Abstract
Background
Zinc deficiency during pregnancy has far-reaching consequences on both mother and fetus and subsequent child survival. However, data on the prevalence and determinants of zinc deficiency among pregnant women are scanty and inconclusive. The aim of this study was to assess the prevalence of zinc deficiency and associated factors among pregnant women attending antenatal care at the University of Gondar Hospital, Gondar, Ethiopia.
Methods
Institution based cross-sectional study was conducted at the University of Gondar Hospital from March to May, 2014. A total of 377 pregnant women were selected by systematic sampling technique. Data on socio-demographic factors, reproductive history and nutrition related factors were collected using a structured questionnaire. Blood sample were collected to analyze biochemical indicators. Statistical analysis was done using logistic regression analysis method. P-value < 0.05 at 95 % confidence interval was considered as statistically significance.
Results
The prevalence of zinc deficiency among pregnant women was 57.4 % (95 % CI: 52.2 %– 62.9 %). Living in rural area [AOR = 1.92; 95 % CI (1.04, 3.56)], too close birth [AOR = 3.97; 95 % (1.30, 12.13)], low intakes of diet of animal origin [AOR = 2.29; 95 % CI (1.35, 3.89)], inadequate dietary diversity [AOR = 2.09; 95 % CI (1.24,3.51)], lack of nutrition education [AOR =1.78; 95 % CI (1.10,2.86)], low serum albumin [AOR = 2.55; 95 % CI (1.40,4.63)] and intestinal parasitic infection [AOR = 2.60; 95 % CI (1.49,4.54)] were significantly associated with zinc deficiency.
Conclusion
Zinc deficiency is of public health concern in the study area. To combat the problems, nutrition education to increase knowledge as well as practices concerning the consumption of zinc rich foods and optimal dietary diversity, use of home based phytate reduction techniques and agricultural based approaches should be considered.
Similar content being viewed by others
Background
Zinc (Zn) is an essential trace mineral element vital for many physiological functions and plays an important role in growth, reproduction and immune system. It is necessary for over 300 enzymes required for the synthesis and degradation of carbohydrates, lipids, proteins, and nucleic acids. Furthermore, zinc has an essential role in the maintenance of cell and organ integrity, in the process of genetic expression and as an antioxidant and anti-inflammatory agent [1–5].
Zinc deficiency (ZD) during pregnancy has an adverse effect on both mother and fetus and on subsequent birth outcomes. Major problems associated with zinc deficiency include growth retardation, delayed immune system development, cognitive impairment, impaired glucose tolerance, low birth weight, congenital malformations, pregnancy-induced hypertension and increased risk of abortion, miscarriage, stillbirths, preterm labour, postpartum hemorrhage and prolonged labor [1, 3, 6–8].
Various studies conducted over years have provided evidence that ZD is a worldwide public health problem [8, 9]. World Health Organization(WHO) estimates that zinc deficiency affects 31 % with the prevalence rates ranging from 4 to 73 % in various regions of the world’s population [9]. In developing countries zinc deficiency is one of the ten significant factors contributing to burden of disease [3]. According to a report on global and regional child mortality and burden of disease attributable to zinc deficiency, Africa suffers 58 % of child deaths attributable to zinc deficiency. Ethiopia is one of the five countries who together contribute 47 % of the child deaths attributable to zinc deficiency in Africa [10]. According to Ethiopia Demographic and Health Survey (EDHS) 2011, nearly 44 % of the under-five children are stunted. Stunting in children is considered as an indirect indicator of zinc nutritional status [11].
The limited available reports indicate that zinc deficiency is of public health problems in Ethiopian pregnant women. In Ethiopia, few studies determined the prevalence of ZD in pregnant women and came up with figures ranging from 53 to 76 % [12–15]. All the studies consistently witnessed the public health significance of ZD in the country. Other studies conducted in Kenya [16], Sudan [17], Cameroon [18], India [19], Nepali [20] and Iran [21] also reported high prevalence figures.
Although ZD is increasingly being recognized as a widespread problem, currently, there is no precise data regarding the magnitude and severity of ZD in pregnant women [22]. This lack of information on population zinc status has been a major limiting factor in expansion of interventions to control zinc deficiency [23]. Almost nothing is being done in Ethiopia to address zinc deficiency of this magnitude except for the short-term zinc supplementation targeting children with diarrhea.The present study aims at assessing the prevalence and factors associated with ZD among pregnanat women.
Methods
Study design, area and population
An institution based cross-sectional study was conducted from March to April, 2014. The period was neither food insecured nor harvest season. The study was conducted at the University of Gondar (UOG) Hospital in Gondar, Northwest Ethiopia. The University of Gondar Hospital is a tertiary-level teaching and service-rendering institution that provides health service to over 4 million people in Northwest Ethiopia. The Gondar town lies on the average at 2,300 meters above sea level and over 350,000 population reside in this administrative town. The study populations were all pregnant women in Gondar town and the surrounding area who attend antenatal care (ANC) at University of Gondar Hospital.
