Abstract
Background
Comprehensive nationwide data on prevalence and distribution of intestinal parasites (IPIs) among pregnant women are lacking. Therefore, the aim of this study was to provide pooled prevalence estimate, prevalence in different regions and species-specific IPIs among pregnant women in Ethiopia.
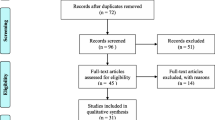
Methods
The search was carried out in Medline via PubMed, Scopus, Science Direct, Web of Science and Google Scholar on published and unpublished data between 2008 and Sep 2020 for studies describing rate of IPIs among pregnant women in Ethiopian. A random-effects model and forest plots to estimate pooled effect size and effect of each study with their confidence interval (CI) were used to provide a visual summary of the data. We conducted meta-regression to understand the source of heterogeneity and pooled the prevalence using ‘metaprop’ command using STATA software version 14.
Results
A total of 3149 of the 9803 pregnant women were infected with one or more species of IPIs resulted in an overall prevalence of 29% (95% CI 22–37%). The prevalence estimate varied among studies with considerable heterogeneity (χ2 = 2069.19, p < 0.001 I2 = 98.84). The prevalence of IPIs was 36% (95% CI 22–50%) in Oromia region, 29% (95% CI 10–47%) in Amhara region, 24% (95% CI 17–32%) in southern nation, nationality and people region, 24% (95% CI 22–27%) in Tigray region and 24% (95% CI 20–29%) in Addis Ababa city. Hookworms with pooled prevalence estimate of 10% (95% CI 8–13%) followed by Ascaris lumbricoides 10% (95% CI 7–13%), and Entamoeba histolytica/dispar 6% (95% CI 4–8%) were the three common species of IPIs identified in this group of population.
Conclusion
The prevalence of IPIs among pregnant women is relatively high in comparison to other general population. Hookworms and Ascaris lumbricoides were the most dominant species of intestinal helminths, whereas Entamoeba histolytica/dispar was the dominant intestinal protozoa among pregnant women in Ethiopia.








Similar content being viewed by others
Availability of data and materials
The data sets generated during and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- NTD:
-
Neglected tropical disease
- IPI:
-
Intestinal parasite infection
- CI:
-
Confidence interval
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- WHO:
-
World Health Organization
References
Savioli L, Stansfield S, Bundy DA, Mitchell A, Bathia R, Engels D, et al. Schistosomiasis and soil-transmitted helminth infections: forging control efforts. Trans R Soc Trop Med Hyg. 2002;96:577.
Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. The lancet. 2006;367:1521–32.
Haque R. Human intestinal parasites. J Health Popul Nutr. 2007;25(4):387.
Bolka A, Gebremedhin S. Prevalence of intestinal parasitic infection and its association with anemia among pregnant women in Wondo Genet district, southern Ethiopia: a cross-sectional study. BMC Infect Dis. 2019;19:483.
Organization WH. 2006 Preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers: World Health Organization.
Blackwell AD. Helminth infection during pregnancy: insights from evolutionary ecology. Int J Women’s Health. 2016;8:651.
Kefiyalew F, Zemene E, Asres Y, Gedefaw L. Anemia among pregnant women in southeast Ethiopia: prevalence, severity and associated risk factors. BMC Res Notes. 2014;7:771.
Alem M, Enawgaw B, Gelaw A, Kena T, Seid M, Olkeba Y. 2013 Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia.
Getachew M, Yewhalaw D, Tafess K, Getachew Y, Zeynudin A. Anaemia and associated risk factors among pregnant women in Gilgel Gibe dam area, southwest Ethiopia. Parasit Vectors. 2012;5:296.
Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasit Vectors. 2014;7:37.
Adegnika AA, Agnandji ST, Chai SK, Ramharter M, Breitling L, Kendjo E, et al. Increased prevalence of intestinal helminth infection during pregnancy in a sub-Saharan African community. Wien Klin Wochenschr. 2007;119:712–6.
Sackey ME, Weigel MM, Armijos RX. Predictors and nutritional consequences of intestinal parasitic infections in rural Ecuadorian children. J Trop Pediatr. 2003;49:17–23.
Tsoka-Gwegweni JM, Ntombela N. A double load to carry: parasites and pregnancy. South Afr J Infect Dis. 2014;29:52–5.
Berhe B, Mardu F, Legese H, Gebrewahd A, Gebremariam G, Tesfay K, et al. Prevalence of anemia and associated factors among pregnant women in Adigrat general hospital, Tigrai, northern Ethiopia, 2018. BMC Res Notes. 2019;12:310.
