalence with the following precisions: 5% (95% CI 3.7–6.5%), 10% (95% CI 8.2–12.0%) and 200 individuals in the rural villages with the precision of 15% (95% CI 10.4–20.7%), 20% (95% CI 14.7–26.2%).
Data management and statistical analysis
Data were collected onto paper-based case report forms (CRFs) and then double entered in Studytrax (© Sciencetrax LLC, USA) data base. Consistency checks were carried out, data entry errors and discrepancies verified and corrected prior to statistical analysis which was performed using STATA software version 16.0 (Stata Corp, College Station, Texas, USA). Age was categorized into three groups: < 5 years, 5–15 years and > 15 years; anaemia was defined as Hb < 13.0 g/dl. Severity of anaemia was defined as follows: mild (Hb: 11.0–12.9 g/dl), moderate (Hb: 8.0–10.9 g/dl), and severe (Hb: < 8.0 g/dl) [27]. Descriptive statistics are presented for continuous variables (medians and interquartile range) and proportions for categorical variables. Point estimates are presented with 95% confidence intervals. Malaria prevalence was estimated as the proportion of positive participants by microscopy at each survey and incidence as risk of clinical malaria per 1000 cohort population per transmission season. Evidence of linear trend for prevalence of malaria infection from 2012 to 2016 was assessed. Owing to failed convergence of log-binomial regression models, a mixed effects logistic regression model was used to examine the association between carriage at the end of a season and before start of the next one and to determine independent predictors for persistent carriage (i.e. infected both at the end of a season and at the start of the next one). Mixed effects Poisson regression model was used to determine the association between P. falciparum carriage before start of the season and incidence of clinical malaria during the following season and to assess effect measure modification of this association by village setting. The relationship between clinical malaria during the season and risk of carriage at the end of the season was assessed using mixed effects logistic regression. Regression analyses were performed from pooled data for the years 2012 to 2015. All models account for clustering at household level and repeated measurement on subjects allowing for random effects at both levels.
Ethical considerations
This study was approved by the Gambian Government/MRC Joint Ethics Committee (SCC1256). Written informed consent was obtained from all participants; parents/guardians provided written consent for children less than 18 years old. Written assent in addition to parental consent was obtained from children aged between 12 and 17 years.
Results
Description of study population
In June 2012, a total of 1403 individuals were enrolled into the cohort—1154 from the semi-urban village (GMB) and 249 from the three rural villages (SBD, FMB and SJW) combined. Age distribution was similar between the semi-urban and the rural villages. However, ethnic group composition differed, with semi-urban village inhabited mostly by Serahules and the rural villages exclusively by Fulas. Females were more represented in the cohort, particularly in the semi-urban village (Table 1).
Malaria prevalence before start and at the end of transmission seasons
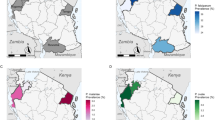
Malaria prevalence both just before the start and at the end of the transmission season was consistently higher in the rural villages. Prevalence at the end of the transmission season declined between 2012 and 2016, both in the semi-urban village (from 10.7 to 3.2%) and in the rural villages (from 35.2 to 19.9%) although there was an increase in 2015 within this decline. Overall, prevalence of P. falciparum infection at the end of the transmission season showed declining trend over the 5-year study period in both the semi-urban (p < 0.001) and the rural villages (p = 0.002). Remarkably, prevalence before start of the transmission season did not show such declining trend (Fig. 1). Prevalence of infection was consistently higher in the 5–15 years age group, both in the semi-urban and rural villages (Fig. 2). Asexual parasite density tended to be higher in the rural villages (Additional file 1: Appendix S1). Proportion of infected individuals at start of season (June) that harboured gametocytes ranged between 0 and 15.0% in the semi-urban village and between 2.2 and 10.5% in the rural villages (Additional file 1: Appendix S2). Coverage at surveys (proportion of total cohort sampled) ranged between 77.1 and 99.1% and was always slightly higher in the rural villages (Additional file 1: Appendix S3).