Sample size and sampling technique
Sample size for estimating the prevalence of ZD was computed using single population proportion sample size calculation formula with the inputs of 95 % confidence level, 5 % of margin of error, non-response rate of 10 % and expected prevalence of ZD of 66.7 % [13]. Accordingly, sample size of 377 was computed. A systematic random sampling technique was used to select the study subjects. According to the Hospital report, around 1080 pregnant women have been enrolled to ANC. On average, 30–40 pregnant women visit ANC daily. Since the sample size was determined as 377, hence a sampling interval of 3 was used to select study participants. Of the first three subjects, one woman was randomly selected by lottery method, and then every 3rd pregnant women was selected to participate in the study until the required sample size of 377 pregnant women was obtained. To avoid double enumeration the client chart number was used and after data was collected code was given to the client chart.
Data collection method
Questionnaire
Data on potential determinants of ZD were collected using structured and pretested questionnaire through interview. The content validity of the questionnaire was checked against the conceptual framework of the study. Five data collectors (three mid wives and two laboratory technicians) and one supervisor were recruited. Training was given for them by the principal investigator. The data collection process was followed daily by the supervisor and principal investigator. The questionnaire was administered in local language.
The parts of the questionnaire on dietary diversity were adopted from Food and Agriculture Organization of the United Nations (FAO) guidelines for measuring household and individual dietary diversity [24]. The Standard English version of the questionnaire was translated to local language by an expert to insure its consistency, and locally available foods were also considered. The translated Amharic version (local language) was pre-tested prior to the actual survey and modifications were made accordingly. Training was given for data collectors and supervisor to have consensus and the same understanding of what is intended to be measured by each question in the questionnaire.
The women dietary diversity (WDD) level was assessed using 24 h recall method. Respondents were asked whether they had taken any food from predefined 9 food categories in the previous day of the survey. Accordingly, the level of DD was computed out of the score of 9. The mean DD score of the study subjects was computed. DD score less than the mean was categorized as inadequate DD whereas, DD score greater than the mean was categorized as adequate DD.
Nutrition education (prenatal dietary advice) received were assessed using the items adapted from the national nutrition survey conducted by the Ethiopian Health and Nutrition Institute in 2009. Prenatal dietary advice was constructed by combining three items that asked the woman whether she received each of the following advices: (1) advised to eat a balanced diet, (2) advised to eat more and (3) advised to eat different fruits and vegetables in this pregnancy. A value of 1 was assigned if the pregnant woman answered yes to each item and 0 was assigned otherwise. Then, an aggregate variable, Nutrition education (prenatal dietary advice), with possible values ranging from 0 to 3 was constructed from the linear combination of the responses on the above items. The scores of prenatal dietary advice were recorded to develop dichotomous variable that divided the respondent who received any prenatal dietary information and those who did not.
The last date of the menstrual period and/or fundal height with subsequent pregnant urine test were used to diagnose pregnancy. Pregnant women from all trimesters (first, second and third) were included in the study. Mid upper arm circumference (MUAC) was measured half way between the olecranon process and acromion process using non stretchable tape to the nearest 0.1 cm to determine the nutritional status of the participants.
Laboratory analysis
Blood collection, Serum separation and zinc level determination
About 5 ml of venous blood was collected from each pregnat women, using sterile trace element-free evacuated blood collection tubes. The blood was allowed to clot for 20 minutes, centrifuged at 3000 rotations per minute for 10 minutes, and sera were separated from the cells following standard procedures. Visibly hemolyzed samples were identified and discarded. Serum were kept frozen at −20 °C at the ART Laboratory of UOG Hospital, until transported to the laboratory of the Ethiopian Public Health Research Institute (EPHRI). Serum was kept in an ice box during transport. Serum zinc concentration was determined at EPHRI using Shimadzu Flame Atomic Absorption Spectroscopy (AA 6800 model, Japan). Zinc deficiency was defined as a serum zinc level of less than 56 μg/dl during the first trimester, or less than 50 μg/dl during the second or third trimester [25].
Hemoglobin and albumin level determination
Hemoglobin level was determined using hematological analyzer (Cell Dyn 1800, PD, USA) machine. Anemia was defined as a hemoglobin level of (at sea level) less than 11.0 g/dl during the first or third trimester or less than 10.5 g/dl during the second trimester [26]. According to the formula recommended by Center for Disease Prevention and Control, hemoglobin values were adjusted for altitude [27]. Albumin level was measured by Roche cobas intgera® 400 plus chemistry analyzer (Roche Diagnostic, Germany).
