Abstract
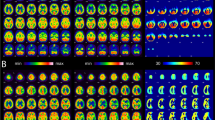
More than 60% of moyamoya disease (MMD) patients suffers cerebral ischemia and preoperative cerebral infarction (CI) increases the risk of postoperative stroke and unfavorable outcome. We established a nomogram system for risk stratification of CI to help tailoring individualized management. We enrolled 380 patients including 680 hemispheres for the training cohort from our hospital and 183 patients including 348 hemispheres for the validation cohort from multicenter. A nomogram for CI was formulated based on the multivariable logistic regression analysis. The predictive accuracy and discriminative ability of nomogram were determined with concordance index (C-index) and calibration curve. For the training cohort, 246 hemispheres (36.2%) were found with CI. In multivariable logistic regression used generalized estimating equations approach, anterior choroidal artery (AchA) grade (grade 1, OR 0.214, 95%CI 0.124–0.372, P < 0.001; grade 2, OR 0.132, 95%CI 0.066–0.265, P < 0.001), cerebral perfusion (OR 4.796, 95%CI 2.922–7.872; P < 0.001), white matter hyperintensity (OR 3.652, 95%CI 1.933–6.902; P < 0.001), brush sign (OR 3.555, 95%CI 2.282–5.538; P < 0.001), and ivy sign (equivocal, OR 4.752, 95%CI 2.788–8.099, P < 0.001; present, OR 8.940, 95%CI 4.942–16.173, P < 0.001) were significant factors for CI. The C-index of the nomogram for predicting cerebral infarction was 0.890 (95%CI 0.866–0.915) in the training cohort and 0.847 (95%CI 0.805–0.889) in the validation cohort. The nomogram composed of AchA grade, cerebral perfusion, white matter hyperintensity, brush sign, and ivy sign could provide risk stratification of CI before surgery in patients with MMD. Active treatment might be recommended before CI, which could reduce the risk of stroke after surgery.


Similar content being viewed by others
Data Availability
Data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis ea. Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurologia Medico-Chirurgica. 2012;52(5):245–66. https://doi.org/10.2176/nmc.52.245.
Cho WS, Chung YS, Kim JE, Jeon JP, Son YJ, Bang JS, Kang HS, Sohn CH, Oh CW. The natural clinical course of hemodynamically stable adult moyamoya disease. J Neurosurg. 2015;122(1):82–9. https://doi.org/10.3171/2014.9.Jns132281.
Kraemer M, Heienbrok W, Berlit P. Moyamoya disease in Europeans. Stroke. 2008;39(12):3193–200. https://doi.org/10.1161/strokeaha.107.513408.
Jeon JP, Kim JE, Cho WS, Bang JS, Son YJ, Oh CW. Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg. 2018;128(3):793–9. https://doi.org/10.3171/2016.11.Jns161688.
Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, Nakagawara J, Takahashi JC. Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan adult moyamoya trial. Stroke. 2014;45(5):1415–21. https://doi.org/10.1161/strokeaha.113.004386.
Chen Y, Ma L, Yang S, Burkhardt JK, Lu J, Ye X, Jiang W, Ren Z, Wang R, Chen X, Zhao Y. Quantitative angiographic hemodynamic evaluation after revascularization surgery for moyamoya disease. Transl Stroke Res. 2020;11(5):871–81. https://doi.org/10.1007/s12975-020-00781-5.
Kazumata K, Ito M, Tokairin K, Ito Y, Houkin K, Nakayama N, Kuroda S, Ishikawa T, Kamiyama H. The frequency of postoperative stroke in moyamoya disease following combined revascularization: a single-university series and systematic review. J Neurosurg. 2014;121(2):432–40. https://doi.org/10.3171/2014.1.Jns13946.
Kuroda S, Kashiwazaki D, Hirata K, Shiga T, Houkin K, Tamaki N. Effects of surgical revascularization on cerebral oxygen metabolism in patients with moyamoya disease: an 15O-gas positron emission tomographic study. Stroke. 2014;45(9):2717–21. https://doi.org/10.1161/strokeaha.114.006009.
Yu L, Ma L, Huang Z, Shi Z, Wang R, Zhao Y, Zhang D. Revascularization surgery in patients with ischemic-type moyamoya disease: predictors for postoperative stroke and long-term outcomes. World Neurosurg. 2019;128:e582–96. https://doi.org/10.1016/j.wneu.2019.04.214.
