Abstract
Purpose
Aortic valve replacement remains the only viable solution for symptomatic patients with severe aortic valve stenosis. Despite their improved design and long history of successful operation, bileaflet mechanical heart valves are still associated with post-operative complications leading to valve dysfunction. Thus, the flow dynamics can be highly disturbed downstream of the dysfunctional valve.
Methods
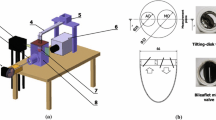
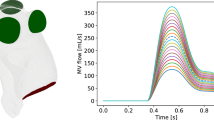
In this in vitro study, the flow dynamics downstream of healthy and dysfunctional bileaflet mechanical heart valves have been investigated using particle image velocimetry measurements. Proper orthogonal decomposition of the velocity field has been performed in order to explore the coherent flow features in the ascending aorta in the presence of a dysfunctional bileaflet mechanical heart valve.
Results
The ability of proper orthogonal decomposition derived metrics to differentiate between heathy and dysfunctional cases is reported. Moreover, reduced-order modeling using proper orthogonal decomposition is thoroughly investigated not only for the velocity field but also for higher order flow characteristics such as time average wall shear stress, oscillatory shear index and viscous energy dissipation.
Conclusion
Considering these results, proper orthogonal decomposition can provide a rapid binary classifier to evaluate if the bileaflet mechanical valve deviates from its normal operating conditions. Moreover, the study shows that the size of the reduced-order model depends on which flow parameter is required to be reconstructed.







Similar content being viewed by others
References
Aubry, N., R. Guyonnet, and R. Lima. Spatiotemporal analysis of complex signals: theory and applications. J. Stat. Phys. 64:683–739, 1991. https://doi.org/10.1007/BF01048312.
Bagur, R., P. Pibarot, and C. M. Otto. Importance of the valve durability-life expectancy ratio in selection of a prosthetic aortic valve. Heart 103:1756–1759, 2017. https://doi.org/10.1136/heartjnl-2017-312348.
Ballarin, F., E. Faggiano, S. Ippolito, A. Manzoni, A. Quarteroni, G. Rozza, et al. Fast simulations of patient-specific haemodynamics of coronary artery bypass grafts based on a POD-Galerkin method and a vascular shape parametrization. J. Comput. Phys. 315:609–628, 2016. https://doi.org/10.1016/j.jcp.2016.03.065.
Berkooz, G., P. Holmes, and J. L. Lumley. The proper orthogonal decomposition in the analysis of turbulent flows. Annu. Rev. Fluid Mech. 25:539–575, 1993. https://doi.org/10.1146/annurev.fl.25.010193.002543.
Borazjani, I., and F. Sotiropoulos. The effect of implantation orientation of a bileaflet mechanical heart valve on kinematics and hemodynamics in an anatomic aorta. J. Biomech. Eng. 132:111005, 2010. https://doi.org/10.1115/1.4002491.
Boulakia, M., E. Schenone, and J. F. Gerbeau. Reduced-order modeling for cardiac electrophysiology application to parameter identification. Int J Numer Method Biomed Eng 28:727–744, 2012. https://doi.org/10.1002/cnm.
Byrne, G., F. Mut, and J. Cebral. Quantifying the large-scale hemodynamics of intracranial aneurysms. Am J Neuroradiol 35:333–338, 2014. https://doi.org/10.3174/ajnr.A3678.
Caiazzo, A., R. Guibert, and I. E. Vignon-Clementel. A reduced-order modeling for efficient design study of artificial valve in enlarged ventricular outflow tracts. Comput Methods Biomech Biomed Engin 19:1314–1318, 2016. https://doi.org/10.1080/10255842.2015.1133811.
Carnecky, R., T. Brunner, S. Born, J. Waser, C. Heine, and R. Peikert. Vortex detection in 4D MRI data: using the proper orthogonal decomposition for improved noise-robustness. Eurographics Conf Vis 33:281–290, 2014.
