Abstract
Introduction
Published data on hypertension incidence and management in Anderson–Fabry disease are scant and the contribution of elevated blood pressure to organ damage is not well recognized.
Aim
Therefore, we have assessed blood pressure values and their possible correlations with clinical findings in a well described cohort of Fabry patients.
Methods
Between January 2015 and May 2019, all adult Fabry patients (n = 24 females, n = 8 males) referred to our institute were prospectively enrolled. During the first examination patient’s genotype and clinical characteristics were recorded. Blood pressure data were obtained by standard observed office measurements followed, within 6 months, by ambulatory blood pressure monitoring and home self-recordings. Organ involvement, including kidneys, heart and brain, was monitored over time. Consequently, patients were defined as clinically stable or progressive through the Fabry Stabilization Index.
Results
The standard office measurements have diagnosed hypertension in three (9.37%) patients, but the ambulatory monitoring showed elevated blood pressure in six (18.75%) patients, revealing three cases of masked hypertension. All the hypertensive patients were females and, compared with normotensive subjects, they presented a lower glomerular filtration rate (p < 0.05) and a more advanced cardiac hypertrophy (p < 0.05). Four (66.7%) of them were diagnosed with a progressive form of the disease through the Fabry Stabilization Index while the majority of the normotensive group (84.6%, n = 19) was stable over time. No correlation was found between the prevalence of hypertension and the type of mutations causing Fabry disease.
Conclusion
Hypertension can be found in a restricted portion of clinically stable Fabry patients. In contrast, patients presenting with a progressive organ involvement, particularly renal impairment, have a major risk of developing uncontrolled blood pressure, and should be followed carefully. Moreover, the ambulatory blood pressure monitoring proved to be useful to reveal masked hypertension, which can contribute to the progressive worsening of the organ damage. Therefore, a proper diagnosis and therapy of hypertension may improve the outcome of Fabry patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Anderson–Fabry disease (AFD) is a rare X-linked sphingolipid storage disorder caused by a mutation in the GLA gene leading to a deficient activity of the lysosomal enzyme α-galactosidase A (α-Gal A). The reduced or absent activity of the enzyme results in a progressive lysosomal accumulation of globotriaosylceramide (Gb3) and its derivates, including globotriaosylsphingosine (lyso-Gb3), within different body cells [1].
The phenotypic spectrum of the disease comprises a “classic” form characterized by a total, or almost total, absence of α-Gal A activity and an early onset of the symptoms, generally during childhood or adolescence, with neuropathic pain, skin lesions (angiokeratomas), gastrointestinal symptoms and corneal opacities (cornea verticillata) [2]. Advancing with age, the progressive glycosphingolipid accumulation, particularly in vascular endothelial cells, cardiomyocytes and renal podocytes, leads to cerebrovascular disease, cardiomyopathy and renal failure [3] resulting in severe morbidity and premature death [4].
In contrast, two other categories of the disease are increasingly diagnosed: the “late-onset” and the “genetic variant of unknown significance” (GVUS) [5]. The former generally leads to a milder disease in adulthood, especially in females, and often involves a single organ system (usually cardiac or renal), while the latter is associated with unclear and variable pathological consequences or no clinical disease at all [6].
Data on blood pressure (BP) monitoring in AFD patients are scant, however, those available have revealed a significant prevalence of hypertension, especially in cases with moderate to severe kidney impairment [7,8,9,10,11] and it becomes more prevalent with the progression of the renal disease [8].
Kleinert et al. examined uncontrolled hypertension, defined as systolic BP (SBP) ≥ 130 mmHg and/or diastolic BP (DBP) ≥ 80 mmHg, among 391 patients with AFD participating in the Fabry Outcome Survey (FOS). Uncontrolled hypertension was diagnosed in 52.4% of the participants (57% males and 47% females) progressively increasing with the decline of glomerular filtration rate (GFR) estimated using the short Modification of Diet in Renal Disease (MDRD) formula [7].
On the contrary, analysing 105 male AFD patients, Branton et al. showed that hypertension (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg) was diagnosed in only one-third of the patients (30%) and, in most cases, was not present until the onset, or long after the onset, of renal impairment or end-stage renal disease (ESRD) [12].