Deng X, Gao F, Zhang D, Zhang Y, Wang R, Wang S, Cao Y, Zhao Y, Pan Y, Ye X, Liu X, Zhang Q, Wang J, Yang Z, Zhao M, Zhao J. Effects of different surgical modalities on the clinical outcome of patients with moyamoya disease: a prospective cohort study. J Neurosurg. 2018;128(5):1327–37. https://doi.org/10.3171/2016.12.Jns162626.
Suzuki J, Takaku A. Cerebrovascular, “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20(3):288–99. https://doi.org/10.1001/archneur.1969.00480090076012.
Morioka M, Hamada J, Kawano T, Todaka T, Yano S, Kai Y, Ushio Y. Angiographic dilatation and branch extension of the anterior choroidal and posterior communicating arteries are predictors of hemorrhage in adult moyamoya patients. Stroke. 2003;34(1):90–5. https://doi.org/10.1161/01.str.0000047120.67507.0d.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR Signal abnormalities at 15 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6. https://doi.org/10.2214/ajr.149.2.351.
Horie N, Morikawa M, Nozaki A, Hayashi K, Suyama K, Nagata I. “Brush Sign” on susceptibility-weighted MR imaging indicates the severity of moyamoya disease. AJNR Am J Neuroradiol. 2011;32(9):1697–702. https://doi.org/10.3174/ajnr.A2568.
Lu J, Zhao Y, Li M, Ma L, Chen Y, Wang R, Ye X, Wang H, Chen X, Zhao Y. Clinical implications of the “brush sign” in susceptibility-weighted imaging for moyamoya disease. Cerebrovasc Dis (Basel Switzerland). 2021;50(2):147–55. https://doi.org/10.1159/000511936.
Yoon HK, Shin HJ, Chang YW. "Ivy sign" in childhood moyamoya disease: depiction on FLAIR and contrast-enhanced T1-weighted MR images. Radiology. 2002;223(2):384–9.https://doi.org/10.1148/radiol.2232011094
Yin H, Liu X, Zhang D, Zhang Y, Wang R, Zhao M, Zhao J. A novel staging system to evaluate cerebral hypoperfusion in patients with moyamoya disease. Stroke. 2018;49(12):2837–43. https://doi.org/10.1161/strokeaha.118.022628.
Jang DK, Lee KS, Rha HK, Huh PW, Yang JH, Park IS, Ahn JG, Sung JH, Han YM. Bypass surgery versus medical treatment for symptomatic moyamoya disease in adults. J Neurosurg. 2017;127(3):492–502. https://doi.org/10.3171/2016.8.Jns152875.
Ha EJ, Kim KH, Wang KC, Phi JH, Lee JY, Choi JW, Cho BK, Yang J, Byun YH, Kim SK. Long-term outcomes of indirect bypass for 629 children with moyamoya disease: longitudinal and cross-sectional analysis. Stroke. 2019;50(11):3177–83. https://doi.org/10.1161/strokeaha.119.025609.
Nielsen TH, Abhinav K, Sussman ES, Han SS, Weng Y, Bell-Stephens T, Heit JJ, Steinberg GK. Direct versus indirect bypass procedure for the treatment of ischemic moyamoya disease: results of an individualized selection strategy. J Neurosurg. 2020;134(5):1578–89. https://doi.org/10.3171/2020.3.Jns192847.
Chen J, Duan L, Xu WH, Han YQ, Cui LY, Gao S. Microembolic signals predict cerebral ischaemic events in patients with moyamoya disease. European J Neurol. 2014;21(5):785–90. https://doi.org/10.1111/ene.12392.
Kim SK, Cho BK, Phi JH, Lee JY, Chae JH, Kim KJ, Hwang YS, Kim IO, Lee DS, Lee J, Wang KC. Pediatric moyamoya disease: an analysis of 410 consecutive cases. Ann Neurol. 2010;68(1):92–101. https://doi.org/10.1002/ana.21981.
Funaki T, Takahashi JC, Houkin K, Kuroda S, Takeuchi S, Fujimura M, Tomata Y, Miyamoto S. High rebleeding risk associated with choroidal collateral vessels in hemorrhagic moyamoya disease: analysis of a nonsurgical cohort in the Japan Adult Moyamoya Trial. J Neurosurg. 2019;130(2):337–673. https://doi.org/10.3171/2017.9.Jns17576.