Feleke BE, Jember TH. Prevalence of helminthic infections and determinant factors among pregnant women in Mecha district, Northwest Ethiopia: a cross sectional study. BMC Infect Dis. 2018;18(1):373.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8:79.
Asrie F. Prevalence of anemia and its associated factors among pregnant women receiving antenatal care at Aymiba Health Center, northwest Ethiopia. J Blood Med. 2017;8:35.
Bekele A, Tilahun M, Mekuria A. Prevalence of anemia and its associated factors among pregnant women attending antenatal care in health institutions of Arba Minch Town, Gamo Gofa Zone, Ethiopia: a crosssectional study. Anemia. 2016. https://doi.org/10.1155/2016/1073192.
Derso A, Nibret E, Munshea A. Prevalence of intestinal parasitic infections and associated risk factors among pregnant women attending antenatal care center at Felege Hiwot Referral Hospital, northwest Ethiopia. BMC Infect Dis. 2016;16:530.
Gebre W. 2012 Intestinal parasitic infection in pregnant women attending antenatal care at Gandhi Memorial Hospital, Addis Ababa, Ethiopia. Accessed on 2019.
Gebrehiwet MG, Medhaniye AA, Alema HB. Prevalence and associated factors of soil transmitted helminthes among pregnant women attending antenatal care in Maytsebri primary hospital, North Ethiopia. BMC Res Notes. 2019;12:644.
Gedefaw L, Ayele A, Asres Y, Mossie A. Anaemia and associated factors among pregnant women attending antenatal care clinic in Walayita Sodo town, southern Ethiopia. Ethiop J Health Sci. 2015;25:155–64.
Getachew M, Tafess K, Zeynudin A, Yewhalaw D. Prevalence soil transmitted helminthiasis and malaria co-infection among pregnant women and risk factors in Gilgel Gibe dam Area, southwest Ethiopia. BMC Res Notes. 2013;6:263.
Getahun W, Belachew T, Wolide AD. Burden and associated factors of anemia among pregnant women attending antenatal care in southern Ethiopia: cross sectional study. BMC Res Notes. 2017;10:276.
Kumera G, Awoke T, Melese T, Eshetie S, Mekuria G, Mekonnen F, et al. Prevalence of zinc deficiency and its association with dietary, serum albumin and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital, Gondar, Northwest Ethiopia. BMC Nutrition. 2015;1:31.
Kumera G, Gedle D, Alebel A, Feyera F, Eshetie S. Undernutrition and its association with socio-demographic, anemia and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital, Northwest Ethiopia. Matern Health, Neonatol Perinatol. 2018;4:18.
Lebso M, Anato A, Loha E. Prevalence of anemia and associated factors among pregnant women in southern Ethiopia: a community based cross-sectional study. PloS one. 2017. https://doi.org/10.1371/journal.pone.0188783.
Melku M, Addis Z, Alem M, Enawgaw B. Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: an institutional based cross-sectional study. Anemia. 2014. https://doi.org/10.1155/2014/108593.
Mengist HM, Demeke G, Zewdie O, Belew A. Diagnostic performance of direct wet mount microscopy in detecting intestinal helminths among pregnant women attending ante-natal care (ANC) in East Wollega, Oromia, Ethiopia. BMC Res Notes. 2018;11:276.
Shiferaw MB, Zegeye AM, Mengistu AD. Helminth infections and practice of prevention and control measures among pregnant women attending antenatal care at Anbesame health center, Northwest Ethiopia. BMC Res Notes. 2017;10:274.
Tefera G. Determinants of anemia in pregnant women with emphasis on intestinal helminthic infection at Sher-Ethiopia Hospital, Ziway. Southern Ethiopia Immunol Infect Dis. 2014;2:33–9.
Tesfaye DJ. Prevalence of intestinal helminthiases and associated factors among pregnant women attending antenatal clinic of Nigist Eleni Mohammed memorial hospital, Hossana, Southern Ethiopia. Open Access Library J. 2015;2:1.
Tulu BD, Atomssa EM, Mengist HM. Determinants of anemia among pregnant women attending antenatal care in Horo Guduru Wollega Zone, West Ethiopia: Unmatched case-control study. PloS one. 2019. https://doi.org/10.1371/journal.pone.0224514.
Weldekidan F, Kote M, Girma M, Boti N, Gultie T. Determinants of anemia among pregnant women attending antenatal clinic in public health facilities at Durame Town: unmatched case control study. Anemia. 2018. https://doi.org/10.1155/2018/8938307.
