Abstract
This narrative review summarizes the current knowledge on point-of-care ultrasound (POCUS) of gastric contents in order to inform an assessment of aspiration risk and guide anesthetic management at the bedside. An I-AIM framework (Indication, Acquisition, Interpretation, and Medical decision-making) is used to summarize and organize the content areas. This narrative review spans the breadth of the literature on pediatric and adult subjects as well as on special patient populations such as obstetric and severely obese individuals. Areas that need further investigation include the diagnostic accuracy of gastric POCUS from a Bayesian perspective and the impact of POCUS on patient outcomes, healthcare economics, and educational curricula.
Résumé
Ce compte rendu narratif résume les connaissances actuelles concernant l’échographie au chevet (POCUS) du contenu gastrique afin de raffiner l’évaluation du risque d’aspiration et de guider la prise en charge anesthésique au chevet. Un cadre dit I-AIM (Indication, Acquisition, Interprétation, et prise de décision Médicale) est utilisé pour résumer et organiser les domaines de contenu. Ce compte rendu narratif a revu la littérature sur les sujets pédiatriques et adultes ainsi que celle portant sur des populations spéciales, telles que les patientes en obstétrique et les patients obèses morbides. Parmi les domaines qui bénéficieraient de recherches approfondies, citons la précision diagnostique de l’échographie gastrique au chevet d’un point de vue bayésien et l’impact de ce type d’échographie sur les pronostics de patients, l’économie des soins de santé, et les programmes de formation.
Similar content being viewed by others
The purpose of this narrative review is to summarize the current knowledge on gastric point-of-care ultrasound (POCUS). The subject matter is geared towards an international audience with the goal to raise interest in POCUS and to provide a basic set of reference materials for use in the preparation for a “hands on” training course.
Methods
A broad literature search was performed on the MEDLINE® database from inception to May 1, 2017, including the MeSH terms stomach, ultrasonography, pneumonia, and aspiration, and combined with AND. Two authors reviewed and selected the abstracts by consensus according to relevance. The new information from the full-text articles was summarized and presented according to an I-AIM framework (Indications, Acquisition, Interpretation, and Medical decision-making).
Rationale for use
Pulmonary aspiration of gastric contents carries significant morbidity and mortality.1,2,3 Aspiration is the leading cause of death from anesthesia airway events,4 and major morbidity (including pneumonitis, acute respiratory distress syndrome, multiple organ dysfunction, and brain damage) is common among survivors.5 Inaccurate risk assessment is often a root cause of aspiration events.4 While a “full stomach” is a major risk factor for aspiration under anesthesia, the lack of an objective tool to assess gastric content at the bedside limits risk assessment, and patient management is usually based on patient history alone. Although the risk of aspiration is highest in emergency situations, it occasionally occurs in patients who have followed fasting guidelines and are considered at low risk.2 This baseline risk is approximately 1:4,000.2
Gastric ultrasound is an emerging point-of-care tool that provides bedside information on gastric content and volume.6,7,8 Similar to other more established POCUS applications, such as cardiac or lung assessment, this diagnostic modality is used to answer a well-defined clinical question in a short period of time in order to guide patient management and ultimately improve patient outcome.9 In the case of gastric ultrasound, this is typically a dichotomous question. Is the patient’s stomach “empty” or “full”? While the definition of a “full” stomach is controversial and conceivably open to interpretation, an acceptable working definition denotes any gastric content beyond what is normal for healthy fasted subjects (i.e., any solid or thick particulate content or clear fluid in excess of baseline gastric secretions of > 1.5 mL·kg−1)10,11 Gastric ultrasound has been studied in pregnant and non-pregnant adults, severely obese subjects, elective and non-elective situations, and pediatric patients. Several recent editorials in major anesthesiology journals have called for greater adoption and teaching of gastric POCUS in anesthesia practice.12,13,14 Benhamou suggested that this skill should be part of the basic armamentarium of anesthesiologists for daily practice.12 Mahmood et al. reported a POCUS curriculum for anesthesiologists that includes gastric ultrasound along with other more established applications such as lung and cardiac assessment.13 Finally, Lucas et al. suggested that the three most useful emerging ultrasound applications in obstetric anesthesia practice are a) ultrasound of the spine prior to neuraxial anesthesia, b) ultrasound for airway assessment, and c) gastric ultrasound.14
All POCUS applications are ultimately diagnostic tests. Although they are brief and focused, each needs to be studied from multiple angles. It is essential to determine their diagnostic validity (i.e., do they evaluate what needs to be evaluated?) and to establish their reliability and diagnostic accuracy. Diagnostic accuracy refers to the global accuracy (the percentage of exams with a “correct diagnosis”) as well as the sensitivity, specificity, and positive and negative predictive values. Given the importance of correctly ruling out a full stomach to prevent aspiration, the negative predictive value of the test is arguably of outmost importance. Other aspects of relevance that need further study include the clinical applicability, educational aspects, and cost-effectiveness of POCUS. As an emerging diagnostic tool, some (but not all) of these aspects of the test have been studied for gastric ultrasound, and there is much room for development and change.
Clinical scenario
-
History of present illness: A 79-yr-old male presents for an internal fixation of a closed femoral shaft fracture that occurred 24 hr ago. The surgical procedure is relatively urgent but not immediately life-threatening. The timing of the last meal is unclear. While the patient’s daughter states he has remained nil per os, the patient insists he had a full lunch three hours ago.