Trend analysis for malaria prevalence at the end and before start of the transmission seasons by village setting. Error bars correspond to 95% confidence interval for estimated prevalence. P values calculated from test for trend of odds of malaria infection. For the year 2016, data was not collected at the start of the season
Prevalence of asymptomatic P. falciparum malaria by age groups before the start (June) and at end (January) of the transmission seasons. 2012 (abbreviated as 12) to 2016 (abbreviated as 16). Note: (i) For the year 2016, data was not collected at the start of the season. (ii) There are few participants in the < 5 years age group at end of season 2015 survey due to aging of participants over the years of follow up. Additional participants for this age category only were enrolled at end of 2016 survey (Additional file 1: Appendix S7)
In the semi-urban village, compounds with infected individuals just before start of the transmission season varied over the study period (i.e. changed every year); only 1.1% (1/95) of compounds consistently had infected individual(s) at all the four start of season surveys. In the rural villages, 37% (10/27) of compounds consistently had at least one infected individual at every start of season survey particularly in FMB and SJB (Additional file 1: Appendix S4).
The proportion of individuals that reported sleeping under an ITN the previous night during the transmission season estimated from attendees of the PCD clinic over the 5-year study period was slightly higher in the semi-urban (93.8%) than the rural villages (84.8%) (Additional file 1: Appendix S5).
Plasmodium falciparum carriage at end of a season and before start of the following season
The proportion of individuals that carried infection at the end of a transmission season and just before start of the next one for the transmission years 2012 to 2015 (i.e. positive at end of 2012 season and at start of 2013, positive at end 2013 and at start of 2014, positive at end 2014 and at start of 2015) was higher in the rural villages each year (Fig. 3). Similarly, majority (95%) of those who carried malaria infection at the end of a season and at start of the next season for more than one year (i.e. multiple years) were from the rural villages. Mixed effect logistic regression analysis from combined data for the years 2012 to 2015 showed a strong association between parasite carriage at the end of the transmission season and at just before start of the next season (OR = 35.04: 95% CI 22.19–55.31; p < 0.001), even after adjusting for age, gender, anaemia, village setting and transmission year (aOR = 19.99; 95% CI 12.57–31.77, p < 0.001). The odds of persistent carriage (i.e. carriage both at the end of the season and at start of the next one) were significantly higher in the rural villages compared to the semi-urban village (aOR = 13.0; 95% CI 6.33–26.68; p < 0.001). Compared to other age groups, children 5–15-year-old had the highest odds of persistent carriage (aOR = 5.03; 95% CI 2.47–10.23; p < 0.001) (Table 2).
Clinical malaria and association with asymptomatic P. falciparum carriage
Incidence of clinical malaria was higher in the rural villages than in the semi-urban village over the study period. Generally, incidence tended to decrease over the study period although there was an increase in 2015 in all study villages (Additional file 1: Appendix S5). Village setting modified the effect of carriage at the start of the season on risk of clinical malaria during the season (p = 0.002 for interaction term carriage-village). While there was no association between carriage at start of the season and risk of clinical malaria during the season in both crude analysis (IRR 1.27, 95% CI 0.83–1.94, p = 0.251) and after adjusting for age, gender, years and village setting (IRR 0.81, 95% CI 0.53–1.24, p = 0.348) when rural and semi-urban villages were combined, analysis stratified by village setting showed that parasite carriage before start of the transmission season tended to be associated with a higher risk of clinical malaria during the ensuing season in the semi-urban village (IRR 1.83, 95% CI 0.98–3.42, p = 0.055). Conversely, in the rural villages, parasite carriage just before start of the season was significantly associated with a lower risk of clinical malaria (IRR 0.48, 95% CI 0.27–0.81, p = 0.007) (Table 3). At the compound level, there was no association between asymptomatic carriage in a compound just before start of the season and the risk of subsequent clinical malaria in the same compound, both in the semi-urban (IRR 1.13, 95% CI 0.98–1.30, p = 0.076) and in the rural villages (IRR 0.99, 95% CI 0.88–1.10, p = 0.907).