CRP, fasting status and time of blood sample collection
CRP was determined qualitatively using CRP-Latex (08390 Montgat, Barcelona, Spain) following the procedure provided with the kit. Both nonfasting and fasting blood samples were collected following standard procedures for serum zinc analysis. Fasting was defined as no intake of food or beverage in the preceding 8 h of the sample collection [28]. Blood sample was drawn both in the morning and afternoon.
HIV status determination
Rapid test for HIV (1/2) antibody from whole blood was performed by serial testing algorithm. The algorithm includes KHB (Shanghai kehua Bioengineering CO-Ltd, Shanghai, China) as a primary test and HIV 1/2 STAT-PAK™ (Chembio HIV1/2, Medford, New york, USA) as a secondary test and Uni-Gold TM (Trinity Biotech PLC, Bray, Ireland) as a tie breaker.
Stool specimen collection and examination
About two gram of stool samples were collected from participants using clean, dry and leak proof cupped plastic container following standard procedures. About 50 mg of stool was mixed with normal saline (0.85 % NaCl) and processed using direct saline wet mount to diagnose intestinal parasite/s. In the case of formol-ether concentration technique, 1 gram of stool was preserved by 10 % formalin and diagnosed for intestinal parasites [29].
Data processing and analysis
Data were entered using EPI-INFO version 7 software. Analysis was carried out using SPSS version 20 statistical program. Descriptive analysis was carried out using mean, frequency and percentage. Wealth index quintiles (poor, middle and rich) were computed using Principal component analysis. Bivariate and multivariable logistic regression analysis were used to assess the relative effect of various explanatory variables on the dependent variable and to control potential confounders. Absence of multicollinearity was checked using VIF/tolerance. The fitness of logistic regression model was checked using Hosmer-Lemeshow statistic test. P-value < 0.05 at 95 % CI was considered statistically significant.
Ethical consideration
The study was conducted in confirmation of national and international ethical guidelines for biomedical research involving human subjects. Ethical clearance was obtained from ethical review committee of University of Gondar. Written informed consent was obtained from each study participant after the purpose of the study explained. Needle safety procedures was in line with WHO standard. Nutrition education was given to all study participants. Anemic women were given iron supplementation. Women who had intestinal parasites were treated accordingly.
Results
Socio-demographic characteristics of the study subjects
Of 377 pregnant women recruited, 364 were willing to take part in the study, with a response rate of 96.5 %. The mean age of the mothers was 26.7 years (±4.7 years) of standard deviation, with a range of 25 (16, 41). The vast majority of the respondents were Amhara in ethnicity (95.3 %) and orthodox (88.5 %) in religion. A relatively small proportion of the participants, 73(20.1 %) had no formal education and more than half, 199 (54.7 %) were housewives. More than three-fourth, 294 (77.2 %), of the respondents were urban dwellers. The mean monthly household income was 2519 birr. The average family size was 3.36 (±1.7) (Table 1).
Environmental and sanitation factors
The vast majority of participants, 344(94.5 %) had toilet facilities. The greater number of study subjects, 259(75.3 %) use pit latrine. Source of drinking water for majority, 324(89 %) of study participants was tap water. Among pregnant women who used other soursces of drinking water other than tab water the risk of zinc deficiency tend increase. Among 12 pregnant women who consumed well water, 9(75 %) were zinc deficienct. Similarly among 28 pregnant women who consumed spring water, 22(78.6 %) were zinc deficienct (Table 2).
Clinical factors and Zinc deficiency
Small proportion, 13(3.6 %) of the pregnant women were positive for HIV. Among 13 prganant women who were positive for HIV, 10(76.9 %) were zinc deficienct. The mean zinc levels for HIV positive and negative samples were 40.3(±15.2) and 48.3(±21.8) μg/dl, respectively. Of all pregnant women, 79(21.7 %) were taking iron supplement at least once in the preceding four weeks of the survey. Small proportion, 24(6.6 %) of the respondents had diarrhea; of whom more than three-fourth, 19 (79.2 %) were zinc deficient. One - third, 119(32.7 %) of the pregnant women had anemia on the basis of their hemoglobin levels. Among anemic women, more than two third, 78(65.5 %), were zinc deficient. Similarly, among zinc deficient women, 78 (37.3 %) had anemia. Nearly one - fifth, 83(22.8 %) of the pregnant women were undernourished (MUAC ≤ 21 cm). The findings of the present study showed that, 88(24.2 %) of the prganant women had low serum albumin level (<3.2 g/dl). Among albumin deficienct women, three-fourth, 66(75 %) were zinc deficient (Table 3).
Intestinal parasitic infection among the study participants
More than quarter, 105(28.8 %) of the study participants were infected with one or more intestinal parasites. The most common parasites observed were Entamoeba histolytica 45(42.9 %) and Ascaris lumbricoides 28(26.7 %). Intestinal parasitic infection tend increase among rural dwellers. Of 83 rural dwellers pregnant women, 61(73.5 %) were infected with one or more intestinal parasites (Table 4).