Given the wide and complex spectrum of AFD and the potential negative impact of hypertension on target organ damage (kidney, heart and nervous system), an appropriate algorithm for the diagnosis and therapy of elevated blood pressure may improve morbidity and mortality of AFD patients [13].
Our aim was therefore to assess BP levels and analyse its clinical implications, compare routine BP measurement techniques and describe risk factors for hypertension. Additionally, we analysed possible correlations between high BP and patient’s genotype.
2 Methods
Patients aged 18 years or older with a prior confirmed genetic diagnosis of AFD were eligible for inclusion. Between January 2015 and May 2019, thirty-two patients referred to the Fabry Disease Unit, Nephrology Division of San Gerardo Hospital (Monza, Italy) were prospectively enrolled in the study. They were twenty-four (75%) females and eight (25%) males; all of them gave informed consent.
The included patients (n = 32) accounted for 80% of the total eligible Fabry patient cohort (n = 40) at our institution in that time-period. Accordingly, the following patients (20%, n = 8) were excluded from the study: four patients refused or failed to perform the 24-h ambulatory blood pressure monitoring (ABPM) and four subjects reported insufficient clinical or echocardiographic information.
2.1 Blood Pressure Measurements
BP values were obtained by ABPM (oscillometric method), office measurements and home recordings. First, during our examination, we measured patient’s sitting BP following 5 min rest and standing BP within 3 min of assuming the upright position. Our observed office measurements were paired, within 6 months, to ABPM and home blood pressure monitoring results. Patients were invited to monitor and record their BP at home for seven consecutive days. On each day they took three measurements in the morning and three in the evening, then the average values were logged. Therefore, hypertension was defined according to 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) Guidelines for the management of arterial hypertension [14] (Supplemental Digital Content 1).
2.2 Characterization of Patients
During the first evaluation, we collected patient’s demographical characteristics and assessed the occurrence of any risk factors related to the development of hypertension.
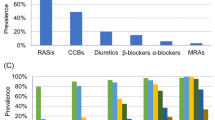
Information on medications such as enzyme replacement therapy (ERT) or oral chaperone therapy and antihypertensive drugs (calcium channel blockers, ACE inhibitors (ACEi), angiotensin II receptor antagonists (ARBs), diuretics and beta-blockers) were also recorded.
Patient genotype and phenotype were characterized. In particular, we analysed the different mutations carried by each patient (classic, late-onset) and investigated whether there could be a statistical correlation between them and the occurrence of high BP. Fabry organ damage was analysed and in particular we focused on renal and cardiac alterations, which are related with the development of hypertension [7,8,9,10,11].
The glomerular filtration rate (GFR) was measured along with the albumin-to-creatinine ratio (ACR) and the proteinuria levels on a 24-hours urine collection sample. According to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines, chronic kidney disease was classified in different levels ranging from G1 to G5 on the GFR scale and A1 to A3 on the ACR range [15] (Supplemental Digital Content 2). Serum electrolyte test and automatic urinary sediment analyses were also performed by our routine biochemistry laboratory.
2.2.1 Echocardiographic Examination
During the first examination of our study, parasternal and apical 2-dimensional echocardiograms (2D) were acquired according to the American Society of Echocardiography/European Association of Echocardiography (ASE/EAE) recommendations [16]. All echocardiograms were performed and analysed by the same experienced cardiologist. The inter-ventricular septum thickness at end diastole (IVSd), the posterior wall thickness at end diastole (PWd) and the diameter of the left ventricle at end diastole (LVDd) were measured at end-diastole. Left ventricular mass index (LVMi) and relative wall thickness (RWT) were calculated using the adequate equations [17, 18]. The reference ranges for these values were: RWT ≤ 0.42 in males and females, LVMi < 115 g/m2 in males and < 95 g/m2 in females. The geometric changes of the left ventricle were classified, using the LVMi and RWT values, in concentric hypertrophy (elevated RWT with increased LVMi), concentric remodelling (elevated RWT with normal LVMi), eccentric hypertrophy (normal RWT with increased LVMi) and normal geometry (normal RWT with normal LVMi). Data on the ejection fraction (EF), left atrial volume index (LAVi), tricuspid annular plane systolic excursion (TAPSE), E/e′ and E/A ratio were reported.