Jiang H, Ni W, Xu B, Lei Y, Tian Y, Xu F, Gu Y, Mao Y. Outcome in adult patients with hemorrhagic moyamoya disease after combined extracranial-intracranial bypass. J Neurosurg. 2014;121(5):1048–55. https://doi.org/10.3171/2014.7.Jns132434.
Pantoni L, Garcia JH. Pathogenesis of leukoaraiosis: a review. Stroke. 1997;28(3):652–9. https://doi.org/10.1161/01.str.28.3.652.
van Swieten JC, van den Hout JH, van Ketel BA, Hijdra A, Wokke JH, van Gijn J. Periventricular lesions in the white matter on magnetic resonance imaging in the elderly. A morphometric correlation with arteriolosclerosis and dilated perivascular spaces. Brain : J Neurol. 1991;114(Pt 2):761–74. https://doi.org/10.1093/brain/114.2.761.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ (Clin Res ed). 2010;341:c3666. https://doi.org/10.1136/bmj.c3666.
Akhtar N, Salam A, Kamran S, D’Souza A, Imam Y, Bermejo PG, Wadiwala MF, Own A, ElSotouhy A, Vattoth S, Bourke P, Bhutta Z, Joseph S, Santos M, Khan RA, Shuaib A. Pre-existing small vessel disease in patients with acute stroke from the Middle East, Southeast Asia, and Philippines. Transl Stroke Res. 2018;9(3):274–82. https://doi.org/10.1007/s12975-017-0578-7.
Bang OY, Chung JW, Kim DH, Won HH, Yeon JY, Ki CS, Shin HJ, Kim JS, Hong SC, Kim DK, Koizumi A. Moyamoya disease and spectrums of RNF213 vasculopathy. Transl Stroke Res. 2020;11(4):580–9. https://doi.org/10.1007/s12975-019-00743-6.
Li SJ, Xiong J, He Y, Xiao YY, Mao DA, Liu LQ. A rare case of pediatric moyamoya disease with reversible white matter lesions in a 3-year-old Chinese girl. Child’s Nerv Syst. 2020;36(1):197–201. https://doi.org/10.1007/s00381-019-04391-x.
Komatsu K, Mikami T, Noshiro S, Miyata K, Wanibuchi M, Mikuni N. Reversibility of white matter hyperintensity by revascularization surgery in Moyamoya disease. J Stroke Cerebrovasc Dis. 2016;25(6):1495–502. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.02.035.
Sun H, Li W, Xia C, Ren Y, Ma L, Xiao A, You C, Wang X, Tian R, Liu Y. Magnetic resonance imaging markers of cerebral small vessel disease in adults with Moyamoya disease. Transl Stroke Res. 2022;13(4):533–42. https://doi.org/10.1007/s12975-021-00973-7
Ohta T, Tanaka H, Kuroiwa T. Diffuse leptomeningeal enhancement, “ivy sign,” in magnetic resonance images of moyamoya disease in childhood: case report. Neurosurgery. 1995;37(5):1009–12. https://doi.org/10.1227/00006123-199511000-00024.
Kawashima M, Noguchi T, Takase Y, Ootsuka T, Kido N, Matsushima T. Unilateral hemispheric proliferation of ivy sign on fluid-attenuated inversion recovery images in moyamoya disease correlates highly with ipsilateral hemispheric decrease of cerebrovascular reserve. AJNR Am J Neuroradiol. 2009;30(9):1709–16. https://doi.org/10.3174/ajnr.A1679.
Kaku Y, Iihara K, Nakajima N, Kataoka H, Fukushima K, Iida H, Hashimoto N. The leptomeningeal ivy sign on fluid-attenuated inversion recovery images in moyamoya disease: positron emission tomography study. Cerebrovasc Dis (Basel Switzerland). 2013;36(1):19–25. https://doi.org/10.1159/000351143.
Acknowledgements
The authors thank Pro.Aizhong Liu, who is professor of the department of Epidemiology and Health Statistics, Xiangya School of Public Health, Central South University, for providing some advices on statistical analysis.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82001274 to Dr. Huang) and the Natural Science Foundation of Hunan Province of China (Grant No. 2021JJ40994 to Dr. Huang).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board of Xiangya Hospital.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, P., Wang, Y., Li, S. et al. Development and External Validation of Nomogram for Cerebral Infarction in Moyamoya Diseases. Transl. Stroke Res. 14, 890–898 (2023). https://doi.org/10.1007/s12975-023-01127-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-023-01127-7