-
Medical history: The patient has hemodynamically significant severe aortic stenosis with a valve area of 0.8 cm2 with recent episodes of exertional syncope. He has severe left ventricular hypertrophy with diastolic dysfunction but preserved systolic function. He also had an episode of transient ischemic attack within the past year. He has mild carotid stenosis for which he is on antiplatelet therapy. His medications include metoprolol 25 mg twice daily, clopidogrel 75 mg daily, and atorvastatin 20 mg daily, and he received 5 mg of morphine iv one hour ago.
-
Physical examination: He is oriented to self, place, and year but unsure of the month or exact day. He has a body mass index (BMI) of 38 kg·m−2 and the upper airway looks normal. He is currently hemodynamically stable. An electrocardiogram shows signs of left ventricular hypertrophy but is otherwise unremarkable, and routine blood work is within normal limits.
-
Anesthetic plan: The first decision is whether to proceed with semi-urgent surgery in a subject with questionable nil per os status. The second decision pertains to the most appropriate anesthetic technique, which may impact the higher-order decision whether to proceed. Given the contraindications for a neuraxial technique (severe aortic stenosis and current antiplatelet therapy) a general anesthetic is planned. The clinical conflict here is between a) a “full stomach”, which would dictate a rapid sequence induction of anesthesia but pose a higher risk of hemodynamic instability and acute cardiac events, and b) a slowly titrated induction of anesthesia, which would be indicated for his severe aortic stenosis but possibly increase the risk of aspiration in the setting of a “full stomach”.
The I-AIM framework
An I-AIM framework is a suitable paradigm for using and teaching gastric ultrasound.15 When gastric content is unknown or uncertain based on clinical information (Indication), ultrasound images are acquired in a standardized manner (Acquisition). Once an adequate image is obtained, it is interpreted based on qualitative and quantitative findings (Interpretation). This interpretation of the findings is then used to guide airway or anesthetic management (Medical decision-making). This framework succinctly describes the main conceptual steps for the clinical use of any point-of-care diagnostic ultrasound application and is used in this review.11
Indication
A gastric ultrasound exam is indicated to assess individual risk of aspiration in the setting of unclear or undetermined nil per os status. Similar to other tests with dichotomous results (yes or no; full or empty) and following a Bayesian diagnostic framework, gastric ultrasound is likely most useful when there is true clinical uncertainty, i.e., when the pre-test probability of having a full stomach is in the order of 50%.11,16 Such common clinical scenarios include a) uncertain or contradictory information regarding nil per os status (e.g., due to a language barrier or decreased level of consciousness) and b) medical comorbidities or physiologic conditions that may prolong gastric emptying despite adequate fasting (e.g., diabetic gastroparesis, achalasia, advanced renal or hepatic dysfunction, critical illness, multiple sclerosis, Parkinson’s disease, substance abuse, recent trauma, and labour).10,17 Another interesting group of patients are those presenting for non-elective procedures who may not have had an opportunity to fast or may have delayed gastric emptying related to pain, sympathetic activation, or recent opioid therapy. Bouvet et al. reported a prevalence of full stomach in 56% of emergency surgical patients and suggested that a preoperative ultrasound assessment of gastric content may be particularly useful in this setting.17 The routine application of gastric POCUS in patients with a low pre-test probability of a full stomach (i.e., fasted subjects for elective surgery) is somewhat controversial. The likelihood of an unexpected “full stomach” in these scenarios is very low16,17 and the risk of aspiration rare (1:4,000). In low-risk situations, it is likely that the number-needed-to-test to change anesthetic management and affect outcomes would be very high and probably not cost-effective, although there is a lack of current clinical data available to confirm the optimal application of this diagnostic test.
Acquisition
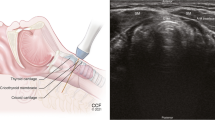
After adjusting the ambient light, the patient’s upper abdomen is exposed and gel is used as an acoustic medium. The patient is scanned consecutively in the supine and then in the right lateral decubitus (RLD) position (Fig. 1). In the RLD position, a larger proportion of the stomach’s content flows towards the more dependent distal antrum, and therefore, scanning in this position increases the test’s sensitivity.6,8 When examination in the RLD position is not possible (e.g., critically ill, trauma), a semi-recumbent position (head elevated 45°) may be an acceptable “second best”, with the supine position being the least sensitive and least accurate patient position.18,19,20
In the adult patient, a curved array low-frequency abdominal probe (2-5 MHz) with abdominal pre-sets is most suited to provide sufficient penetration to identify the relevant anatomical landmarks.6,7,8 In pediatric patients under 40 kg, a linear high-frequency transducer can be used.21 The stomach is imaged in a sagittal plane in the epigastric area, immediately inferior to the xiphoid and superior to the umbilicus. The transducer is swept from the left to the right subcostal margin. Gentle sliding, rotation, and tilting of the probe are used to locate the antrum and to optimize the image while avoiding oblique views from excessive probe rotation that could overestimate the antral size. The gastric antrum (the most distal portion of the organ) is particularly amenable to ultrasound examination. This is due to its superficial and consistent location in the epigastric area with a favourable soft tissue acoustic window through the left lobe of the liver.6,7,8,10 Most importantly, an evaluation of the antrum provides accurate information about the content in the entire organ.6,7,8,10 The gastric body usually has a greater air content that may interfere with the exam and the gastric fundus is difficult to access with ultrasound.6,10 The antrum appears as a superficial hollow viscus with a thick multilayered wall immediately inferior to the left lobe of the liver and anterior to the body of the pancreas.7 Both the inferior vena cava and the aorta lie posterior to the antrum, and both can be identified in the course of the exam. Nevertheless, a standardized plane at the level of the aorta is used for a quantitative evaluation of the volume of gastric fluid.8 Other vascular landmarks include the superior mesenteric artery or vein. The gastric wall is approximately 4-6 mm thick in the adult patient and has five distinct sonographic layers that are best visualized in the empty state with a high-frequency transducer. The five layers (from the inner to the outer surface) are as follows: a) mucosal-air interface, b) muscularis mucosa, c) submucosa, d) muscularis propria, and e) serosa.7 With a low-frequency transducer, only the muscularis propria is consistently observed. This thick muscularis layer, along with the characteristic location of the antrum, allows differentiating the stomach from other portions of the gastrointestinal tract with a thinner, less prominent smooth muscle layer.