2.2.2 Fabry Stabilization Index Assessment
The severity and the stability of the organ involvement were assessed through the Fabry Stabilization Index (FASTEX) [19]. We calculated the “raw score” based on seven clinical parameters: pain, cerebrovascular events, proteinuria, glomerular filtration rate, echocardiography parameters, electrocardiographic parameters and New York Heart Association (NYHA) class. Two “raw scores” were compared in two consecutive visits one year apart, obtaining the FASTEX index: a percentage threshold value that indicates if the patient has worsened between one visit and another. When FASTEX is equal to or greater than 20%, the patient is defined not stable, if less than 20% the patient is in stable conditions [19]. The score was obtained using the online FASTEX index tool [20].
2.3 Statistical Analysis
Data are given as means ± standard deviation (SD). Statistical analysis was performed using Microsoft Excel and SPSS version 25.0. Mean values were compared by Student’s t-test for independent samples and categorical data were analysed by the Fisher’s exact test when appropriate.
3 Results
3.1 Blood Pressure Measurements
Out of the whole population (n = 32), the standard office and home measurements showed high BP in three (9.37%) patients. The ABPM, confirming the previous results, allowed us to diagnose hypertension in other three (9.37%) cases, for a total of six (18.75%) hypertensive patients. The rest of the population (81.25%, n = 26) was normotensive, but included four patients with a prior diagnosis of hypertension and currently under an adequate anti-hypertensive therapy.
The ABPM of the hypertensive patients showed a mean SBP of 138.17 ± 4.88 mmHg and a mean DBP of 81.17 ± 3.66 mmHg, half (50%, n = 3) of them presented a non-dipper pattern. One half (50%, n = 3) reported normal office BP measurements (SBP 130 ± 2.6 mmHg, DBP 82.33 ± 2.5 mmHg) and normal home values (SBP 121 ± 8.9 mmHg, DBP 82.33 ± 2.1 mmHg). Three patients (50%) presented an elevation of both home and office BP levels. In detail, the results of the home monitoring revealed a mean SBP of 133.33 ± 14.77 mmHg and a mean DBP of 89.17 ± 7.63 mmHg, while the office measurements presented a mean SBP of 144.17 ± 16.07 mmHg and a DBP of 90.83 ± 9.91 mmHg, without differences between sitting and standing (Table 1).
The true normotensive patients (68.75%, n = 22) at the ABPM revealed a mean SBP of 111.64 ± 10.61 mmHg and a mean DBP of 65.68 ± 6.30 mmHg. The office monitoring showed a SBP of 119.09 ± 11.48 mmHg and a DBP of 73.64 ± 8.47 mmHg while the home measurements a SBP of 114.32 ± 10.20 mmHg and a DBP of 65.91 ± 6.40 mmHg (Table 1). Only one (3.8%) patient presented elevated BP values at the office monitoring, probably due to the “white coat syndrome”.
The four patients with a previously known diagnosis of hypertension presented a pressure profile (ABPM, home and outpatient monitoring) well controlled by the current anti-hypertensive therapy. At the ABPM showed a normal mean SBP of 116.75 ± 1.26 mmHg and a mean DBP of 72.5 ± 3.70 mmHg along with normal office and home BP monitoring (Table 1).
3.2 Characterization of the Patients
All patients (n = 32) were Caucasian with an average age of 50.3 ± 12.4 (22 ÷ 69) years.
They had mostly a sedentary lifestyle (56.25%, n = 18) and less than a half of them was affected by dyslipidaemia (43.75%, n = 14). Obesity was a rare condition (9.37%, n = 3) and the average body mass index was within normal ranges (BMI=23.3 ± 4.1). Glucose intolerance and diabetes type 2 were uncommon (3.12%, n = 1) and only few of them were smokers (21.87%, n = 7) or alcohol consumers (9.37%, n = 3) (Table 2).
The six hypertensive patients were all females with an average age of 58 ± 10.9 (43÷69) years old, but they were not significantly older (p > 0.05) compared with the normotensive patients which had an average age of 48.4 ± 12.4 (22÷69) years.