Concerning the risk of asymptomatic carriage at the end of the season after a clinical episode during that season, the association again differed by village setting. In the semi-urban village, the risk of carriage was higher in individuals who had clinical malaria in the preceding transmission months, both in the crude analysis (OR 2.17; 95% CI 1.37–3.42, p < 0.001) and after adjustment for age and gender (aOR 2.09; 95% CI 1.32–3.29, p < 0.001). In the rural villages, this association was reversed as the risk of carriage was significantly lower in individuals who had a clinical malaria in the preceding transmission months both in the crude analysis (OR 0.43; 95% CI 0.24–0.77, p = 0.005) and after adjustment for age, gender and years (aOR 0.39; 95% CI 0.22–0.69, p < 0.001) (Table 4).
Discussion
This study assessed asymptomatic P. falciparum carriage at the end of a malaria transmission season and at start of the next one, the risk factors for this and the relationship between carriage and clinical malaria in neighbouring villages of differing transmission intensity. Microscopically patent asymptomatic carriage at the end of the malaria season (January) was strongly associated with carriage just before start of the next season (June); it was estimated that among those infected in January, up to one third in the semi-urban and half in the rural villages could carry infections up to June, when rains usually start, heralding the start of a new malaria transmission season. However, considering infections were identified by microscopy, an important proportion of asymptomatic carriers with sub-patent infections may have been missed [28]. A study conducted in a lower transmission area within the same region that used molecular tests on samples collected monthly during the dry season and, therefore, able to detect sub-patent infections, found that 40% of individuals infected in December remained positive including sub-patent infections until the end of the dry season in May [13]. In the current study, given the known fluctuation of parasitaemia in malaria-infected individuals [28] and the expected decrease in parasite density from partial spontaneous clearance [29], some of those positive in January but negative in June could have been infected at sub-patent level undetectable by microscopy. Therefore, the estimated proportion of individuals that carried infection at the end of a transmission season and at the start of the next one (persistent carriage) reported in this study has probably been underestimated.
The odds of persistent carriage were much higher in rural villages compared to the semi urban village, an observation possibly explained by the higher parasite densities in rural villages which have been shown to persist for longer [29, 30]. Furthermore, given the relatively higher transmission intensity in the rural villages, most infections may have been multiclonal [20], which have been associated with longer persistence [13, 23, 31]. Compared to other age groups, children aged 5–15 years had the highest odds of persistent carriage. This can possibly be due to age-dependent acquisition of immunity that enables older children in endemic areas to tolerate but not eliminate malaria infections [32,33,34]. Odds of carriage tended to be lower in adults; given that anti-parasite immunity increases with age [34], a faster spontaneous clearance of asymptomatic infections has been observed in adults [29, 35] which could explain this observation. The observed higher odds of persistent carriage in children aged 5–15 years, coupled with the relatively higher exposure of this age group to mosquito bites [36], suggest they probably are major contributors to the initiation of the yearly seasonal malaria transmission in this setting.
The proportion of infected individuals with microscopically patent gametocytes, the parasite stage required for human to mosquito transmission, detected just before start of season was similar to that reported amongst clinical cases during the transmission season [37]. A much higher proportion of gametocyte positive asymptomatic infections has been reported from studies carried out during the dry season that used sensitive molecular diagnostic methods [13, 38]. Remarkably, up to 80% of infections carried to the end of the dry season harboured gametocytes in the study by Collins et al. [13]. Even though gametocyte transmissibility was not assessed in these studies, the findings nonetheless suggest that infections carried through the dry season can potentially infect mosquitoes.
Parasite carriage just before start of the transmission season was associated with the risk of clinical malaria during the following season. However, the direction of such a risk differed between the semi-urban and rural villages. While in the semi-urban village carriage just before start of the season was associated with an increased risk of clinical malaria during the following season, such a risk was decreased in rural villages, a result similar to what has been described in an area of intense transmission of Mali, where individuals with asymptomatic multiclonal infections during the dry season had significantly lower risk of clinical malaria in the following season [17]. Similarly, an earlier study from a high transmission setting in Tanzania observed that baseline multiple infection tended to confer protection against subsequent clinical malaria in older but not in younger children and attributed this to exposure-dependent acquisition of immunity [39]. However, in moderate transmission settings of Senegal [15] and Kenya [31], asymptomatic carriage at the start of the transmission season was associated with an increased risk of clinical malaria as observed in the semi-urban village of the current study. A recent systematic review and pooled analysis of studies concluded that the relationship of asymptomatic infections and risk of subsequent clinical malaria depends on age and transmission intensity; with increasing age, there is a reduced risk in high transmission settings and an increased risk in low to moderate transmission settings [33].