Cenedese, A., Z. Del Prete, M. Miozzi, and G. Querzoli. A laboratory investigation of the flow in the left ventricle of a human heart with prosthetic. Tilting-Disk Valves. Exp Fluids 39:322–335, 2005. https://doi.org/10.1007/s00348-005-1006-4.
Chang, G. H., C. M. Schirmer, and Y. Modarres-Sadeghi. A reduced-order model for wall shear stress in abdominal aortic aneurysms by proper orthogonal decomposition. J. Biomech. 54:33–43, 2017. https://doi.org/10.1016/j.jbiomech.2017.01.035.
Charonko, J. J., R. Kumar, K. Stewart, W. C. Little, and P. P. Vlachos. Vortices formed on the mitral valve tips aid normal left ventricular filling. Ann. Biomed. Eng. 41:1049–1061, 2013. https://doi.org/10.1007/s10439-013-0755-0.
Chaudhary, R., J. Garg, P. Krishnamoorthy, N. Shah, B. A. Feldman, M. W. Martinez, et al. On-X valve: the next generation aortic valve. Cardiol Rev 25:77–83, 2017. https://doi.org/10.1097/CRD.0000000000000105.
Dangas, G. D., J. I. Weitz, G. Giustino, R. Makkar, and R. Mehran. Prosthetic heart valve thrombosis. J. Am. Coll. Cardiol. 68:2670–2689, 2016. https://doi.org/10.1016/j.jacc.2016.09.958.
Darwish, A., G. Di Labbio, W. Saleh, and L. Kadem. In vitro characterization of lagrangian fluid transport downstream of a dysfunctional bileaflet mechanical aortic valve. AIP Adv. 10:095319, 2020. https://doi.org/10.1063/5.0021372.
Darwish, A., G. Di Labbio, W. Saleh, O. Smadi, and L. Kadem. Experimental investigation of the flow downstream of a dysfunctional bileaflet mechanical aortic valve. Artif. Organs 43:1–15, 2019. https://doi.org/10.1111/aor.13483.
Dasi, L. P., H. A. Simon, P. Sucosky, and A. P. Yoganathan. Fluid mechanics of artificial heart valves. Clin. Exp. Pharmacol. Physiol. 36:225–237, 2009. https://doi.org/10.1111/j.1440-1681.2008.05099.x.
Di Labbio, G., and L. Kadem. Jet collisions and vortex reversal in the human left ventricle. J. Biomech. 78:155–160, 2018. https://doi.org/10.1016/j.jbiomech.2018.07.023.
Di Labbio, G., and L. Kadem. Reduced-order modeling of left ventricular flow subject to aortic valve regurgitation. Phys. Fluids 31:31901, 2019. https://doi.org/10.1063/1.5083054.
Farag, E. S., L. Peroni, L. M. Gottwald, J. Vendrik, S. M. Boekholdt, A. J. Nederveen, et al. Bileaflet mechanical aortic valve prosthesis orientation influences ascending aortic blood flow patterns. Struct Hear 3:12, 2019. https://doi.org/10.1080/24748706.2019.1587948.
Fishbein, G. A., and M. C. Fishbein. Pathology of the aortic valve: aortic valve stenosis/aortic regurgitation. Curr Cardiol Rep 2019. https://doi.org/10.1007/s11886-019-1162-4.
Ge, L., L. P. Dasi, F. Sotiropoulos, and A. P. Yoganathan. Characterization of hemodynamic forces induced by mechanical heart valves: reynolds vs. viscous stresses. Ann. Biomed. Eng. 36:276–297, 2008. https://doi.org/10.1007/s10439-007-9411-x.
Grinberg, L., A. Yakhot, and G. E. Karniadakis. Analyzing transient turbulence in a stenosed carotid artery by proper orthogonal decomposition. Ann. Biomed. Eng. 37:2200–2217, 2009. https://doi.org/10.1007/s10439-009-9769-z.
Guibert, R., K. McLeod, A. Caiazzo, T. Mansi, M. A. Fernández, M. Sermesant, et al. Group-wise construction of reduced models for understanding and characterization of pulmonary blood flows from medical images. Med. Image Anal. 18:63–82, 2014. https://doi.org/10.1016/j.media.2013.09.003.