Interpretation
After identifying all relevant structures, the nature of the gastric content (empty, clear fluid, thick fluid/solid) may be established based on qualitative findings. When the stomach is empty, the antrum is either flat or round with juxtaposed anterior and posterior walls. When it is round or ovoid, its appearance has been compared with a ”bull’s eye” or “target” pattern (Fig. 2).6,7,10
Thick fluid, milk, or suspensions have a hyperechoic, usually homogenous aspect. Following the ingestion of solid food, the air content mixed with the solid bolus during the chewing process forms a mucosal-air interface along the anterior wall of the distended antrum. This large area of “ring-down” air artefacts blurrs the gastric content, the posterior wall of the antrum, the pancreas, and the aorta. This is often referred to as a “frosted-glass” pattern (Fig. 3).7 After a variable time interval, this air is displaced, and the antrum then appears distended with better appreciable content of typically mixed echogenicity (Fig. 4).
Normal gastric secretions and clear fluids (e.g., water, tea, apple juice, black coffee) appear anechoic or hypoechoic. The antrum becomes round and distended with thin walls as the volumes increases (Fig. 5). Immediately after fluid intake, gas bubbles can be appreciated as small punctuate echoes, but they disappear rapidly within minutes of ingestion (“starry night” appearance, Fig. 6).7
Sonographic image showing the “starry night appearance” of the stomach represented by clear fluid mixed with gas bubbles. A = antrum; Ao = aorta; D = diaphragm; L = liver; P = pancreas; R = rectus abdominis muscle; S = spine; Sma = superior mesenteric artery. Used with permission from gastricultrasound.org
Healthy subjects who have fasted for elective surgery commonly present with either a completely empty antrum, with no content visible in either the supine or the RLD position (Grade 0 antrum), or with a small, negligible volume of baseline secretions (typically ≤ 1.5 mL·kg−1), which is usually appreciated only in the RLD position (Grade 1 antrum).8,22 The upper limit of normal baseline gastric volume is still somewhat controversial. Nevertheless, we know that the mean value is approximately 0.6 mL·kg−1 and that volumes of up to 100-130 mL (about 1.5 mL·kg−1) are common in healthy fasted subjects and do not pose a significant risk for aspiration.23,24,25 Previously suggested thresholds of “risk” (0.4 mL·kg−1 and 0.8 mL·kg−1)26,27 were extrapolations from volumes of hydrochloric acid directly instilled into the tracheas of animals. These values are not supported by a plethora of human data demonstrating that such volumes of gastric secretions are well within the normal range for healthy fasted individuals with a low risk for aspiration.
Conversely, a volume of clear fluid in excess of 1.5 mL·kg−1 or any amount of solid or particulate content in the stomach suggests a non-fasting state (or a “full stomach”), likely increasing the risk of aspiration. A Grade 2 antrum (defined as an appreciable amount of clear fluid in both the supine and the RLD postions) is associated with greater fluid volumes, is uncommon in fasted healthy individuals, and suggests a non-fasting state.8,16,22
Therefore, when the stomach contains clear fluid (homogeneous, hypoechoic, or anechoic), a volume assessment can help differentiate a negligible volume consistent with baseline secretions vs a higher-than-baseline volume.8,10,11
It has been consistently shown that a single cross-sectional area (CSA) of the gastric antrum measured in a standardized manner correlates with the total gastric volume and this correlation is stronger in the RLD position.6,28,29,30,31,32 Several mathematical models have been reported that describe this numerical relationship.6,8,29,33,34,35,36,37 One such model has been validated against endoscopically guided gastric suctioning for non-pregnant adults with a wide range of ages and weights. This model accurately predicts gastric volume up to 500 mL as follows (Fig. 7):
This model has high intra-rater and inter-rater reliability.38 For a volume evaluation, the antral area is obtained at the level of the aorta, with the antrum at rest (i.e., between peristaltic contractions), and measured using a free-tracing tool of the equipment following the serosa (or outer surface) of the antrum. Similar to other ultrasound measurements for other applications, a mean of three readings is recommended to minimize measurement error.