Clinical malaria during the transmission season was associated with the risk of asymptomatic carriage at the end of the season (January); it was significantly lower in rural villages but higher in semi-urban village. Repeated exposure to many heterologous strains in rural villages where transmission is relatively higher would have resulted in an expanded repertoire of relevant memory effector cells, priming the immune system to effectively clear subsequent new infections [20, 40]. In addition, the rural villages were exclusively inhabited by the Fula (Fulani) ethnic group that has been shown to genetically exhibit hyper immune response to P. falciparum when exposed [41, 42]. It is also important to point out that infection status was determined by microscopy, therefore, the risk of carriage refers to infection with a relatively high density, detectable by microscopy. Molecular analysis may have provided completely different results as individuals in high and moderate transmission settings may carry very low-density infections. On the other hand, the asymptomatic infections detected after a clinical malaria episode in the semi-urban village may be residual or recrudescent parasitaemia after treatment as has been observed in similar settings [6].
Malaria prevalence at the end of the transmission season declined over the 5-year surveillance period in both the semi-urban and rural villages. This coincided with a relative increased abundance of Anopheles arabiensis in the study area (Jawara et al., pers. commun.), a relatively less efficient vector for malaria transmission, which may have contributed to decline in transmission. Findings from recent nationwide entomological survey in The Gambia confirmed predominance of An. arabiensis in eastern Gambia over other more efficient vector species [43]. The high coverage of ITNs and IRS which primarily target indoor vector biting in eastern Gambia for an extended period [26] may have exerted selection pressure towards outdoor biting species as observed in Kenya [44] and Senegal [45].
There are a few limitations to consider. Microscopy as diagnostic method has probably underestimated the malaria prevalence and thus the estimated persistence of carriage. In addition, given that microscopy detected infections with a relatively high parasite density while molecular diagnostic methods would have identified low density infections, some of the associations reported above would have been modified had sub-patent infections been included in the analysis. Secondly, in determining persistent carriage, parasitaemia by microscopy was measured at two time points only (i.e. January and June). Even though there is only a remote chance of acquiring a new infection between January and June in this setting, more frequent sampling over the dry season with use of genotyping techniques could have ruled out possibility of new infections with greater certainty. Finally, data on coverage and usage of malaria control interventions was not systematically collected over the 5-year period which limited the interpretation of the study findings in relation to control interventions.
Conclusions
A significant proportion of individuals infected with malaria at the end of the transmission season carried infection at the start of the following season; carriage was higher amongst children 5–15 years old and in the rural villages. The highly seasonal nature of transmission in this setting suggests such infections persisted throughout the intervening dry season and probably contributed to initiating the next seasonal transmission. Interventions that clear persistent infections when targeted at subpopulations with higher risk of persistent carriage could reduce the malaria infectious reservoir before the emergence of mosquitoes at the start of the rains and may supress the launch of the seasonal malaria transmission in the communities.
Availability of data and materials
The data used or analyzed in this study are available from the corresponding authors upon reasonable request with approval from the Gambia Government/MRC Joint Ethics Committee.
Abbreviations
- ACT:
-
Artemisinin-based combination therapy
- aOR:
-
Adjusted odds ratio
- CRFs:
-
Case report forms
- Hb:
-
Haemoglobin
- HDSS:
-
Health and demographic surveillance system
- ICEMR:
-
International Center of Excellence for Malaria Research
- IPTp:
-
Intermittent preventive treatment during pregnancy
- IRR:
-
Incidence risk ratio
- IRS:
-
Indoor residual spraying
- ITN:
-
Insecticide-treated nets
- MRC:
-
Medical Research Council
- OR:
-
Odds ratio
- PCD:
-
Passive case detection
- RDT:
-
Rapid diagnostic test
- SMC:
-
Seasonal malaria chemoprevention
- WBCs:
-
White blood cells
References
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
WHO. World malaria report 2020: 20 years of global progress and challenges. Geneva: World Health Organization; 2020. https://www.who.int/publications/i/item/9789240015791. Accessed 24 Jan 2023.