Reproductive health factors
Around 165 (45.3 %), of participants had first pregnancy at a time of data collection. The mean parity of the study participants was 1.21 (±1.64), ranging between 0 and 7 pregnancies. Among 199 women who gave at least a birth in the previous 5 years of the survey, small proportion of the participants, 31(8.5 %) had birth interval less than the recommended two years. Nearly half, 192(52.7 %), of the study participants was in the third trimester of pregnancy (Table 5).
Nutrition related characteristics
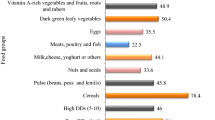
The staple diets for the vast majority, 343 (94.2 %), of the study participants was Teff (Fig 1). The meal frequency was three or more times a day for the majority of the study participants 325(89.3 %). The results revealed that more than a half, 225(61.8 %) of the study participants were consuming coffee. The mean dietary diversity (DD) of the study participants was 3.35 (±0.77), ranging between 1 and 6. The majority of study participants, 230 (63.2 %) had low DD score (≤3 food groups). The highest consumed food groups by the study participants were starchy staple, 363(99.7 %) and legumes and nuts, 259(71.2 %) (Fig 2). Only about one-third, 124 (34.1 %) of pregnant women were consumed diet of animal origin (Table 6).
C - Reactive Protein (CRP), Time of blood sample collection and Fasting status
The majority of the samples 275(75.5 %) were collected at the morning. The mean zinc levels for samples collected in the morning and afternoon were 49 (±22.1) and 45 (±20.2) μg/dl, respectively. The greater majority of the participants were in non-fasting status 291(79.9 %). The mean zinc concentrations for fasting and non-fasting subjects were 44.6 (±20.3) and 48.9 (±21.9) μg/dl respectively. About 76(20.9 %) of the samples were positive for CRP test. The mean zinc levels for CRP positive and negative samples were 45.12 (±18.8) and 48.82 (±22.3) μg/dl, respectively.
Prevalence of zinc deficiency
The prevalence of zinc deficiency among pregnant women was 57.4 % (95 % CI: 52.2 % – 62.9 %). The mean serum zinc concentration was 48.1(±21.6) μg/dl. The value ranged from 10.5 to 102.8 μg/dl. The prevalence of ZD during the first, second and third trimesters were 15.8, 30.6 and 53.6 %, respectively. The mean serum zinc levels for the first, second and third trimesters were 53.1 (±21.6), 47.2(±21.7) and 46.9 (±21.6) μg/dl, respectively.
Factors associated with zinc deficiency
Multivariable logistic regression analysis was computed to identify predictors of zinc deficiency among study participants. Variables which significantly associated to the dependent variable in bivariate regression models were exported to a multivariable regression model for adjustment. Independent variables that showed association on the bivariate logistic regression model include: residence, source of drinking water, diarrhea, birth interval, sorghum consumption, coffee intake, animal source food, dietary diversity, nutrition education, serum albumin and intestinal parasite. The multivariable logistic regression analysis revealed that residence, birth interval, animal source food, dietary diversity, nutrition education, serum albumin and intestinal parasite were variables which significantly associated to zinc deficiency (Table 7).
Residence was significantly associated with zinc deficiency (P = 0.037). Pregnant women living in rural area were two times more likely to be zinc deficient as compared to those living in urban areas [AOR = 1.92; 95 % CI (1.04, 3.56)]. Birth interval was also significantly associated with zinc deficiency (P = 0.016). Pregnant women with short birth interval(<2 yr) were four times more likely to be zinc deficient as compared to pregnant women with no birth [AOR = 3.97; 95 % (1.30,12.13)]. Significant associations were also observed between zinc status and diet of animal origin. Compared to pregnant women who consumed animal source foods, the risk of ZD was 2.29 times higher among those who did not consume animal source foods in the reference period [AOR = 2.29; 95 % CI (1.35, 3.89)]. Similarly compared to pregnant women with adequate DD Score (DDS ≥ 4), the risk of ZD was two times higher among those with inadequate DDS (DDS ≤ 3) [AOR = 2.09; 95 % CI (1.24, 3.51)]. Nutrition education and zinc status were positively associated (P = 0.02). Pregnant women who did not recieve nutrition education was 1.78 times at greater risk of being zinc deficient compared to those who recieved nutrition education during pregnancy [AOR =1.78; 95 % CI (1.10, 2.86)]. Serum albumin was also positively associated with zinc status (P = 0.002). Albumin deficient pregnant women had two and half fold [AOR = 2.55; 95 % CI (1.40, 4.63)] greater risk of being zinc deficient compared to those with normal serum albumin levels. Intestinal parasite was also found to be significantly associated with zinc status. Pregnant women who had one or more intestinal parasitic infection were 2.6 times more likely to be zinc deficient as compared to those who had no intestinal parasitic infection [AOR = 2.60; 95 % CI (1.49, 4.54)].