Predicted gastric fluid volume as determined based on a cross-sectional area of the gastric antrum measured in the right lateral decubitus position and the validated model by Perlas et al. 8 Used with permission from gastricultrasound.org
Medical decision-making
Point-of-care gastric ultrasound is used to stratify individual risk for aspiration and to tailor airway and anesthetic management in situations of clinical equipoise where prandial status is unclear.
An “empty” stomach (Grade 0 antrum) or a low volume of clear fluid within the range of baseline gastric secretions (Grade 1 antrum or ≤ 1.5 mL·kg−1) is consistent with a fasting state and suggests a low risk (Fig. 8). In the absence of other risk factors, the ultrasound confirmation of an empty stomach would indicate that no special airway management precautions (intubation, rapid sequence induction) are required, and that supraglottic airway devices or deep sedation without airway protection may be appropriate management choices. Conversely, solid content or a high volume of clear fluid that is not in keeping with a fasting state suggests a higher-than-baseline risk for aspiration. These findings would indicate that the airway needs to be protected from aspiration with endotracheal intubation and possibly a rapid sequence induction of anesthesia.
The clinical context of each individual patient needs to be taken into account when making a medical decision.11 Specific risk factors for aspiration need to be considered, such as the patient’s history and physical exam, type of procedure (elective or urgent), nature of the last meal, time interval since the last meal, as well as other risk factors for aspiration.39 Ultrasound findings can help turn a 50% pre-test probability of a “full stomach” into a “likely full” or “likely empty” situation, thus guiding anesthetic management accordingly. A growing body of evidence suggests that the addition of point-of-care gastric ultrasound to a patient’s history and physical exam can modify aspiration risk assessment and anesthetic management in a substantial proportion of cases when clinical data alone are uncertain.16,17,40,41,42 A prospective study of 38 elective surgical patients who had not complied with fasting instructions reported a change in anesthetic management in 72% of the cases with point-of-care gastric ultrasound vs with management based on history alone and a trend towards a lower incidence of surgical delays.40
Morbidly obese patients
The incidence of obesity is growing globally. Obese subjects are usually considered to be at increased risk of aspiration and are therefore of particular interest. Although the greater depth of the antrum (around 7 cm) and the increased visceral adiposity can make the examination more challenging, gastric sonography is feasible in 95% of severely obese individuals.43,44 The previously mentioned mathematical model for the assessment of gastric volume has been shown to be reasonably accurate in severely obese subjects (BMI > 40 kg·m−2), with a trend towards an overestimation of the volume, particularly at low volume states (mean overestimation of 35 mL).44 Overall, obese patients presented significantly larger baseline antral CSA and total gastric volumes than their non-obese counterparts.43,44 Nevertheless, the gastric volume per unit of body weight (0.57-0.7 mL·kg−1 and the relative distribution of antral grades were similar to those observed in non-obese subjects.22,43,44
Pediatric patients
For children weighing < 40 kg, a linear high-frequency transducer provides the best images through improved spatial resolution, while a low-frequency curvilinear transducer is recommended for best imaging in larger pediatric patients.21 Similar to the adult population, most fasted children have either a Grade 0 or a Grade 1 antrum. The range of fasting gastric volume per unit of body weight is remarkably constant across all ages and body habitus, with an upper limit of normal in the range of 1.2-1.5 mL·kg−1 for pediatric patients.21,30 A linear correlation between the antral CSA and the gastric volume was described in a study of 100 fasting children, and this correlation was again stronger when measured in the RLD position.30 Point-of-care gastric ultrasound has been used to determine the most appropriate anesthetic technique for the management of hypertrophic pyloric stenosis.45 In addition, a bedside gastric examination has been reported in children for a different diagnostic application-i.e., the detection and monitoring of ingested foreign bodies (batteries, hairclips, coins, etc.).46,47,48,49 In this context, it has been noted that the additional ingestion of water may aid in the positive identification of the foreign body as a hyperechoic structure within a hypoechoic background of clear fluid.47
Critically ill patients and emergency medicine
Two pilot studies have investigated the use of gastric POCUS in critically ill patients.19,20 A preliminary proof-of-concept study reported that novice examiners could identify the antrum in 65% of patients in the supine position following only four hours of training, and that antral CSA correlated well with the assessment of tomographic volume.19 It has also been suggested that a craniocaudal diameter may be a simple surrogate of CSA and residual gastric volume.20
Gastric ultrasound may be used for indications other than assessment of content and risk of aspiration. Confirmation of nasogastric tube placement in the stomach or duodenum has been reported by either direct imaging of the tip or indirect confirmation through air instillation (“dynamic fogging”), and it has also been used for the diagnosis of gastric outlet obstruction.50,51
Obstetric patients
Pulmonary aspiration remains one of the most feared complications in obstetric anesthesia.52 Regardless of the planned anesthetic technique, an empty stomach is highly desirable prior to anesthetic induction. Gastric emptying in healthy non-labouring pregnant women is similar to that of non-pregnant patients, but it is significantly prolonged once labour begins and appears to return to normal only many hours after delivery.53,54 There are several clinical situations in obstetric anesthesia where knowing the status of the gastric content may be critical for clinical management.11 Therefore, real-time ultrasound assessment may allow an opportunity to improve patient safety.55 Although the general principles and anatomical landmarks of the ultrasound examination of pregnant women are similar to those of non-pregnant subjects, some technical details may differ. Identification of the gastric antrum can be more difficult in pregnant patients due to the gravid uterus and the moving fetus. The stomach is displaced more cephalad and to the right compared with non-pregnant subjects, and dynamic characteristics, such as a fast shallow breathing and hyperdynamic circulation, may pose additional challenges to the exam.31,32,56 Finally, the presence of the gravid uterus will determine a slightly steeper angle between xiphoid and abdomen, which may make probe placement more difficult.31,32