Cotter C, Sturrock HJ, Hsiang MS, Liu J, Phillips AA, Hwang J, et al. The changing epidemiology of malaria elimination: new strategies for new challenges. Lancet. 2013;382:900–11.
Keegan LT, Dushoff J. Population-level effects of clinical immunity to malaria. BMC Infect Dis. 2013;13:428.
Bjorkman A, Morris U. Why Asymptomatic Plasmodium falciparum infections are common in low-transmission settings. Trends Parasitol. 2020;36:898–905.
Lindblade KA, Steinhardt L, Samuels A, Kachur SP, Slutsker L. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect Ther. 2013;11:623–39.
Ouedraogo AL, Goncalves BP, Gneme A, Wenger EA, Guelbeogo MW, Ouedraogo A, et al. Dynamics of the human infectious reservoir for malaria determined by mosquito feeding assays and ultrasensitive malaria diagnosis in Burkina Faso. J Infect Dis. 2016;213:90–9.
Bousema T, Okell L, Felger I, Drakeley C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nat Rev Microbiol. 2014;12:833–40.
WHO. World malaria report 2016. Geneva: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/252038/9789241511711-eng.pdf. Accessed 24 Jan 2023.
Lehmann T, Dao A, Yaro AS, Adamou A, Kassogue Y, Diallo M, et al. Aestivation of the African malaria mosquito, Anopheles gambiae in the Sahel. Am J Trop Med Hyg. 2010;83:601–6.
Jawara M, Pinder M, Drakeley CJ, Nwakanma DC, Jallow E, Bogh C, et al. Dry season ecology of Anopheles gambiae complex mosquitoes in The Gambia. Malar J. 2008;7:156.
Babiker HA, Abdel-Muhsin AM, Ranford-Cartwright LC, Satti G, Walliker D. Characteristics of Plasmodium falciparum parasites that survive the lengthy dry season in eastern Sudan where malaria transmission is markedly seasonal. Am J Trop Med Hyg. 1998;59(4):582–90.
Collins KA, Ceesay S, Drammeh S, Jaiteh FK, Guery MA, Lanke K, et al. A cohort study on the duration of Plasmodium falciparum infections during the dry season in The Gambia. J Infect Dis. 2022;226:128–37.
Lin JT, Saunders DL, Meshnick SR. The role of submicroscopic parasitemia in malaria transmission: what is the evidence? Trends Parasitol. 2014;30:183–90.
Le Port A, Cot M, Etard JF, Gaye O, Migot-Nabias F, Garcia A. Relation between Plasmodium falciparum asymptomatic infection and malaria attacks in a cohort of Senegalese children. Malar J. 2008;7:193.
Portugal S, Tran TM, Ongoiba A, Bathily A, Li S, Doumbo S, et al. Treatment of chronic asymptomatic Plasmodium falciparum infection does not increase the risk of clinical malaria upon reinfection. Clin Infect Dis. 2017;64:645–53.
Sonden K, Doumbo S, Hammar U, VafaHomann M, Ongoiba A, Traore B, et al. Asymptomatic multiclonal Plasmodium falciparum infections carried through the dry season predict protection against subsequent clinical malaria. J Infect Dis. 2015;212:608–16.
Doumbo S, Tran TM, Sangala J, Li S, Doumtabe D, Kone Y, et al. Co-infection of long-term carriers of Plasmodium falciparum with Schistosoma haematobium enhances protection from febrile malaria: a prospective cohort study in Mali. PLoS Negl Trop Dis. 2014;8:e3154.
Muller DA, Charlwood JD, Felger I, Ferreira C, do Rosario V, Smith T. Prospective risk of morbidity in relation to multiplicity of infection with Plasmodium falciparum in Sao Tome. Acta Trop. 2001;78:155–62.
Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36.
Smith T, Felger I, Tanner M, Beck HP. Premunition in Plasmodium falciparum infection: insights from the epidemiology of multiple infections. Trans R Soc Trop Med Hyg. 1999;93(Suppl 1):59–64.