They had mostly a sedentary life-style (83.3%, n = 5), half of them (50%, n = 3) had a known diagnosis of dyslipidaemia and one was considered obese with a BMI > 30. Smoking habit and alcohol consumption were a rare condition (16.6%, n = 1).
Similarly, almost half of the normotensive patients had a sedentary life-style and a known diagnosis of dyslipidaemia. Two were considered obese. Smoking habit and alcohol consumption were a rare condition. The same applies for patients with treated hypertension who were also predominantly sedentary and with a low prevalence of smokers and alcohol users (Table 2).
This group of patients were under anti-hypertensive drugs such as calcium channel blockers (25%, n = 1) or ACEi (50%, n = 2) in combination with beta-blockers (50%, n = 2) or diuretics (25%, n = 1). Equally, seven (31.81%) of the normotensive patients were taking anti-proteinuric drugs (ACEi and ARBs), but all of them had normal BP levels (office and home monitoring) even before starting the therapy. The remaining (65.6%, n = 21) did not have a known diagnosis of hypertension and were not taking any anti-hypertensive drug (Table 2).
The 59.4% (n = 19, 12 females and 7 males) of the total population was under specific treatment for AFD, two (10.52%) were taking migalastat and the majority (89.48%, n = 17) were on enzyme replacement therapy (ERT): 41.2% (n = 7) on agalsidase-alpha and 58.8% (n = 10) on agalsidase-beta (Table 2).
The remaining patients (40.6%, n = 13) were still under assessment, whereas three (23.07%) of them had already refused the therapy.
The phenotypic expression was varied, with more than a half of the patients presenting with multi-organ involvement. Signs and symptoms mainly involved the nervous (neuropathic pain and dyshidrosis), cardiac (echocardiographic alterations) and renal (proteinuria and renal failure) systems (Table 3).
Chronic kidney disease ranged mainly from G1/A1 to G2/A1 (81.25%, n = 26) while few patients (18.75%, n = 6) presented a more advanced renal failure with chronic kidney disease (CKD) stages from G3a to G5 and/or albuminuria stages from A2 to A3 (Table 2).
Three untreated hypertensive patients (50%) presented with renal impairment, two with CKD stage G3a/A2 and the patient with BMI > 30 showed hyperfiltration (eGFR > 150 ml/min) (Table 3). They presented a lower (p < 0.05) eGFR compared with the normotensive patients, whilst other renal indexes were not significantly different between the groups (Table 4). No electrolytic imbalance or urinary sediment alterations were detected. All the hypertensive patients had cardiological involvement and peripheral neurological manifestations with acroparesthesias and/or hypohidrosis. Three patients (50%) presented with gastrointestinal symptoms, two out of three experiencing recurrent episodes of abdominal pain and one complaining of frequent nausea and diarreha. No one had pulmonary or cutaneous involvement. Nearly all patients with treated hypertension had cardiological (75%, n = 3) involvement as well as normotensives (86.4%, n = 19) (Table 3).
All patients were carriers of heterogeneous GLA gene mutations. The majority (71.87%, n = 23) expressed a classic or likely-classic [21] mutation. Seven (21,87%) had a late-onset one, with the most common being the p.Asn215Ser (85.71%, n = 6) which has been reported to be associated with a late-onset cardiac variant [22]. Two (6.25%) patients had a mutation not previously described in literature. In the normotensive group sixteen (72.7%) patients had a classic or “likely classic” mutation, five a late-onset and one a not-previously-described one (Table 5). The patients with treated hypertension mostly expressed a classical phenotype (75%, n = 3) (Table 5) with mainly cardiac involvement (75%, n = 3) (Table 3).
Finally, in the hypertensive group, four patients (66.7%) were carrying a classic or likely-classic mutation, one a late-onset and another a not previously described (ND) mutation (Table 5). The correlation test between the prevalence hypertension and the type of mutations, classical or late-onset, was not significant (p > 0.05).