In 1992, a novel study by Carp et al. evaluating the nature of gastric contents for a qualitative ultrasound assessment rendered promising but less than optimal results. Their findings showed that only a markedly distended stomach was appreciable and an empty stomach could not be consistently identified.54 Recent advances in ultrasound imaging, such as multibeam technology and improved engineering, now allow a much higher special resolution. Arzola et al. showed substantial agreement and reliable diagnosis when evaluating various gastric contents after a conventional fasting period of solids and clear fluids in the third trimester of pregnancy.31 Although Barboni et al. suggested an initial slower gastric emptying of solid contents after a standardized meal in patients scheduled for elective Cesarean deliveries, no ultrasound examination was carried out beyond six hours.56 Nevertheless, after following current fasting guidelines (six to eight hours for solids and two hours for clear fluids), no solid gastric contents were found in two cohort studies in term pregnant women before elective Cesarean delivery. These results suggest that these guidelines to ensure an empty stomach are equally effective as in the non-pregnant population.32,57 Clear fluids were initially assessed by Wong et al. in obese and non-obese pregnant women, confirming normal gastric emptying during pregnancy.58,59 Volume estimation based on a CSA of the gastric antrum has been the focus of multiple recent investigations. Several mathematical models have been described in various examining positions and different clinical scenarios.60,61,62,63 Based on these models, there is currently a search for cut-off values of antral CSA to discriminate different levels of risk.60,61,62,63 While a cut-off value has been reported to discriminate a completely empty stomach (Grade 0 antrum) from one with low fluid volume (Grade 1 antrum), this type of threshold is of limited clinical applicability, as both the Grade 0 and the Grade 1 antrum are common in fasted individuals and carry no significant risk. A more clinically relevant “cut-off” value of CSA would be one that differentiates a baseline volume (Grade 0 or Grade 1 antrum or ≤ 1.5 mL·kg−1) from a greater-than-baseline condition (Grade 2 antrum or > 1.5 mL·kg−1). Although Bataille et al.60 and Jay et al.61 reported antral size during labour, patients were not allowed to take any oral intake, which deviates from most current recommendations in obstetric practice.60 In contrast, Zieleskiewicz et al. based their report on women who were allowed to drink water at their convenience during established labour under effective epidural analgesia.62 Arzola et al. proposed a mathematical model to estimate gastric volume in pregnant women in the third trimester.63 Although the ingested volume of fluid rather than suction under gastroscopic examination was used as the reference standard, the resulting model very closely resembles the previous predictive model described by Perlas et al. in adult non-pregnant subjects.8 Based on these data, an antral CSA of 9.6 cm2 in the semi-recumbent right lateral position can discriminate a low from a high gastric volume (> 1.5 mL·kg−1).63 This value of antral CSA could be a simple surrogate measure that could facilitate the interpretation of examination findings when clear fluid is observed in the antrum. Further research is warranted to develop decision-making strategies based on peripartum gastric ultrasound assessment.
Limitations and areas of further research
It is important to consider both the technical limitations of this diagnostic test as well as the conceptual framework within which it is used. From a technical standpoint, gastric ultrasound has been validated in patients with normal gastric anatomy and may therefore not be reliable or accurate in subjects with previous gastric surgery (e.g., partial gastrectomy, gastric bypass) or large hiatus hernias. Information on the nature of gastric content (clear fluid, solid) could still be useful in these settings, but volume estimation, in particular, will likely be inaccurate in these subjects.
Regarding the conceptual framework for the use of gastric POCUS, it is first important to consider that this test evaluates only one of the determinants of aspiration risk-i.e., gastric content, nothing more or less. The risk of clinically important aspiration is partly determined by the presence of gastric content at the time of anesthetic induction, but it is also influenced by other independent factors, such as a) co-existing diseases of the upper gastrointestinal tract (e.g., achalasia and gastroesophageal reflux disease), b) the anesthetic technique, and c) the events related to airway management (e.g., unexpected difficult intubation requiring prolonged manual ventilation). So, point-of-care gastric ultrasound evaluates an important, but not the only, determinant of risk.
A second significant issue is that, like any ultrasound examination (and any diagnostic test for that matter), gastric POCUS is not infallible. In fact, up to 3-5% of all exams may be inconclusive, and the diagnostic accuracy of gastric ultrasound to detect a full stomach (i.e., the sensititvity, specificity, and positive and negative predictive values of gastric POCUS) remains to be studied.6,8,43
Although both the positive and negative predictive values are important attributes of a test, given the implications of a correct “empty” stomach diagnosis for aspiration prevention, the negative predictive value of gastric POCUS is arguably of utmost importance. Furthermore, the diagnostic accuracy of the test will be related to the experience of the sonographer. It has been established that, on average, approximately 33 practice examinations followed by expert feedback are needed for anesthesia fellows learning to perform gastric ultrasound to obtain an accurate diagnosis in 95% of cases. Nevertheless, the optimal way to learn and teach this skill has yet to be established.64 Gastric content is dynamic and changes quickly over time. Therefore gastric POCUS gives information that may be accurate only at the time of the test. For example, a stomach that is found to be “full” prior to induction of anesthesia may not be so at the end of a surgical procedure and vice versa. So, the test may be repeated as dictated by the clinical situation. Along those lines, ensuring an empty stomach prior to extubation in questionable cases (e.g., difficult airway; critically ill subjects) may be an appropriate additional indication.
