Abstract
Purpose
Papillary thyroid carcinoma (PTC), the most common thyroid cancer histotype, has a good prognosis even when spread to the neck lymph node (LN). The prognostic role of LN metastases’ location is still controversial. The aim of the present study was to evaluate the clinical relevance of the number and location of LN metastases at presentation in PTCs.
Methods
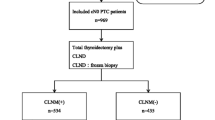
This retrospective study included a consecutive series of 1653 PTC patients followed for a mean period of 5.9 years in a referral thyroid cancer clinic. All patients have undergone thyroidectomy with the dissection of at least six LNs. According to the LN status, patients were subdivided into 569 N0 (34.4%), 644 N1a (39.0%, central compartment) and 440 N1b (26.6%, latero-cervical compartment).
Results
Age at diagnosis was significantly lower in N1b (39.8, IQR 30.7–51.6) and N1a (40.1, IQR 31.3–50.1) than in N0 (44.7, IQR 36.6–55.0 yrs). The male gender was more prevalent in N1b than in N1a and N0 (F/M = 1.9/1, 4.0/1 and 5.5/1, respectively). Persistent/recurrent disease at last control was significantly more frequent in N1b (29.8%) than in N1a (14.3%), and in N1a than in N0 (4.2%) (p < 0.01 for all). Also, distant metastases were significantly (p < 0.001) more frequent in N1b (14.1%) than in N1a (4.3%) and N0 (1.6%). LN metastases’ number (>5) was a significant risk factor for persistent/recurrent disease only for N1a patients.
Conclusions
These data indicate that persistent/recurrent disease and distant metastases are significantly more frequent in patients with latero-cervical LN (N1b) metastases and that the LN location should be used for a better postsurgical risk stratification.

Similar content being viewed by others
References
Shin HR, Masuyer E, Ferlay J, Curado MP, Contributors Asian, Asian Contributors to CI (2010) Cancer in Asia—Incidence rates based on data in cancer incidence in five continents IX (1998–2002). Asian Pac J Cancer Prev APJCP 11(Suppl 2):11–16
Davies L, Welch HG (2014) Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surgery 140(4):317–322. doi:10.1001/jamaoto.2014.1
Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH (2003) Papillary microcarcinoma of the thyroid-Prognostic significance of lymph node metastasis and multifocality. Cancer 98(1):31–40. doi:10.1002/cncr.11442
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 5(1):43–63
Hay ID, Grant CS, van Heerden JA, Goellner JR, Ebersold JR, Bergstralh EJ (1992) Papillary thyroid microcarcinoma: a study of 535 cases observed in a 50-year period. Surgery 112(6):1139–1146 (discussion 1146-1137)
Stulak JM, Grant CS, Farley DR, Thompson GB, van Heerden JA, Hay ID, Reading CC, Charboneau JW (2006) Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141(5):489–494. doi:10.1001/archsurg.141.5.489 (discussion 494-486)
O’Connell K, Yen TW, Quiroz F, Evans DB, Wang TS (2013) The utility of routine preoperative cervical ultrasonography in patients undergoing thyroidectomy for differentiated thyroid cancer. Surgery 154(4):697–701. doi:10.1016/j.surg.2013.06.040 (discussion 701-693)
Lesnik D, Cunnane ME, Zurakowski D, Acar GO, Ecevit C, Mace A, Kamani D, Randolph GW (2014) Papillary thyroid carcinoma nodal surgery directed by a preoperative radiographic map utilizing CT scan and ultrasound in all primary and reoperative patients. Head Neck 36(2):191–202. doi:10.1002/hed.23277
Yeh MW, Bauer AJ, Bernet VA, Ferris RL, Loevner LA, Mandel SJ, Orloff LA, Randolph GW, Steward DL, American Thyroid Association Surgical Affairs Committee Writing Task F (2015) American Thyroid Association statement on preoperative imaging for thyroid cancer surgery. Thyroid Off J Am Thyroid Assoc 25(1):3–14. doi:10.1089/thy.2014.0096
Sugitani I, Fujimoto Y, Yamada K, Yamamoto N (2008) Prospective outcomes of selective lymph node dissection for papillary thyroid carcinoma based on preoperative ultrasonography. World J Surg 32(11):2494–2502. doi:10.1007/s00268-008-9711-9
Scherl S, Mehra S, Clain J, Dos Reis LL, Persky M, Turk A, Wenig B, Husaini H, Urken ML (2014) The effect of surgeon experience on the detection of metastatic lymph nodes in the central compartment and the pathologic features of clinically unapparent metastatic lymph nodes: what are we missing when we don’t perform a prophylactic dissection of central compartment lymph nodes in papillary thyroid cancer? Thyroid Off J Am Thyroid Assoc 24(8):1282–1288. doi:10.1089/thy.2013.0600
Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R (1998) The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg 228(3):320–330
Leboulleux S, Rubino C, Baudin E, Caillou B, Hartl DM, Bidart JM, Travagli JP, Schlumberger M (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 90(10):5723–5729. doi:10.1210/jc.2005-0285
Adam MA, Pura J, Goffredo P, Dinan MA, Reed SD, Scheri RP, Hyslop T, Roman SA, Sosa JA (2015) Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol 33(21):2370–2375. doi:10.1200/JCO.2014.59.8391
Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, Tufano RP, Tuttle RM, American Thyroid Association Surgical Affairs Committee’s Taskforce on Thyroid Cancer Nodal S (2012) The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid Off J Am Thyroid Assoc 22(11):1144–1152. doi:10.1089/thy.2012.0043
Lee J, Song Y, Soh EY (2014) Prognostic significance of the number of metastatic lymph nodes to stratify the risk of recurrence. World J Surg 38(4):858–862. doi:10.1007/s00268-013-2345-6
Alpert EH, Wenig BM, Dewey EH, Su HK, Dos Reis L, Urken ML (2015) Size distribution of metastatic lymph nodes with extranodal extension in patients with papillary thyroid cancer: a pilot study. Thyroid Off J Am Thyroid Assoc 25(2):238–241. doi:10.1089/thy.2014.0392
Clain JB, Scherl S, Dos Reis L, Turk A, Wenig BM, Mehra S, Karle WE, Urken ML (2014) Extrathyroidal extension predicts extranodal extension in patients with positive lymph nodes: an important association that may affect clinical management. Thyroid Off J Am Thyroid Assoc 24(6):951–957. doi:10.1089/thy.2013.0557
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A (2006) Prognostic significance of extrathyroid extension of papillary thyroid carcinoma: massive but not minimal extension affects the relapse-free survival. World J Surg 30(5):780–786. doi:10.1007/s00268-005-0270-z
Fukushima M, Ito Y, Hirokawa M, Miya A, Shimizu K, Miyauchi A (2010) Prognostic impact of extrathyroid extension and clinical lymph node metastasis in papillary thyroid carcinoma depend on carcinoma size. World J Surg 34(12):3007–3014. doi:10.1007/s00268-010-0776-x
Radowsky JS, Howard RS, Burch HB, Stojadinovic A (2014) Impact of degree of extrathyroidal extension of disease on papillary thyroid cancer outcome. Thyroid Off J Am Thyroid Assoc 24(2):241–244. doi:10.1089/thy.2012.0567
Nixon IJ, Ganly I, Patel S, Palmer FL, Whitcher MM, Tuttle RM, Shaha AR, Shah JP (2011) The impact of microscopic extrathyroid extension on outcome in patients with clinical T1 and T2 well-differentiated thyroid cancer. Surgery 150(6):1242–1249. doi:10.1016/j.surg.2011.09.007
Nikiforov YE, Ohori NP, Hodak SP, Carty SE, LeBeau SO, Ferris RL, Yip L, Seethala RR, Tublin ME, Stang MT, Coyne C, Johnson JT, Stewart AF, Nikiforova MN (2011) Impact of mutational testing on the diagnosis and management of patients with cytologically indeterminate thyroid nodules: a prospective analysis of 1056 FNA samples. J Clin Endocrinol Metab 96(11):3390–3397. doi:10.1210/jc.2011-1469
Alexander EK, Kennedy GC, Baloch ZW, Cibas ES, Chudova D, Diggans J, Friedman L, Kloos RT, LiVolsi VA, Mandel SJ, Raab SS, Rosai J, Steward DL, Walsh PS, Wilde JI, Zeiger MA, Lanman RB, Haugen BR (2012) Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med 367(8):705–715. doi:10.1056/NEJMoa1203208
Bartolazzi A, Orlandi F, Saggiorato E, Volante M, Arecco F, Rossetto R, Palestini N, Ghigo E, Papotti M, Bussolati G, Martegani MP, Pantellini F, Carpi A, Giovagnoli MR, Monti S, Toscano V, Sciacchitano S, Pennelli GM, Mian C, Pelizzo MR, Rugge M, Troncone G, Palombini L, Chiappetta G, Botti G, Vecchione A, Bellocco R, Italian Thyroid Cancer Study G (2008) Galectin-3-expression analysis in the surgical selection of follicular thyroid nodules with indeterminate fine-needle aspiration cytology: a prospective multicentre study. Lancet Oncology 9(6):543–549. doi:10.1016/S1470-2045(08)70132-3
Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A (2004) A novel classification system for patients with PTC: addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery 135(2):139–148. doi:10.1016/S0039
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM, American Thyroid Association Guidelines Taskforce on Thyroid N, Differentiated Thyroid C (2009) Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc 19(11):1167–1214. doi:10.1089/thy.2009.0110
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc 26(1):1–133. doi:10.1089/thy.2015.0020