3.2.1 Echocardiographic Examination
The echocardiogram examination showed an all-over high prevalence of cardiac hypertrophy; thirteen (40.6%) patients presented a concentric hypertrophy, seven (21.9%) a concentric remodelling and twelve (37.5%) had normal parameters. All the untreated hypertensive patients (18.75%, n = 6) were diagnosed with concentric hypertrophy with a significantly higher LVPWD (p < 0.05) and LVMi (p < 0.05) compared to the normotensive patients. All the other echocardiographic parameters were not significantly different between hypertensive and normotensive patients.
All the treated hypertensive patients (12.5%, n = 4) presented a concentric hypertrophy, but no statistically significant differences were found between this group and the normotensive one (Table 6).
3.2.2 FASTEX Assessment
In the overall study population (n = 32), eight (25%) patients presented a progressive form of AFD accordingly to the FASTEX score. Four out of the six (66.7%) hypertensive subjects were classified as progressive, while a great portion (86.4%, n = 19) of the normotensive group was not. The majority (75%, n = 3) of well treated hypertensive patients also showed a stable FASTEX score (Figure 1).
4 Discussion
In this study, the majority of AFD patients (68.75%, n = 22) were normotensive without specific blood pressure control therapy. Four (12.5%) patients previously diagnosed with hypertension and currently under anti-hypertensive treatment showed a well-controlled blood pressure, while six (18.75%) were diagnosed with uncontrolled hypertension for the first time, due to the ABPM measurements. Half of them presented a non-dipping blood pressure pattern, which is shown to be associated with additional cardiovascular alterations and organ damage [24]. Of note, half of these patients had normal blood pressure recordings in office and home measurements; masked hypertension was diagnosed with 24-h blood pressure measurements highlighting the need of standardized long-term recordings, especially in patients with concomitant early signs of cardiomyopathy and/or nephropathy.
Our findings in the AFD population are in line with a recent presentation that shows that masked hypertension may have an average prevalence of about 40% in CKD-patients [25].
Apart from dyslipidaemia and sedentary lifestyle, the overall population revealed a low prevalence of well-known risk factors for the development of hypertension such obesity, glucose intolerance and diabetes, smoke habit and alcohol consumption.
The hypertensive group showed a higher prevalence of kidney involvement with the development of proteinuria and renal failure, supporting previous reports [7,8,9,10,11]. Almost all of them presented electrocardiographic and echocardiographic alterations and the echocardiographic analysis highlighted that patients with uncontrolled hypertension showed a worse cardiac hypertrophy as compared to the well treated-hypertensive patients.
The majority of the hypertensive patients presented a progressive disease through the FASTEX, indexes of progressive renal damage are included in determining the score and renal failure and its progression can be considered a crucial factor in the development of hypertension Moreover, untreated high blood pressure values represent an established risk factor for adverse cardiovascular and kidney outcomes [25, 26].
In addition, hypertensive AFD patients showed a higher prevalence of classical mutations, related to a more severe phenotype compared with the late-onset ones, mainly involving one organ system such as the neuro-vegetative, cardiological or renal one [27].
In our study, the prevalence of hypertensive patients was lower as compared to several previous published papers [7,8,9,10]. For instance, our results are in contrast to the report by Kleinert et al. [7] which showed a high overall rate of uncontrolled hypertension (57% in male patients) in a population of 391 patients affected by AFD. We described a lower prevalence of hypertension despite the average age of our patients being higher. Furthermore, the majority of our patients were female, and none of our patients had severe kidney failure, ESRD, needed dialysis or had received a kidney transplantation. In addition, the criteria for the diagnosis of hypertension differs slightly between the two studies. It is significant to point out that we analysed a smaller sample size, but our blood pressure monitoring was strictly structured.
Notably, our hypertensive patients were identified by automated and home blood pressure analyses, highlighting the need of well standardized blood pressure measuring routines in the follow-up of Fabry patients as half of them presented with normal office blood pressure. An important observation in our study is the association between non-controlled hypertension and clinically progressive disease, not seen in those patients where blood pressure was well controlled by antihypertensive agents at the time of inclusion. Of note, our observation also highlights the necessity of diagnosing the often-overlooked masked hypertension in AFD patients with early progressive cardiac or renal disease.