Discussion
In the current study, more than half, (57.4 %) of pregnant women had biochemical evidence of zinc deficiency based on low serum zinc concentrations. According to the International Zinc Nutrition Consultative Group (IZiNCG), the risk of zinc deficiency is of public health concern when the prevalence of low serum zinc concentrations is greater than 20 % [6]. Hence, the study provide evidence for the public health significance of zinc deficiency in the study area.
The result of the present study was relatively similar with study conducted in Southern Ethiopia 53 % [12] and Nepal 61 % [20]. However, relatively lower than other reports from Ethiopia; prevalence of ZD was 76 % [30], 74 % [15] and 72 % [14] in Sidama and 66.7 % [13] in Gondar. It was also relatively lower than study from other countries, Kenya 66.9 % [16], Cameroon 82 % [18], and India 73.5 % [31]. The previous studies reported severe deficiency situation compared to the present study. The variation can be explained by different cut-offs of serum zinc levels that were used and seasonal difference in data collection. Further, the prevalence may have overestimated as only pregnant women in the third trimester was included in the study from Sidama and India. Other possible explanation may be urban–rural difference, as the previous studies in India and Sidama targeted only rural areas.
The result of the present study was relatively higher than reports from Eastern Sudan (38 %) [32], Central Sudan (45 %) [17], Malawi (36 %) [33], Vietnam 29 % [34], Bangladesh 14.7 % [35], and Iran 49 % [21]. The reason for this difference probably is due to nutritional regiment; cultural differences in food preparation and feeding habit. Further, the studies may have underestimated the problem as they only included pregnant women in early pregnancy in study from Bangladesh and Vietnam.
The existence of low biochemical zinc status was attributed to seven major factors: living in rural areas, too close births, inadequate dietary diversity, low intakes of foods of animal origin, lack of nutrition education, low serum albumin and intestinal parasitic infection, each of which is discussed below.
Residence was significantly associated with zinc deficiency. Pregnant women from urban area were better-off in their zinc status as compared to pregnant women from rural areas. This finding is comparable to study from Cameroon [18]. This might be due to reason that pregnant women who lives in rural areas had low nutritional awareness, were likely to be more disadvantaged and thus will be more vulnerable to food shortage and micronutrient deficiencies. Further, pregnant women from rural areas were more likely to be involved in laborious activities, as chronic overexertion is a predisposing factor to maternal nutritional depletion [36].
Birth interval was one of a significant factor influencing the biochemical zinc status of pregnant women. Pregnant women with short birth interval(<2 yr) had four fold greater risk of being zinc deficient as compared to pregnant women with no birth. The study finding showed deleterious effect of too close birth on zinc status. This study is in line with previous studies conducted in India [37] and Southern Ethiopia [12]. The study finding agrees with the understanding that too close births and repeated pregnancies deplete maternal nutritional store. However, study conducted in Turkey did not find any significant association between zinc status and birth interval [38]. The variation might be explained by difference in socioeconomic status and nutritional care prior to and during pregnancy.
Albumin deficient pregnant women had two and half fold greater risk of being zinc deficient compared to those with adequate serum albumin levels. The current study finding witnessed a highly significant positive association between serum albumin and serum zinc level. Previous study conducted in Malawi also supported the finding [33]. The finding is parallel to the knowledge that serum zinc concentration declines in concert with serum albumin during pregnancy, due to expansion in plasma volume. Serum zinc concentration also falls with the hypoalbuminemia, which influences absorption and transport of zinc [39, 40].
Intestinal parasitic infection was found to be negatively associated with zinc status. Pregnant women who had one or more intestinal parasitic infection were 2.6 times more likely to be zinc deficient than pregnant women with no intestinal parasites. In current study, 105 (28.8 %) of study participants were infected with one or more intestinal parasites. Of whom three-fourth, 79 (75.2 %) were zinc deficient. Zinc deficiency due to intestinal parasitoses might be due to increased fecal losses of Zn through diarrhea, blocking of the absorbing surface of the mucosa by adult worms and intestinal bleeding [39, 41, 42].
Pregnant women who did not receive nutrition education during pregnancy was at greater risk of being zinc deficient as compared to those who received nutrition education. One recent study in Southern Ethiopia failed to witness any definite trend on the effect of nutrition education on maternal zinc status [12]. However, the present study showed a positive association between nutrition education and zinc status. This might be due to the reason that nutrition education might have contributed to optimal zinc status through enhancing good nutritional awareness and practice of pregnant women.
The present study showed that low dietary zinc intake is one of the main contributing factors in the development of zinc deficiency. Compared to pregnant women with adequate DDS the risk of ZD was two times higher among those with inadequate DDS. This finding is comparable to study from Southern Ethiopia [12]. Foods of animal origin was also significantly associated with biochemical zinc status of pregnant women. Compared to pregnant women who consumed animal source foods, the risk of ZD was 2.29 times higher among those who did not consume animal source foods in the reference period. Previous studies conducted in Malawi [33] and Southern Ethiopia [12] also supported the finding.