Sargent D (2006) General and statistical hierarchy of appropriate biologic endpoints. Oncology (Williston Park) 20(6 Suppl 5):5–9
Nardi F, Basolo F, Crescenzi A, Fadda G, Frasoldati A, Orlandi F, Palombini L, Papini E, Zini M, Pontecorvi A, Vitti P (2014) Italian consensus for the classification and reporting of thyroid cytology. J Endocrinol Investig 37(6):593–599. doi:10.1007/s40618-014-0062-0
Castagna MG, Cantara S, Pacini F (2016) Reappraisal of the indication for radioiodine thyroid ablation in differentiated thyroid cancer patients. J Endocrinol Investig 39(10):1087–1094. doi:10.1007/s40618-016-0503-z
Pacini F, Brianzoni E, Durante C, Elisei R, Ferdeghini M, Fugazzola L, Mariotti S, Pellegriti G (2016) Recommendations for post-surgical thyroid ablation in differentiated thyroid cancer: a 2015 position statement of the Italian Society of Endocrinology. J Endocrinol Investig 39(3):341–347. doi:10.1007/s40618-015-0375-7
Lang BH, Ng SH, Lau LL, Cowling BJ, Wong KP, Wan KY (2013) A systematic review and meta-analysis of prophylactic central neck dissection on short-term locoregional recurrence in papillary thyroid carcinoma after total thyroidectomy. Thyroid Off J Am Thyroid Assoc 23(9):1087–1098. doi:10.1089/thy.2012.0608
Wang TS, Cheung K, Farrokhyar F, Roman SA, Sosa JA (2013) A meta-analysis of the effect of prophylactic central compartment neck dissection on locoregional recurrence rates in patients with papillary thyroid cancer. Ann Surg Oncol 20(11):3477–3483. doi:10.1245/s10434-013-3125-0
Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JW, Wiersinga W, European Thyroid Cancer T (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol Eur Fed Endocr Soc 154(6):787–803. doi:10.1530/eje.1.02158
Chereau N, Buffet C, Tresallet C, Tissier F, Leenhardt L, Menegaux F (2016) Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: predictive factors and operative management. Surgery 159(3):755–762. doi:10.1016/j.surg.2015.08.033
Choi SY, Cho JK, Moon JH, Son YI (2016) metastatic lymph node ratio of central neck compartment has predictive values for locoregional recurrence in papillary thyroid microcarcinoma. Clin Exp Otorhinol 9(1):75–79. doi:10.21053/ceo.2016.9.1.75
Urken ML, Mechanick JI, Sarlin J, Scherl S, Wenig BM (2014) Pathologic reporting of lymph node metastases in differentiated thyroid cancer: a call to action for the College of American Pathologists. Endocr Pathol 25(3):214–218. doi:10.1007/s12022-013-9282-7
Wang LY, Palmer FL, Nixon IJ, Tuttle RM, Shah JP, Patel SG, Shaha AR, Ganly I (2015) Lateral neck lymph node characteristics prognostic of outcome in patients with clinically evident N1b Papillary thyroid cancer. Ann Surg Oncol 22(11):3530–3536. doi:10.1245/s10434-015-4398-2
Ito Y, Miyauchi A (2009) Prognostic factors and therapeutic strategies for differentiated carcinomas of the thyroid. Endocr J 56(2):177–192
Moreno MA, Agarwal G, de Luna R, Siegel ER, Sherman SI, Edeiken-Monroe BS, Clayman GL (2011) Preoperative lateral neck ultrasonography as a long-term outcome predictor in papillary thyroid cancer. Arch Otolaryngol Head Neck Surg 137(2):157–162. doi:10.1001/archoto.2010.254
Ito Y, Uruno T, Nakano K, Takamura Y, Miya A, Kobayashi K, Yokozawa T, Matsuzuka F, Kuma S, Kuma K, Miyauchi A (2003) An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid Off J Am Thyroid Assoc 13(4):381–387. doi:10.1089/105072503321669875
Lee SG, Ho J, Choi JB, Kim TH, Kim MJ, Ban EJ, Lee CR, Kang SW, Jeong JJ, Nam KH, Jung SG, Jo YS, Lee J, Chung WY (2016) Optimal cut-off values of lymph node ratio predicting recurrence in papillary thyroid cancer. Medicine 95(5):e2692. doi:10.1097/MD.0000000000002692
Acknowledgements
This work was supported in part by a Grant from the Associazione Italiana per la Ricerca sul Cancro (AIRC, Milan, Italy) to R.V.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have nothing to declare.
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of institutional research committee and with the Helsinki declaration as revised in 2013.
Informed consent
Informed consent of the present retrospective study was waived.
Rights and permissions
About this article
Cite this article
Sapuppo, G., Palermo, F., Russo, M. et al. Latero-cervical lymph node metastases (N1b) represent an additional risk factor for papillary thyroid cancer outcome. J Endocrinol Invest 40, 1355–1363 (2017). https://doi.org/10.1007/s40618-017-0714-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0714-y