Yesuf DA, Abdissa LT, Gerbi EA, Tola EK. Prevalence of intestinal parasitic infection and associated factors among pregnant women attending antenatal care at public health facilities in Lalo Kile district, Oromia, Western Ethiopia. BMC Res Notes. 2019;12:735.
Yohannes N, Leykun N, Abebe W, Asrie F. 2016 Buden of intestinal paraciated risk factors among pregnant women attending antenatal care service at Gondar University Hospital, Northwest Ethiopia.
Yatich NJ, Yi J, Agbenyega T, Turpin A, Rayner JC, Stiles JK, et al. Malaria and intestinal helminth co-infection among pregnant women in Ghana: prevalence and risk factors. Am J Trop Med Hyg. 2009;80:896–901.
Kawai K, Saathoff E, Antelman G, Msamanga G, Fawzi WW. Geophagy (soil-eating) in relation to anemia and helminth infection among HIV–infected pregnant women in Tanzania. Am J Trop Med Hyg. 2009;80:36–43.
Ndibazza J, Muhangi L, Akishule D, Kiggundu M, Ameke C, Oweka J, et al. Effects of deworming during pregnancy on maternal and perinatal outcomes in Entebbe, Uganda: a randomized controlled trial. Clin Infect Dis. 2010;50:531–40.
Woodburn PW, Muhangi L, Hillier S, Ndibazza J, Namujju PB, Kizza M, et al. Risk factors for helminth, malaria, and HIV infection in pregnancy in Entebbe, Uganda. PLoS Negl Trop Dis. 2009. https://doi.org/10.1371/journal.pntd.0000473.
Fairley JK, Bisanzio D, King CH, Kitron U, Mungai P, Muchiri E, et al. Birthweight in offspring of mothers with high prevalence of helminth and malaria infection in coastal Kenya. Am J Trop Med Hyg. 2013;88:48–53.
Alli J, Okonko I, Kolade A, Nwanze J, Dada V, Ogundele M. Prevalence of intestinal nematode infection among pregnant women attending antenatal clinic at the University College Hospital, Ibadan. Niger Adv Appl Sci Res. 2011;2:1–13.
Wakabi W. Extension workers drive Ethiopia’s primary health care. The Lancet. 2008;372:880.
Organization WH. 2011 Helminth control in school-age children: a guide for managers of control programmes: World Health Organization.
Brooker S, Hotez PJ, Bundy DA. Hookworm-related anaemia among pregnant women: a systematic review. PLoS Negl Trop Dis. 2008. https://doi.org/10.1371/journal.pntd.0000291.
Hotez PJ, Kamath A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl Trop Dis. 2009. https://doi.org/10.1371/journal.pntd.0000412.
Brooker S, Clements AC, Bundy DA. Global epidemiology, ecology and control of soil-transmitted helminth infections. Adv Parasitol. 2006;62:221–61.
O’lorcain P, Holland C. . The public health importance of Ascaris lumbricoides. Parasitology. 2000. https://doi.org/10.1017/s0031182000006442.
Hall A, Holland C. Geographical variation in Ascaris lumbricoides fecundity and its implications for helminth control. Parasitol Today. 2000;16:540–4.
Quilès F, Balandier J-Y, Capizzi-Banas S. In situ characterisation of a microorganism surface by Raman microspectroscopy: the shell of Ascaris eggs. Anal Bioanal Chem. 2006;386:249–55.
Yimam Y, Woreta A, Mohebali M. Intestinal parasites among food handlers of food service establishments in Ethiopia: a systematic review and meta-analysis. BMC Pub Health. 2020;20:73.
McConnell E, Armstrong J. Intestinal parasitism in fifty communities on the central plateau of Ethiopia. Ethiop Med J. 1976;14:159.
Nikolay B, Brooker SJ, Pullan RL. Sensitivity of diagnostic tests for human soil-transmitted helminth infections: a meta-analysis in the absence of a true gold standard. Int J Parasitol. 2014;44:765–74.
Author information
Authors and Affiliations
Contributions
All authors critically reviewed, provided substantive feedback and contributed to the intellectual content of this paper and made substantial contributions to the conception, conceptualization and manuscript preparation of this systematic review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no competing interests to declare.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chelkeba, L., Melaku, T., Lemma, D. et al. Burden of intestinal parasitic infections among pregnant women in Ethiopia: a systematic review and meta-analysis. Infection 49, 1091–1105 (2021). https://doi.org/10.1007/s15010-021-01635-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-021-01635-4