The present study revealed a high dependency on consumption of cereals, 363(99.7 %) and legumes, 259(71.2 %) in the study community. Such diets contains high level of phytates, which are the most potent inhibitor of zinc absorption [40, 43]. Only one-third, 124 (34.1 %) of pregnant women were consumed diet of animal origin, which are good sources of bioavailable zinc [40]. The heavy dependence on plants diets (cereals and legumes), which have low zinc bio availability and minimal intake of foods of animal origin, which are a rich source of readily available zinc, could suggest the role of phytate in exacerbating the zinc deficiency in the study area. Cereals and legumes do contribute relatively high amounts of zinc but also contribute importantly to phytate intake. Thus, the high prevalence of zinc deficiency in the present study could be partially explained by the poor zinc absorption from the plant-based diets. However, inadequate intake of zinc rather than low bioavailability might be the main risk factor for the zinc deficiency in pregnant women from the study area. High prevalence of zinc deficiency in the present study might be also partially explained by low zinc content of Ethiopian soil, as crops grown locally will have low zinc concentration and households who depend entirely on locally grown crops will be at risk of inadequate zinc intake [41, 44, 45].
Our study also showed positive relationship between zinc deficiency and anemia. ZD and anemia tend to occur together. About 73 (34.9 %) of the subjects had both deficiencies. A previous studies also found significant positive association between zinc deficiency and anemia [12, 15, 32, 46]. As the studies are cross-sectional it is not viable to implicate causal inference. Nevertheless, as zinc is known to participate in multiple metabolic pathways, it might have causal role in anemia. This relation between ZD and anemia might be due to the role of zinc in erythropoiesis or the common dietary sources of iron and zinc [15, 47, 48].
The major limitation of this study was the study design as cross-sectional study design by its nature limits information about cause and effect relationship in the majority of predictors. Secondly, the study was facility based and the participants may not represent the general population. Assessment of dietary intake depends on the 24 hour recall method, which may not accurately reflect their past feeding experience.
Conclusion
Zinc deficiency is of a public health concern among pregnant women in the study area. Living in rural areas, too close births, inadequate dietary diversity, low intakes of foods of animal origin, lack of nutrition education, low serum albumin and intestinal parasitic infection are key predisposing factors to zinc deficiency. The problem must be combated through implementation of strategies like promoting higher agricultural productivity and diversity, use of zinc containing fertilizers and rural livelihood promotion and empowerment of women. We also suggest sustained nutrition education to increase knowledge as well as practices concerning the consumption of zinc rich foods and optimal dietary diversity, use of home based phytate reduction techniques, homemade water treatment practices especially in rural community and use of effective methods of contraception to reduce frequent reproductive cycling. Multicentric studies in various parts of the country should be conducted to substantiate the data obtained in the present study so that intervention measures can be initiated.
Abbreviations
- ANC:
-
Antenatal Care
- CRP:
-
C-reactive protein
- DD:
-
Dietary Diversity
- DDS:
-
Dietary Diversity Score
- EPHRI:
-
Ethiopian Public Health Research Institute
- FAO:
-
Food and Agriculture Organization of the United Nations
- MUAC:
-
Mid Upper Arm Circumference
- UOG:
-
University of Gondar
- WHO:
-
World Health Organization
- Zn:
-
Zinc
- ZD:
-
Zinc Deficiency
References
Prasad AS. Discovery of human zinc deficiency: its impact on human health and disease. Ad Nut An Int Rev J. 2013;4(2):176–90.
DiSilvestro RA. Zinc in relation to diabetes and oxidative disease. J Nutr. 2000;130(5):1509S–11S.
Khalid N, Ahmed A, Bhatti MS, Randhawa MA, Ahmad A, Rafaqat R. A Question Mark on Zinc Deficiency in 185 Million People in Pakistan—Possible Way Out. Crit Rev Food Sci Nutr. 2014;54(9):1222–40.
Bhaskaram P. Micronutrient malnutrition, infection, and immunity: an overview. Nutr Rev. 2002;60 suppl 5:S40–5.
Joint FAO, WHO. Vitamin and mineral requirements in human nutrition. Joint Food and Agriculture Organization of the United Nations, World Health Organization; 2005.
Brown KH, Hess SY. International Zinc Nutrition Consultative Group Technical Document No. 2: systematic reviews of zinc intervention strategies. Food Nutr Bull. 2009;30:S5–S184.
Mahomed K, Bhutta ZA, Middleton P. Zinc supplementation for improving pregnancy and infant outcome, The Cochrane Library. 2007.