Gürsoy, M. O., M. Kalcik, M. Yesin, S. Karakoyun, E. Bayam, S. Gündüz, et al. A global perspective on mechanical prosthetic heart valve thrombosis: diagnostic and therapeutic challenges. Anatol J Cardiol 2016. https://doi.org/10.14744/AnatolJCardiol.2016.7486.
Ha, H., H. J. Koo, H. K. Huh, G. B. Kim, J. Kweon, N. Kim, et al. Effect of Pannus formation on the prosthetic heart valve. In vitro demonstration using particle image velocimetry. PLoS ONE 13:1–19, 2018. https://doi.org/10.1371/journal.pone.0199792.
Habets, J., R. P. Budde, P. Symersky, R. B. van den Brink, B. A. de Mol, W. P. Mali, et al. Diagnostic evaluation of left-sided prosthetic heart valve dysfunction. Nat Rev Cardiol 8:466–478, 2011. https://doi.org/10.1038/nrcardio.2011.71.
Haya, L., and S. Tavoularis. Effects of bileaflet mechanical heart valve orientation on fluid ftresses and coronary flow. J. Fluid Mech. 806:129–164, 2016. https://doi.org/10.1017/jfm.2016.582.
Huang, G., H. V. Schaff, T. M. Sundt, and S. H. Rahimtoola. Treatment of obstructive thrombosed prosthetic heart valve. J. Am. Coll. Cardiol. 62:1731–1736, 2013. https://doi.org/10.1016/j.jacc.2013.07.075.
Janiga, G. Computerized Medical Imaging and Graphics Novel feature-based visualization of the unsteady blood flow in intracranial aneurysms with the help of proper orthogonal decomposition (POD). Comput. Med. Imaging Graph. 73:30–38, 2019. https://doi.org/10.1016/j.compmedimag.2019.01.001.
Janiga, G. Quantitative assessment of 4D hemodynamics in cerebral aneurysms using proper orthogonal decomposition. J. Biomech. 82:80–86, 2019. https://doi.org/10.1016/j.jbiomech.2018.10.014.
Kefayati, S., and T. L. Poepping. Transitional flow analysis in the carotid artery bifurcation by proper orthogonal decomposition and particle image velocimetry. Med. Eng. Phys. 35:898–909, 2013. https://doi.org/10.1016/j.medengphy.2012.08.020.
Khalili, F., P. P. T. Gamage, R. H. Sandler, and H. A. Mansy. Adverse hemodynamic conditions associated with mechanical heart valve leaflet immobility. Bioengineering 5:74, 2018. https://doi.org/10.3390/bioengineering5030074.
Kheradvar, A., E. M. Groves, C. J. Goergen, S. H. Alavi, R. Tranquillo, C. A. Simmons, et al. Emerging trends in heart valve engineering: Part II. Novel and standard technologies for aortic valve replacement. Ann. Biomed. Eng. 43:844–857, 2015. https://doi.org/10.1007/s10439-014-1191-5.
Lucia, D. J., P. S. Beran, and W. A. Silva. Reduced-order modeling: new approaches for computational physics. Prog. Aerosp. Sci. 40:51–117, 2004. https://doi.org/10.1016/j.paerosci.2003.12.001.
Lumley JL. The structure of inhomogeneous turbulent flows. Atmospheric turbulence and radio wave propagation. 1967:166–76.
Ma, W.-G., B. Hou, A. Abdurusul, D.-X. Gong, Y. Tang, Q. Chang, et al. Dysfunction of mechanical heart valve prosthesis: experience with surgical management in 48 patients. J Thorac Dis 7:2321–2329, 2015. https://doi.org/10.3978/j.issn.2072-1439.2015.12.25.
Mcgregor, R. H. P., D. Szczerba, M. Von Siebenthal, K. Muralidhar, and G. Székely. Exploring the use of proper orthogonal decomposition for enhancing blood flow images via computational fluid dynamics. Med Image Comput Comput Interv MICCAI 2008. https://doi.org/10.1007/978-3-540-85990-1_94.