A third important limitation is the difficulty to prove conclusively that the introduction of this test will lead to a reduction in episodes of clinically important aspiration and tangible improvements in patient outcomes. A randomized-controlled trial of patients with unclear prandial status with enough power to answer this question would need to be very large and would be logistically difficult to accomplish. This limitation is shared by other POCUS applications, and many current clinical recommendations are based on observational data. For example, the addition of lung ultrasound to a Focused Assessment with Sonography in Trauma (FAST) protocol for evaluating trauma victims is based on the fact that bedside ultrasound is more sensitive than chest x-ray to diagnose pneumothorax. Nevertheless, there is a lack of clinical evidence that FAST improves survival or other important patient outcomes. Similarly, the American Heart Association currently recommends that bedside ultrasound may be considered during resuscitation to identify potentially reversible causes of cardiac arrest. This is suggested despite inadequate evidence to evaluate whether there is any survival benefit of cardiac ultrasound during Advanced Cardiovascular Life Support (ACLS). Furthermore, although the performance of a diagnostic test is not a therapeutic intervention itself, every diagnostic test is potentially destined to lead to clinical interventions that may themselves be beneficial or harmful. So far, we have scant evidence of the effect of gastric ultrasound on important clinical outcomes. The assertion that gastric ultrasound is beneficial in the management of perioperative patients is currently a hypothesis that needs to be tested with properly designed clinical studies examining clinical outcomes rather than just surrogate outcomes.
Given the above limitations and knowledge gaps, further research is needed to define the diagnostic accuracy of gastric POCUS from a Bayesian perspective, including determination of sensitivity, specificity, positive and negative predictive values, and cost-effectiveness considerations. The above information will help define the clinical role of this test, including the determination of appropriate indications. This knowledge is particularly relevant within the current “Choosing Wisely Canada” initiative.
Back to the clinical scenario
In our case scenario, an “empty” test result (no content at all or ≤ 1.5 mL·kg−1 of clear fluid) would be compatible with a fasting state. It would suggest that ingestion did not in fact occur, and the “memory” of it may be related to confusion or delirium, which is highly prevalent in this clinical context. This negative result would suggest that the risk of aspiration is low, and it may be safe to proceed with surgery with a slowly titrated induction of anesthesia as dictated by the patient’s cardiac condition.
Conversely, the documentation of solid or particulate content or a grossly distended stomach with >1.5 mL·kg−1 of clear fluid would suggest that the ingestion did likely take place, the stomach has not fully emptied, and the risk of aspiration is higher than baseline. This finding would support postponing the surgery until either a) a recommended fasting interval has been achieved or b) the stomach is confirmed to have emptied on a repeat examination.
Conclusions
Gastric POCUS is an emerging application of sonography increasingly used in anesthesia education and practice. Its validity and reliability have been evaluated for a variety of patient populations, including pregnant and non-pregnant adults, severely obese patients, and pediatric patients. It is likely most useful to define risk and guide patient management when prandial status is uncertain or unknown. Further research is warranted to establish the diagnostic accuracy of gastric POCUS from a Bayesian perspective, determine the impact of this test on patient outcomes and on healthcare economics, and establish how best to incorporate this new skill into existing educational curricula.64,65,66
References
Lockey DJ, Coats T, Parr MJ. Aspiration in severe trauma: a prospective study. Anaesthesia 1999; 54: 1097-8.
Lienhart A, Auroy Y, Pequignot F, et al. Survey of anesthesia-related mortality in France. Anesthesiology 2006; 105: 1087-97.
Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology 1993; 78: 56-62.
Cook TM, Woodall N, Frerk C. Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011; 106: 617-31.
Sakai T, Planinsic RM, Quinlan JJ, Handley LJ, Kim TY, Hilmi IA. The incidence and outcomes of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis. Anesth Analg 2006; 103: 941-7.
Perlas A, Chan VW, Lupu CM, Mitsakakis N, Hanbidge A. Ultrasound assessment of gastric content and volume. Anesthesiology 2009; 111: 82-9.
Cubillos J, Tse C, Chan VW, Perlas A. Bedside ultrasound assessment of gastric content: an observational study. Can J Anesth 2012; 59: 416-23.
Perlas A, Mitsakakis N, Liu L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination. Anesth Analg 2013; 116: 357-63.
Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med 2007; 35(5 Suppl): S126-30.
Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014; 113: 12-22.
Perlas A, Van de Putte P, Van Houwe P, Chan VW. I-AIM framework for point-of-care gastric ultrasound. Br J Anaesth 2016; 116: 7-11.
Benhamou D. Ultrasound assessment of gastric contents in the perioperative period: why is this not part of our daily practice? Br J Anaesth 2015; 114: 545-8.
Mahmood F, Matyal R, Skubas N, et al. Perioperative ultrasound training in anesthesiology: a call to action. Anesth Analg 2016; 122: 1794-804.