Roohani N, Hurrell R, Kelishadi R, Schulin R. Zinc and its importance for human health: An integrative review. J Res Med Sci. 2013;18(2):144.
Caulfield LE, Black RE. Zinc deficiency. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. World Health Org. 2004;1:257–80.
Walker CF, Ezzati M, Black R. Global and regional child mortality and burden of disease attributable to zinc deficiency. Eur J Clin Nutr. 2009;63(5):591–7.
IZiNCG. Assessment of the risk of zinc deficiency in populations and options for its control. International Zinc Nutrition Consultative Group Technical document #1; 2004.
Gebremedhin S, Enquselassie F, Umeta M. Prevalence of prenatal zinc deficiency and its association with socio-demographic, dietary and health care related factors in Rural Sidama, Southern Ethiopia: A cross-sectional study. BMC Public Health. 2011;11(1):898.
Kassu A, Yabutani T, Mulu A, Tessema B, Ota F. Serum zinc, copper, selenium, calcium, and magnesium levels in pregnant and non-pregnant women in Gondar, Northwest Ethiopia. Biol Trace Elem Res. 2008;122(2):97–106.
Abebe Y, Bogale A, Hambidge KM, Stoecker BJ, Arbide I, Teshome A, Krebs NF, Westcott JE, Bailey KB, Gibson RS. Inadequate intakes of dietary zinc among pregnant women from subsistence households in Sidama, Southern Ethiopia. Public Health Nutr. 2008;11(04):379–86.
Gibson RS, Abebe Y, Stabler S, Allen RH, Westcott JE, Stoecker BJ, Krebs NF, Hambidge KM. Zinc, gravida, infection, and iron, but not vitamin B-12 or folate status, predict hemoglobin during pregnancy in Southern Ethiopia. J Nutr. 2008;138(3):581–6.
Mitheko A, Kimiywe J, Njeru PN. Dietary, Socio-economic And Demographic Factors Influencing Serum Zinc Levels Of Pregnant Women At Naivasha Level 4 Hospital Nakuru County, Kenya. 2013.
Bushra M, Elhassan EM, Ali NI, Osman E, Bakheit KH, Adam II. Anaemia, zinc and copper deficiencies among pregnant women in central Sudan. Biol Trace Elem Res. 2010;137(3):255–61.
Engle-Stone R, Ndjebayi AO, Nankap M, Killilea DW, Brown KH. Stunting prevalence, plasma zinc concentrations, and dietary zinc intakes in a nationally representative sample suggest a high risk of zinc deficiency among women and young children in Cameroon. J Nutr. 2014;144(3):382–91.
Pathak P,KU, Dwivedi SN, Singh R. Serum zinc levels amongst pregnant women in a rural block of Haryana state, India. Asia Pac J Clin Nutr. 2008;17:2.
Jiang T, Christian P, Khatry SK, Wu L, West KP. Micronutrient deficiencies in early pregnancy are common, concurrent, and vary by season among rural Nepali pregnant women. J Nutr. 2005;135(5):1106–12.
Salimi S, Yaghmaei M, Joshaghani H, Mansourian A. Study of zinc deficiency in pregnant women. Iranian J Pub Health. 2004;33(3):15–8.
Shah D, Sachdev H. Effect of gestational zinc deficiency on pregnancy outcomes: summary of observation studies and zinc supplementation trials. Br J Nutr. 2001;85(S2):S101–8.
Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PLoS One. 2012;7(11):e50568.
FAO. Guidelines for measuring household and individual dietary diversity. Food and Agriculture Organization of the United Nations; 2011.
International Zinc Nutrition Consultative Group., Assessing population zinc status with serum zinc concentration. IZiNCG Technical Brief, 2007(2).
Earl R, Woteki CE. Iron Deficiency Anemia: Recommended Guidelines for the Prevention, Detection, and Management Among US Children and Women of Childbearing Age. Washington, D.C.: National Academy Press; 1994.
Nestel P. Adjusting hemoglobin values in program surveys. Washington, DC: International Nutritional Anaemia Consultative Group, ILSI Human Nutrition Institute; 2002. p. 2–4.
King JC. Determinants of maternal zinc status during pregnancy. Am J Clin Nutr. 2000;71(5):1334s–43s.
World Health Organization. Bench aids for the diagnosis of intestinal parasites. 1994.
Stoecker B, Abebe Y, Hubbs-Tait L, Kennedy T, Gibson R, Arbide I, Teshome A, Westcott J, Krebs N, Hambidge K. Zinc status and cognitive function of pregnant women in Southern Ethiopia. Eur J Clin Nutr. 2009;63(7):916–8.
Pathak P, Kapil U, Kapoor SK, Saxena R, Kumar A, Gupta N, Dwivedi SN, Singh R, Singh P. Prevalence of multiple micronutrient deficiencies amongst pregnant women in a rural area of Haryana. Indian J Pediat. 2004;71(11):1007–14.