Moreover, a study on 10,051 individuals (53.2% female, age 56.2 ± 16.8 years) revealed that the prevalence of hypertension in Italy varies from 55 to 59% [28]. Taking into account the limitations of a comparison between these studies, our data indicate that hypertension is not a frequent finding in stable and well-monitored AFD patients, who are likely to have a lower prevalence compared to the general population with the same age range. This is consistent with the general concept that Fabry disease often is accompanied by lower blood pressure levels, which in fact may limit the anti-proteinuric use of ACEi/RAS-blockade in many patients [29]. Our findings may help raise the awareness of masked hypertension in Fabry disease patients. The purpose of a close blood pressure control in AFD population is important to reduce cardiovascular events and progressive deterioration of renal function. We recommend the inclusion of ABPM for a reliable monitoring of BP in routine follow-up of AFD patients. Other studies in CKD patients confirm that the routine office BP measurements provide imprecise reflection of the actual BP load [25, 30] as recommended by the ESC-ESH Guidelines 2018 [31].
The mechanisms connecting Fabry disease to the development of hypertension have not been fully studied yet. Hypertension might be a consequence of an AFD associated vascular disease.
It is not known whether the vascular disease originates from the deposition of glycosphingolipids in endothelial cells or in smooth muscle cells in the arterial media layer [32, 33]. Growing evidence indicates that the deposition of Gb3 in the endothelium activates oxidative enzymes such as nicotinamide adenine dinucleotide phosphate (NADPH) oxidases leading to the production of reactive oxygen species (ROS) [34]. Moreover, storage of glycosphingolipids in smooth muscle cells may promote cell proliferation with fibrotic remodelling of the arterial wall leading to arterial wall stiffness resulting in shear stress that may increase the expression of angiotensin 1 and 2 receptors in endothelial cells, increasing ROS, NF-kB, beta-integrin and cyclooxygenase 1 and 2 activity and decreasing nitric oxide synthesis [35]. These mechanisms may lead to oxidative stress and inflammatory damage which promotes endothelial and vascular dysfunction leading to the development of hypertension [36].
Patients affected by Fabry disease may also develop hypertension due to a direct renal damage [8] caused by the accumulation of glycolipids within the tubular epithelial cells and the podocytes, leading to tubular atrophy, interstitial fibrosis and segmental and global glomerulosclerosis [37].
It has long been accepted the concept that renal impairment and hypertension are closely associated [38]. Sustained and untreated high blood pressure values hasten the progression of kidney disease and, in turn, renal damage is clearly related to the development of hypertension [39].
Another theory speculates that hypertension may be a process unrelated to Fabry disease, such as in the case of essential hypertension [12]. Additionally, kidney biopsy reports have shown concomitant renal diseases causing hypertension that may co-exist with Fabry disease (e.g., focal and segmental glomerular sclerosis, membranous or IgA nephropathy) [40,41,42,43].
However, we can speculate that glycolipids accumulation may also affect the autonomic nervous system causing an impairment of the arterial baroreflex function [44], leading to an altered blood pressure regulation, with possible orthostatic hypotension and predisposition to syncope [9] even if we did not diagnose any orthostatic hypotension in our patients.
The limitations of our study are the small sample size of the population analysed and the higher prevalence of women compared to men. It is important to underline also the lack in the analysis of the patients eating habits, the sodium intake and natriuresis. Enlisting a control group of non-AFD patients would have helped to better develop the analysis. Data on prolonged follow-up are not available, therefore the prognostic impact of hypertension and its consequences cannot be clearly reported.
The strength of the study are the accurate characterization of the patients and the meticulous BP monitoring according to current guidelines.
5 Conclusions
The results of our study underline that hypertension can be found in a restricted portion of stable and well-monitored AFD patients with minimal signs of organ complications, becoming more prevalent in clinically progressive cases. The ABPM proved to be useful to reveal the cases of masked hypertension which, if not properly diagnosed, can contribute to the progressive worsening of the organ damage. We recommend a standardised ambulatory long-term blood pressure monitoring program and timely antihypertensive intervention to improve the outcome of AFD patients.
References
Aerts JM, et al. Elevated globotriaosylsphingosine is a hallmark of Fabry disease. Proc Natl Acad Sci USA. 2008;105:2812–7.
Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5:30.
Nowak A, Mechtler T, Kasper DC, Desnick RJ. Correlation of Lyso-Gb3 levels in dried blood spots and sera from patients with classic and Later-Onset Fabry disease. Mol Genet Metab. 2017;121:320–4.
Hoffmann B. Fabry disease: recent advances in pathology, diagnosis, treatment and monitoring. Orphanet J Rare Dis. 2009;4:21.
van der Tol L, et al. A systematic review on screening for Fabry disease: prevalence of individuals with genetic variants of unknown significance. J Med Genet. 2014;51:1–9.
Svarstad E, Marti HP. The changing landscape of Fabry disease. Clin J Am Soc Nephrol. 2020;15(4):569–76.
Kleinert J, et al. Prevalence of uncontrolled hypertension in patients with Fabry disease. Am J Hypertens. 2006;19:782–7.
Ortiz A, et al. Nephropathy in males and females with Fabry disease: cross-sectional description of patients before treatment with enzyme replacement therapy. Nephrol Dial Transplant. 2008;23:1600–7.
Schiffmann R, et al. Fabry disease: progression of nephropathy, and prevalence of cardiac and cerebrovascular events before enzyme replacement therapy. Nephrol Dial Transplant. 2009;24:2102–11.
Jain G, Warnock DG. Blood pressure, proteinuria and nephropathy in Fabry disease. Nephron Clin Pract. 2011;118:c43–8.
Terryn W, et al. Prevalence of Fabry disease in a predominantly hypertensive population with left ventricular hypertrophy. Int J Cardiol. 2013;167:2555–60.
Branton MH, et al. Natural history of Fabry renal disease: influence of alpha-galactosidase A activity and genetic mutations on clinical course. Medicine. 2002;81:122–38.
Sunderplassmann G. Uncontrolled hypertension in Fabry disease. Am J Hypertens. 2004;17:S206.
Williams B, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:2284–309.
Eknoyan G, et al. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3:5–14.
Lang RM, et al. Recommendations for Chamber Quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
Devereux RB, Roman MJ. Evaluation of cardiac and vascular structure by echocardiography and other noninvasive techniques. In: Laragh JH, Brenner BM, editors. Hypertension: Pathophysiology, Diagnosis, Management, 2nd ed. New York: Raven Press; 1995. p. 1969–85.
Clarkson PB, Prasad N, MacLeod C, Burchell B, MacDonald TM. Influence of the angiotensin converting enzyme I/D gene polymorphisms on left ventricular diastolic filling in patients with essential hypertension. J Hypertens. 1997;15:995–1000.
Mignani R, et al. FAbry STabilization indEX (FASTEX): an innovative tool for the assessment of clinical stabilization in Fabry disease. Clin Kidney J. 2016;9:739–47.
Fastex 2.0 Home page. https://www.fastex.online. Accessed Jan 2020.
Desnick RJ, Chen R, Srinivasan R, Doheny DO, Bishop D. The Fabry disease genotype–phenotype database (dbFGP): an international expert consortium. Mol Genet Metab. 2017;120:S41–2.
Germain DP, et al. Phenotypic characteristics of the p.Asn215Ser (p.N215S) GLA mutation in male and female patients with Fabry disease: a multicenter Fabry Registry study. Mol Genet Genom Med. 2018;6:492–503.
Mutation Search. http://www.dbfgp.org/dbFgp/fabry/Mutation.html. Accessed Jan 2020.
Mezue K, et al. Nocturnal non-dipping blood pressure profile in black normotensives is associated with cardiac target organ damage. Ethn Dis. 2016;26:279–84.
Georgianos PI, Agarwal R. Ambulatory BP phenotypes and their association with target organ damage and clinical outcomes in CKD. Clin J Am Soc Nephrol. 2020;15:441–3.
Schmieder RE. End organ damage in hypertension. Dtsch Arztebl Int. 2010;107:866–73.
Azevedo O, et al. Natural history of the late-onset phenotype of Fabry disease due to the p.F113L mutation. Mol Genet Metab Rep. 2020;22:100565.
Tocci G, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during world hypertension day in Italy. J Clin Hypertens. 2016;18:551–6.