McLeod, K., A. Caiazzo, M. A. Fernandez, T. Mansi, I. E. Vignon-Clementel, M. Sermesant, et al. Atlas-based reduced models of blood flows for fast patient-specific simulations. Lect. Notes Comput. Sci. 6364:95–104, 2010.
Montorsi, P., F. De Bernardi, M. Muratori, D. Cavoretto, and M. Pepi. Role of cine-fluoroscopy, transthoracic, and transesophageal echocardiography in patients with suspected prosthetic heart valve thrombosis. Am. J. Cardiol. 85:58–64, 2000. https://doi.org/10.1016/S0002-9149(99)00607-4.
Morbiducci, U., R. Ponzini, M. Nobili, D. Massai, F. M. Montevecchi, D. Bluestein, et al. Blood damage safety of prosthetic heart valves. Shear-induced platelet activation and local flow dynamics: a fluid-structure interaction approach. J. Biomech. 42:1952–1960, 2009. https://doi.org/10.1016/j.jbiomech.2009.05.014.
Noack, B. R. From snapshots to modal expansions-bridging low residuals and pure frequencies. J. Fluid Mech. 802:1–4, 2016. https://doi.org/10.1017/jfm.2016.416.
Ostrowski, S., A. Marcinkiewicz, A. Kosmider, A. Walczak, R. Zwolinski, and R. Jaszewski. Artificial aortic valve dysfunction due to pannus and thrombus—different methods of cardiac surgical management. Card Surg 12:199–203, 2015. https://doi.org/10.5114/kitp.2015.54453.
Pagani, S., A. Manzoni, and A. Quarteroni. Numerical approximation of parametrized problems in cardiac electrophysiology by a local reduced basis method. Comput Methods Appl Mech Engrg 340:530–558, 2018. https://doi.org/10.1016/j.cma.2018.06.003.
Papolla, C., A. Darwish, L. Kadem, and R. Rieu. Impact of mitral regurgitation on the flow in a model of a left ventricle. Cardiovasc Eng Technol 2020. https://doi.org/10.1007/s13239-020-00490-y.
Raffel, M., C. E. Willert, S. T. Wereley, and J. Kompenhans. Particle Image Velocimetry, Vol. 79. Berlin: Springer, 2007.
Raghav, V., S. Sastry, and N. Saikrishnan. Experimental assessment of flow fields associated with heart valve prostheses using particle image velocimetry (PIV): recommendations for best practices. Cardiovasc Eng Technol 9:273–287, 2018. https://doi.org/10.1007/s13239-018-0348-z.
Rehimi, F., and F. Aloui. Synchronized analysis of an unsteady laminar flow downstream of a circular cylinder centred between two parallel walls using PIV and mass transfer probes. Exp. Fluids 51:1–22, 2011. https://doi.org/10.1007/s00348-010-1005-y.
Rimmer, L., M. U. Ahmad, G. Chaplin, M. Joshi, and A. Harky. Aortic valve repair: where are we now? Hear Lung Circ 28:988–999, 2019. https://doi.org/10.1016/j.hlc.2019.02.007.
Roudaut, R., K. Serri, and S. Lafitte. Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations. Heart 93:137–142, 2007. https://doi.org/10.1136/hrt.2005.071183.
Shahriari, S., H. Maleki, I. Hassan, and L. Kadem. Evaluation of shear stress accumulation on blood components in normal and dysfunctional bileaflet mechanical heart valves using smoothed particle hydrodynamics. J. Biomech. 2012. https://doi.org/10.1016/j.jbiomech.2012.08.009.
Shi, J., Z. Bai, J. Hu, B. Zhang, and Y. Guo. Rare early prosthesis obstruction after mitral valve replacement: a case report and literature review. J Cardiothorac Surg 7:64, 2012. https://doi.org/10.1186/1749-8090-7-64.
Sirovich, L. Turbulence and the dynamics of coherent structures Part I: Coherent structures. Q. Appl. Math. 45:573–582, 1987. https://doi.org/10.1090/qam/910463.