Branch OH, Takala S, Kariuki S, Nahlen BL, Kolczak M, Hawley W, et al. Plasmodium falciparum genotypes, low complexity of infection, and resistance to subsequent malaria in participants in the Asembo Bay Cohort Project. Infect Immun. 2001;69:7783–92.
Liljander A, Bejon P, Mwacharo J, Kai O, Ogada E, Peshu N, et al. Clearance of asymptomatic P. falciparum infections interacts with the number of clones to predict the risk of subsequent malaria in Kenyan children. PLoS ONE. 2011;6:e16940.
Ofosu-Okyere A, Mackinnon MJ, Sowa MP, Koram KA, Nkrumah F, Osei YD, et al. Novel Plasmodium falciparum clones and rising clone multiplicities are associated with the increase in malaria morbidity in Ghanaian children during the transition into the high transmission season. Parasitology. 2001;123(Pt 2):113–23.
Ceesay SJ, Casals-Pascual C, Nwakanma DC, Walther M, Gomez-Escobar N, Fulford AJ, et al. Continued decline of malaria in The Gambia with implications for elimination. PLoS ONE. 2010;5:e12242.
Mwesigwa J, Okebe J, Affara M, Di Tanna GL, Nwakanma D, Janha O, et al. On-going malaria transmission in The Gambia despite high coverage of control interventions: a nationwide cross-sectional survey. Malar J. 2015;14:314.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity, Geneva: Vitamin and Mineral Nutrition Information System. Geneva: World Health Organization; 2011.
O’Meara WP, Collins WE, McKenzie FE. Parasite prevalence: a static measure of dynamic infections. Am J Trop Med Hyg. 2007;77:246–9.
Roe MS, O’Flaherty K, Fowkes FJI. Can malaria parasites be spontaneously cleared? Trends Parasitol. 2022;38:356–64.
Andrade CM, Fleckenstein H, Thomson-Luque R, Doumbo S, Lima NF, Anderson C, et al. Increased circulation time of Plasmodium falciparum underlies persistent asymptomatic infection in the dry season. Nat Med. 2020;26:1929–40.
Farnert A, Williams TN, Mwangi TW, Ehlin A, Fegan G, Macharia A, et al. Transmission-dependent tolerance to multiclonal Plasmodium falciparum infection. J Infect Dis. 2009;200:1166–75.
Filipe JA, Riley EM, Drakeley CJ, Sutherland CJ, Ghani AC. Determination of the processes driving the acquisition of immunity to malaria using a mathematical transmission model. PLoS Comput Biol. 2007;3:e255.
Eldh M, Hammar U, Arnot D, Beck HP, Garcia A, Liljander A, et al. Multiplicity of asymptomatic Plasmodium falciparum infections and risk of clinical malaria: a systematic review and pooled analysis of individual participant data. J Infect Dis. 2020;221:775–85.
Bretscher MT, Maire N, Felger I, Owusu-Agyei S, Smith T. Asymptomatic Plasmodium falciparum infections may not be shortened by acquired immunity. Malar J. 2015;14:294.
Felger I, Maire M, Bretscher MT, Falk N, Tiaden A, Sama W, et al. The dynamics of natural Plasmodium falciparum infections. PLoS ONE. 2012;7:e45542.
Stone W, Goncalves BP, Bousema T, Drakeley C. Assessing the infectious reservoir of falciparum malaria: past and future. Trends Parasitol. 2015;31:287–96.
Ahmad A, Soumare HM, Camara MM, Jadama L, Gaye PM, Bittaye H, et al. Infectivity of patent Plasmodium falciparum gametocyte carriers to mosquitoes: establishing capacity to investigate the infectious reservoir of malaria in a low-transmission setting in The Gambia. Trans R Soc Trop Med Hyg. 2021;115:1462–7.
Oduma CO, Ogolla S, Atieli H, Ondigo BN, Lee MC, Githeko AK, et al. Increased investment in gametocytes in asymptomatic Plasmodium falciparum infections in the wet season. BMC Infect Dis. 2021;21:44.
Henning L, Schellenberg D, Smith T, Henning D, Alonso P, Tanner M, et al. A prospective study of Plasmodium falciparum multiplicity of infection and morbidity in Tanzanian children. Trans R Soc Trop Med Hyg. 2004;98:687–94.