Lucas DN, Elton CD. Through a glass darkly - ultrasound imaging in obstetric anaesthesia. Anaesthesia 2016; 71: 617-22.
Bahner DP, Hughes D, Royall NA. I-AIM: a novel model for teaching and performing focused sonography. J Ultrasound Med 2012; 31: 295-300.
Van de Putte P, Vernieuwe L, Jerjir A, Verschueren L, Tacken M, Perlas A. When fasted is not empty: a retrospective cohort study of gastric content in fasted surgical patients. Br J Anaesth 2017; 118: 363-71.
Bouvet L, Desgranges FP, Aubergy C, et al. Prevalence and factors predictive of full stomach in elective and emergency surgical patients: a prospective cohort study. Br J Anaesth 2017; 118: 372-9.
Koenig SJ, Lakticova V, Mayo PH. Utility of ultrasonography for detection of gastric fluid during urgent endotracheal intubation. Intensive Care Med 2011; 37: 627-31.
Hamada SR, Garcon P, Ronot M, Kerever S, Paugam-Burtz C, Mantz J. Ultrasound assessment of gastric volume in critically ill patients. Intensive Care Med 2014; 40: 965-72.
Sharma V, Gudivada D, Gueret R, Bailitz J. Ultrasound-assessed gastric antral area correlates with aspirated tube feed volume in enterally fed critically ill patients. Nutr Clin Pract 2017; 32: 206-11.
Spencer AO, Walker AM. Antral sonography in the paediatric patient: can transducer choice affect the view? Br J Anaesth 2015; 114: 1002-3.
Perlas A, Davis L, Khan M, Mitsakakis N, Chan VW. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg 2011; 113: 93-7.
Hutchinson A, Maltby JR, Reid CR. Gastric fluid volume and pH in elective inpatients. Part I: coffee or orange juice versus overnight fast. Can J Anaesth 1988; 35: 12-5.
Agarwal A, Chari P, Singh H. Fluid deprivation before operation. The effect of a small drink. Anaesthesia 1989; 44: 632-4.
Maltby JR, Lewis P, Martin A, Sutherland LR. Gastric fluid volume and pH in elective patients following unrestricted oral fluid until three hours before surgery. Can J Anaesth 1991; 38(4 Pt 1): 425-9.
Roberts RB, Shirley MA. Reducing the risk of acid aspiration during cesarean section. Anesth Analg 1974; 53: 859-68.
Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth 1999; 65: 453-60.
Tomomasa T, Tabata M, Nako Y, Kaneko H, Morikawa A. Ultrasonographic assessment of intragastric volume in neonates: factors affecting the relationship between intragastric volume and antral cross-sectional area. Pediatr Radiol 1996; 26: 815-20.
Schmitz A, Schmidt AR, Buehler PK, et al. Gastric ultrasound as a preoperative bedside test for residual gastric contents volume in children. Paediat Anaesth 2016; 26: 1157-64.
Spencer AO, Walker AM, Yeung AK, et al. Ultrasound assessment of gastric volume in the fasted pediatric patient undergoing upper gastrointestinal endoscopy: development of a predictive model using endoscopically suctioned volumes. Paediat Anaesth 2015; 25: 301-8.
Arzola C, Cubillos J, Perlas A, Downey K, Carvalho JC. Interrater reliability of qualitative ultrasound assessment of gastric content in the third trimester of pregnancy. Br J Anaesth 2014; 113: 1018-23.
Arzola C, Perlas A, Siddiqui NT, Carvalho JC. Bedside gastric ultrasonography in term pregnant women before elective cesarean delivery: a prospective cohort study. Anesth Analg 2015; 121: 752-8.
Fujigaki T, Fukusaki M, Nakamura H, Shibata O, Sumikawa K. Quantitative evaluation of gastric contents using ultrasound. J Clin Anesth 1993; 5: 451-5.
Ricci R, Bontempo I, Corazziari E, La Bella A, Torsoli A. Real time ultrasonography of the gastric antrum. Gut 1993; 34: 173-6.
Hveem K, Hausken T, Berstad A. Ultrasonographic assessment of fasting liquid content in the human stomach. Scand J Gastroenterol 1994; 29: 786-9.
Bouvet L, Miquel A, Chassard D, Boselli E, Allaouiche B, Benhamou D. Could a single standardized ultrasonographic measurement of antral area be of interest for assessing gastric contents? A preliminary report. Eur J Anaesthesiol 2009; 26: 1015-9.
Bouvet L, Mazoit JX, Chassard D, Allaouchiche B, Boselli E, Benhamou D. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume. Anesthesiology 2011; 114: 1086-92.
Kruisselbrink R, Arzola C, Endersby R, Tse C, Chan V, Perlas A. Intra- and interrater reliability of ultrasound assessment of gastric volume. Anesthesiology 2014; 121: 46-51.
Bouvet L, Chassard D. Ultrasound assessment of gastric content in the obese patient: one more step for patient safety. Anesth Analg 2014; 119: 1017-8.
Alakkad H, Kruisselbrink R, Chin KJ, et al. Point-of-care ultrasound defines gastric content and changes the anesthetic management of elective surgical patients who have not followed fasting instructions: a prospective case series. Can J Anesth 2015; 62: 1188-95.
Van de Putte P. Bedside gastric ultrasonography to guide anesthetic management in a nonfasted emergency patient. J Clin Anesth 2013; 25: 165-6.