Warnock DG. Fabry disease: diagnosis and management, with emphasis on the renal manifestations. Curr Opin Nephrol Hypertens. 2005;14:87–95.
Mwasongwe SE, et al. Ambulatory blood pressure phenotypes in adults taking antihypertensive medication with and without CKD. Clin J Am Soc Nephrol. 2020;15:501–10.
Williams B, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Rombach SM, et al. Vasculopathy in patients with Fabry disease: current controversies and research directions. Mol Genet Metab. 2010;99:99–108.
DeGraba T, et al. Profile of endothelial and leukocyte activation in Fabry patients. Ann Neurol. 2000;47:229–33.
Napoli C, de Nigris F, Palinski W. Multiple role of reactive oxygen species in the arterial wall. J Cell Biochem. 2001;82:674–82.
Rozenfeld P, Feriozzi S. Contribution of inflammatory pathways to Fabry disease pathogenesis. Mol Genet Metab. 2017;122:19–27.
Baradaran A, Nasri H, Rafieian-Kopaei M. Oxidative stress and hypertension: possibility of hypertension therapy with antioxidants. J Res Med Sci. 2014;19:358–67.
Alroy J, Sabnis S, Kopp JB. Renal pathology in Fabry disease. J Am Soc Nephrol. 2002;13(Suppl 2):S134–8.
Judd E, Calhoun DA. Management of hypertension in CKD: beyond the guidelines. Adv Chronic Kidney Dis. 2015;22:116–22.
Santos PCJL, Krieger JE, Pereira AC. Renin-angiotensin system, hypertension, and chronic kidney disease: pharmacogenetic implications. J Pharmacol Sci. 2012;120:77–88.
Svarstad E, et al. Focal and segmental glomerular sclerosis (FSGS) in a man and a woman with Fabry’s disease. Clin Nephrol. 2005;63:394–401.
Zhou W, Ni Z, Zhang M. Hemizygous Fabry disease associated with membranous nephropathy: a rare case report. Clin Nephrol. 2018;90:227–31.
Maixnerová D, et al. The coincidence of IgA nephropathy and Fabry disease. BMC Nephrol. 2013;14:6.
Ren H, et al. Fabry disease and immunoglobulin A nephropathy presenting with Alport syndrome-like findings: a case report. Medicine. 2019;98:e16256.
Hilz MJ. Autonomic dysfunction in Fabry disease. Clin Ther. 2010;32:S93.
Acknowledgements
Our special thanks go to members of the Renal Research Group (Haukeland University Hospital, University of Bergen, Norway), members of the Fabry Group (San Gerardo Hospital, University of Milano-Bicocca, Italy) for their support.
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E.S. reports receiving a grant from Sanofi Genzyme; positions on the advisory boards of Amicus and Sanofi Genzyme; speaker fees and travel support from Amicus, Sanofi Genzyme, and Shire-Takeda. H.P.M. reports receiving grants from Alexion, Amicus, Sanofi Genzyme, and Shire-Takeda. F.P. reports participations at advisory boards, speaker fees and travel support from Amicus, Sanofi Genzyme, and Shire-Takeda. F.R., H.E., A.B, L.R. and S.A. declare no conflict of interest.
Ethical approval
The research was conducted in accordance with the World Medical Association Declaration of Helsinki and the institute’s Ethics Committee (Comitato Etico Brianza) approved it (DREGC07006/AGAL19211).
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article as additional file.
Code availability
Not applicable.
Author contributions
FR conceived the research design, collected patients’ data, performed the statistical analysis and wrote the manuscript first draft. HPM, ES and HE actively participated in the writing of the manuscript. FP performed the echocardiographic examination. AB, LR and SA collected patients’ data during the clinical visits and implemented the database. HPM, ES and FP provided supervision and mentorship of FR during the drafting. All authors were involved in approving the final version of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rossi, F., Svarstad, E., Elsaid, H. et al. Elevated Ambulatory Blood Pressure Measurements are Associated with a Progressive Form of Fabry Disease. High Blood Press Cardiovasc Prev 28, 309–319 (2021). https://doi.org/10.1007/s40292-021-00450-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-021-00450-0