Sirovich, L., and M. Kirby. Low-dimensional procedure for the characterization of human faces. J. Opt. Soc. Am. A 4:519, 1987. https://doi.org/10.1364/josaa.4.000519.
Smadi, O., J. Garcia, P. Pibarot, E. Gaillard, I. Hassan, and L. Kadem. Accuracy of doppler-echocardiographic parameters for the detection of aortic bileaflet mechanical prosthetic valve dysfunction. Eur Heart J Cardiovasc Imaging 15:142–151, 2014. https://doi.org/10.1093/ehjci/jet059.
Smadi, O., I. Hassan, P. Pibarot, and L. Kadem. Numerical and experimental investigations of pulsatile blood flow pattern through a dysfunctional mechanical heart valve. J. Biomech. 43:1565–1572, 2010. https://doi.org/10.1016/j.jbiomech.2010.01.029.
Teshima, H., N. Hayashida, S. Fukunaga, E. Tayama, T. Kawara, S. Aoyagi, et al. Usefulness of a multidetector-row computed tomography scanner for detecting pannus formation. Ann. Thorac. Surg. 77:523–526, 2004. https://doi.org/10.1016/S0003-4975(03)01531-5.
Teshima, H., N. Hayashida, H. Yano, M. Nishimi, E. Tayama, S. Fukunaga, et al. Obstruction of St Jude medical valves in the aortic position: histology and immunohistochemistry of pannus. J. Thorac. Cardiovasc. Surg. 126:401–407, 2003. https://doi.org/10.1016/S0022-5223(03)00702-5.
Vennemann, B. M., T. Rösgen, T. P. Carrel, and D. Obrist. Time-resolved micro PIV in the pivoting area of the triflo mechanical heart valve. Cardiovasc Eng Technol 7:210–222, 2016. https://doi.org/10.1007/s13239-016-0264-z.
Xu, R., M. Rahnavardi, B. Pitman, M. Shirazi, R. Stuklis, J. Edwards, et al. On-X versus St Jude Medical Regent mechanical aortic valve prostheses: early haemodynamics. Open Hear. 2017. https://doi.org/10.1136/openhrt-2016-000539.
Yakhot, A., T. Anor, and G. E. Karniadakis. A reconstruction method for gappy and noisy arterial flow data. IEEE Trans. Med. Imaging 26:1681–1697, 2007. https://doi.org/10.1109/TMI.2007.901991.
Yoganathan, A. P., K. B. Chandran, and F. Sotiropoulos. Flow in prosthetic heart valves: state-of-the-art and future directions. Ann. Biomed. Eng. 33:1689–1694, 2005. https://doi.org/10.1007/s10439-005-8759-z.
Acknowledgements
This work is supported by a grant from the Natural Sciences and Engineering Research Council of Canada (NSERC)
Conflict of interest
Ahmed Darwish, Giuseppe Di Labbio, Wael Saleh and Lyes Kadem declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Keefe B. Manning oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material. A guide to use the POD data is provided along with entropy values and POD modes for all investigated cases. The same document includes static figures showing the matching flow features between the original flow and the reconstructed flows. Moreover, a table showing the opening and closure times of the valve leaflets for all cases is included in this supplementary document. Finally, six videos (for all cases) are provided showing three panels with the original flow in the left panel, the reconstructed flow using the first 2 modes in the middle panel and the reconstructed flow using the first 10 modes in the right panel.
Supplementary material 1 (MP4 9881 kb)
Supplementary material 2 (MP4 9317 kb)
Supplementary material 3 (MP4 8102 kb)
Supplementary material 4 (MP4 9568 kb)
Supplementary material 5 (MP4 9798 kb)
Supplementary material 6 (MP4 9734 kb)
Rights and permissions
About this article
Cite this article
Darwish, A., Di Labbio, G., Saleh, W. et al. Proper Orthogonal Decomposition Analysis of the Flow Downstream of a Dysfunctional Bileaflet Mechanical Aortic Valve. Cardiovasc Eng Tech 12, 286–299 (2021). https://doi.org/10.1007/s13239-021-00519-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00519-w