Crompton PD, Moebius J, Portugal S, Waisberg M, Hart G, Garver LS, et al. Malaria immunity in man and mosquito: insights into unsolved mysteries of a deadly infectious disease. Annu Rev Immunol. 2014;32:157–87.
Arama C, Skinner J, Doumtabe D, Portugal S, Tran TM, Jain A, et al. Genetic resistance to malaria is associated with greater enhancement of immunoglobulin (Ig)M than IgG responses to a broad array of Plasmodium falciparum antigens. Open Forum Infect Dis. 2015;2:ofv118.
Torcia MG, Santarlasci V, Cosmi L, Clemente A, Maggi L, Mangano VD, et al. Functional deficit of T regulatory cells in Fulani, an ethnic group with low susceptibility to Plasmodium falciparum malaria. Proc Natl Acad Sci U S A. 2008;105:646–51.
Opondo KO, Jawara M, Cham S, Jatta E, Jarju L, Camara M, et al. Status of insecticide resistance in Anopheles gambiae (s.l.) of The Gambia. Parasit Vectors. 2019;12:287.
Bayoh MN, Mathias DK, Odiere MR, Mutuku FM, Kamau L, Gimnig JE, et al. Anopheles gambiae: historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza Province, Kenya. Malar J. 2010;9:62.
Sougoufara S, Harry M, Doucoure S, Sembene PM, Sokhna C. Shift in species composition in the Anopheles gambiae complex after implementation of long-lasting insecticidal nets in Dielmo, Senegal. Med Vet Entomol. 2016;30:365–8.
Acknowledgements
We would like to thank study volunteers and their families. We thank the team of ICEMR investigators from Tulane University, USA: Late Professor Donald J Krogstad (of blessed memory), James C. Welty, Jeffery G. Shaffer, Mary Lukowski and Clarissa Valim. We would also like to thank the following staff from the MRCG at LSHTM: Marie-Rose Thorpe and her team who led the administrative aspect of the ICEMR project, Famalang Camara and his team who led the field work, Mortala Ndow and his team who conducted microscopy readings. We would also want to thank the Gambian National Malaria Control Programme for their collaboration and support during the study.
Funding
This work was funded by Cooperative Agreements from the National Institutes of Allergy and Infectious Diseases (NIAID) for the West African International Center of Excellence for Malaria Research (ICEMR): NIAIDU19AI089696. A.A was supported through the MARCAD DELTAS Africa Initiative grant DEL-15-010. The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust grant 107741/A/15/Z and the UK government.
Author information
Authors and Affiliations
Contributions
DN, UD and JO designed the study, which was conducted by AA, FJ, MJ, MA, SC, AAN and IA. MA supervised microscopy readings. NM, AA, JB and UD analyzed and interpreted the data and the results. AA wrote the original draft manuscript which was reviewed by all authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approvals were obtained from the Gambia Government/MRC Joint Ethics Committee (SCC 1256). Children’s parents or legal representative provided written informed consent prior to screening and study participation.
Consent for publication
Consent for publication of study results and data which do not identify specific individuals was granted by each participant and parents or legal representatives of children when they enrolled for the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
Asexual parasite density (per µ/L) at the start and end of transmission seasons by village setting. Appendix S2. Gametocyte carriers (n) among infected individuals (N) at surveys just before start of season (June). Appendix S3. Coverage at each cross-sectional survey by village setting n/N (%). Appendix S4. Frequency of being an infected compound (at least 1 infected individual in compound) in surveys just before start of transmission (June). Appendix S5. Proportion of individuals that slept under insecticide treated net (ITN) the previous night amongst study clinic attendees 2012 to 2016. Appendix S6. Incidence of clinical malaria (per 1000 population at risk per season) by village setting. Appendix S7. Number of participants by age category sampled at each cross-sectional survey.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahmad, A., Mohammed, N.I., Joof, F. et al. Asymptomatic Plasmodium falciparum carriage and clinical disease: a 5-year community-based longitudinal study in The Gambia. Malar J 22, 82 (2023). https://doi.org/10.1186/s12936-023-04519-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-023-04519-0