Mohamed AA, Ali AAA, Ali NI, Abusalama EH, Elbashir MI, Adam I. Zinc, parity, infection, and severe anemia among pregnant women in Kassla, Eastern Sudan. Biol Trace Elem Res. 2011;140(3):284–90.
Gibson RS, Huddle J-M. Suboptimal zinc status in pregnant Malawian women: its association with low intakes of poorly available zinc, frequent reproductive cycling, and malaria. Am J Clin Nutr. 1998;67(4):702–9.
Nguyen VQ, Goto A, Nguyen TVT, Vo KT, Ta TMT, Nguyen TNT, et al. Prevalence and correlates of zinc deficiency in pregnant Vietnamese women in Ho Chi Minh City. Asia Pac J Clin Nutr. 2013;22:4.
Shamim AA, Kabir A, Merrill RD, Ali H, Rashid M, Schulze K, Labrique A, West KP, Christian P. Plasma zinc, vitamin B12 and α-tocopherol are positively and plasma γ-tocopherol is negatively associated with Hb concentration in early pregnancy in north-west Bangladesh. Public Health Nutr. 2013;16(08):1354–61.
Deshpande JD, Joshi MM, Giri PA. Zinc: The trace element of major importance in human nutrition and health. Int J Med Sci Public Health. 2013;2(1):1–6.
Rathi SS, Srinivas M, Grover J, Mitra D, Vats V, Sharma J. Zinc levels in women and newborns. Indian J Pediat. 1999;66(5):681–4.
Meram I, Bozkurt AI, Ahi S, Ozgur S. Plasma copper and zinc levels in pregnant women in Gaziantep, Turkey. Saudi Med J. 2003;24(10):1121–5.
Brown KH, Wuehler SE, Peerson JM. The importance of zinc in human nutrition and estimation of the global prevalence of zinc deficiency. Food Nutrition Bulletin. 2001;22(2):113–25.
Brown KH, Rivera J, Bhutta Z, Gibson R, King J, Lönnerdal B, Ruel M, Sandtröm B, Wasantwisut E, Hotz C. International Zinc Nutrition Consultative Group (IZiNCG) technical document# 1. Assessment of the risk of zinc deficiency in populations and options for its control. Food Nutr Bull. 2004;25(1 Suppl 2):S99–S203.
Nriagu J: Zinc deficiency in human health. [http://www.extranet.elsevier.com/homepage_about/mrwd/nvrn/Zinc%20Deficiency%20in%20Humans.pdf]
Gibson RS. Zinc: the missing link in combating micronutrient malnutrition in developing countries. Proc Nutr Soc. 2006;65:51–60.
Lönnerdal B. Dietary factors influencing zinc absorption. J Nutr. 2000;130(5):1378S–83S.
Cakmak I. Enrichment of fertilizers with zinc: An excellent investment for humanity and crop production in India. J Trace Elem Med Biol. 2009;23(4):281–9.
Lambein F, Haque R, Khan JK, Kebede N, Kuo Y-H. From soil to brain: zinc deficiency increases the neurotoxicity of Lathyrus sativus and may affect the susceptibility for the motorneurone disease neurolathyrism. Toxicon. 1994;32(4):461–6.
Borna S, Haghollahi F, Golestan B, Norouzi M, Hanachi P, Shariat M, Sh N. A comparative study of Zinc deficiency prevalence in pregnant and non pregnant women. Tehran Univ Med Sci. 2009;67:5.
De Jong N, Romano ABA, Gibson RS. Zinc and iron status during pregnancy of Filipino women. Asia Pac J Clin Nutr. 2002;11(3):186–93.
Folin M, Contiero E, Vaselli GM. Zinc content of normal human serum and its correlation with some hematic parameters. Biometals. 1994;7(1):75–9.
Acknowledgements
We would like to thank the staff of ART laboratory (especially Mr. Yohannis Sinku), University of Gondar Hospital and Ethiopian Public Health Research Institute for their full cooperation and vital assistance during data collection and conducting the laboratory analysis. We also gratefully acknowledge the following persons who participated in various aspects of the research process: Meseret Woldeyohannes, Adamu Belay, Feyissa Challa, and Azeb Atnafu. We acknowledge save the children for funding the study. Special thanks go to entire study subjects for their full participation in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
No competing interests.
Authors’ contributions
GK participated in study protocol development, data collection, analysis, write-up and drafting of the manuscript. TA, TM and SE assisted in reviewing proposal, data analysis and write up. DG, TE, FM and GM assisted in data collection, data analysis and write up. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kumera, G., Awoke, T., Melese, T. et al. Prevalence of zinc deficiency and its association with dietary, serum albumin and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital, Gondar, Northwest Ethiopia. BMC Nutr 1, 31 (2015). https://doi.org/10.1186/s40795-015-0026-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-015-0026-6