Tampo A, Suzuki A, Ijiri E, Kunisawa T, Iwasaki H. Preanesthetic gastric assessment with sonography for a patient with a full stomach. J Clin Anesth 2013; 25: 164-5.
Van de Putte P, Perlas A. Gastric sonography in the severely obese surgical patient: a feasibility study. Anesth Analg 2014; 119: 1105-10.
Kruisselbrink R, Arzola C, Jackson T, Okrainec A, Chan V, Perlas A. Ultrasound assessment of gastric volume in severely obese individuals: a validation study. Br J Anaesth 2017; 118: 77-82.
Gagey AC, de Queiroz Siqueira M, Desgranges FP, et al. Ultrasound assessment of the gastric contents for the guidance of the anaesthetic strategy in infants with hypertrophic pyloric stenosis: a prospective cohort study. Br J Anaesth 2016; 116: 649-54.
Salmon M, Doniger SJ. Ingested foreign bodies: a case series demonstrating a novel application of point-of-care ultrasonography in children. Pediatr Emerg Care 2013; 29: 870-3.
Jecković M, Anupindi SA, Barbir SB, Lovrenski J. Is ultrasound useful in detection and follow-up of gastric foreign bodies in children? Clin Imaging 2013; 37: 1043-7.
Horowitz R, Cico SJ, Bailitz J. Point-of-care ultrasound: a new tool for the identification of gastric foreign bodies in children? J Emerg Med 2016; 50: 99-103.
Yamamoto M, Koyama T, Agata M, Ouchi K, Kotoku T, Mizuno Y. Diagnosis of ingested foreign body in the stomach by point-of-care ultrasound in the upright and slightly forward tilting position (bowing position). Pediatr Emerg Care 2017. https://doi.org/10.1097/PEC.0000000000001125.
Brun PM, Chenaitia H, Lablanche C, et al. 2-point ultrasonography to confirm correct position of the gastric tube in prehospital setting. Mil Med 2014; 179: 959-63.
Gottlieb M, Nakitende D. Identification of gastric outlet obstruction using point-of-care ultrasound. Am J Emerg Med 2017. https://doi.org/10.1016/j.ajem.2017.03.024.
Cantwell R, Clutton-Brock T, Cooper G, et al. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report on the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011; 118 (Suppl 1): 1-203.
O’Sullivan G. Gastric emptying during pregnancy and the puerperium. Int J Obstet Anesth 1993; 2: 216-24.
Carp H, Jayaram A, Stoll M. Ultrasound examination of the stomach contents of parturients. Anesth Analg 1992; 74: 683-7.
Kinsella SM. Position, position, position - terminology during stomach ultrasound in pregnant women. Anaesthesia 2016; 71: 1264-7.
Barboni E, Mancinelli P, Bitossi U, et al. Ultrasound evaluation of the stomach and gastric emptying in pregnant women at term: a case-control study. Minerva Anestesiol 2016; 82: 543-9.
Rouget C, Chassard D, Bonnard C, Pop M, Desgranges FP, Bouvet L. Changes in qualitative and quantitative ultrasound assessment of the gastric antrum before and after elective caesarean section in term pregnant women: a prospective cohort study. Anaesthesia 2016; 71: 1284-90.
Wong CA, Loffredi M, Ganchiff JN, Zhao J, Wang Z, Avram MJ. Gastric emptying of water in term pregnancy. Anesthesiology 2002; 96: 1395-400.
Wong CA, McCarthy RJ, Fitzgerald PC, Raikoff K, Avram MJ. Gastric emptying of water in obese pregnant women at term. Anesth Analg 2007; 105: 751-5.
Bataille A, Rousset J, Marret E, Bonnet F. Ultrasonographic evaluation of gastric content during labour under epidural analgesia: a prospective cohort study. Br J Anaesth 2014; 112: 703-7.
Jay L, Zieleskiewicz L, Desgranges FP, et al. Determination of a cut-off value of antral area measured in the supine position for the fast diagnosis of an empty stomach in the parturient: a prospective cohort study. Eur J Anaesthesiol 2017; 34: 150-7.
Zieleskiewicz L, Boghossian MC, Delmas AC, et al. Ultrasonographic measurement of antral area for estimating gastric fluid volume in parturients. Br J Anaesth 2016; 117: 198-205.
Arzola C, Perlas A, Siddiqui NT, Downey K, Ye XY, Carvalho JC. Gastric ultrasound in the third trimester of pregnancy: a randomised controlled trial to develop a predictive model of volume assessment. Anaesthesia 2017.
Arzola C, Carvalho JC, Cubillos J, Ye XY, Perlas A. Anesthesiologists’ learning curves for bedside qualitative ultrasound assessment of gastric content: a cohort study. Can J Anesth. 2013; 60: 771-9.
Skubas NJ. Teaching whole body point-of-care ultrasound: advancing the skills of tomorrow’s anesthesiologists. Anesthesiology 2015; 123: 499-500.
Ramsingh D, Rinehart J, Kain Z, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology 2015; 123: 670-82.
Conflict of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Perlas, A., Arzola, C. & Van de Putte, P. Point-of-care gastric ultrasound and aspiration risk assessment: a narrative review. Can J Anesth/J Can Anesth 65, 437–448 (2018). https://doi.org/10.1007/s12630-017-1031-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-017-1031-9