Abstract
Objective
To evaluate the interobserver agreement for the features of natal cleft pilonidal sinus disease (PSD) on magnetic resonance imaging (MRI) and propose a standardized checklist for reporting PSD on MRI.
Materials and methods
Forty MRI studies of 39 discrete patients with PSD were retrospectively evaluated by five independent radiologists using a standardized checklist. Fleiss’ Kappa (k) coefficients of agreement were used to test the agreement between categorical variables. The MRI features of the natal cleft sepsis associated with PSD were classified into four main categories: morphology, branching and extensions, external skin openings, and the relationship of the PSD to the coccyx. A survey was created and disseminated online among general surgeons who treat patients with PSD to assess the relevance of the MRI features proposed in the standardized checklist.
Results
The overall agreement regarding the identification of morphology of the natal cleft sepsis was moderate (k = 0.59). Lateral and caudal extensions interobserver agreement was substantial (k = 0.64 and 0.71, respectively). However, the overall agreement regarding the individual parts of anal sphincter involved was moderate (k = 0.47). Substantial interobserver agreement was found in assessing the proximity of the PSD to the coccyx (k = 0.62).
Conclusion
Preoperative MRI can delineate the extensions and branching of PSD with substantial agreement. MRI is superior in describing the deep extensions of PSD with better reliability than assessing the number and locations of the external openings. Expert consensus agreement is needed to establish the MRI features necessary for optimal reporting of PSD.
Clinical relevance statement
MRI can offer valuable information about the extent of sepsis associated with pilonidal sinus disease, particularly in cases with involvement of critical anatomical structures such as the coccyx and anal triangle. MRI can potentially contribute to more accurate patient stratification and surgical planning.
Key Points
• The interobserver agreement for assessing PSD’s lateral and caudal extension on MRI is substantial.
• MRI can describe deep extensions and branching of PSD with superior reliability than assessing the number and site of external openings.
• Reporting the relationship between natal cleft sepsis in PSD and the anal region may influence the surgical approach and postoperative healing.
Similar content being viewed by others
Introduction
Pilonidal sinus disease (PSD) is a recurrent suppurative condition that commonly affects the natal cleft region in young patients of both sexes [1]. Its prevalence in the general population is approximately 26 out of 100,000 [2], with a higher incidence among males, hirsute, and obese individuals [3]. While PSD was previously believed to be congenital, the current prevailing theory suggests that loose hairs invade the skin surface, triggering a foreign body reaction that leads to inflammation and infection within the hair follicle, resulting in the characteristic midline pit necessary for diagnosis [4].
Different terms such as pilonidal cyst, abscess, or sinus are used interchangeably to describe this condition. PSD serves as an umbrella term covering various abnormalities and stages of presentation, including acute pilonidal abscess, chronic pilonidal sinus, and recurrent or complex pilonidal sinus. However, there is a lack of consensus on a classification system for the appearance of PSD [5, 6]. A recent systematic review of surgical classification systems for PSD noted that the location and number of sinuses defined those classifications but lacked evidence to support their use [6].
PSD is clinically diagnosed and typically requires surgical intervention. Historically, excision and healing by primary closure or secondary intention (“left-open”) have been common surgical approaches. Several other surgical options are available, including less invasive techniques and phenol injection [7]. The management of complications, particularly recurrences, poses a significant challenge for surgeons and can result from inadequate excision, delayed wound healing, or wound infection [7]. Preoperative mapping of PSD extensions is crucial for controlling natal cleft sepsis and ensuring proper drainage and excision of the sinus [8]. Intraoperative mapping using methylene blue is frequently performed. However, a study suggested that its use for guiding PSD surgery may lead to inadequate excision without evidence of reducing recurrence rates [9].
Imaging plays a limited role in PSD. Few studies have evaluated the use of ultrasonography (US) to assess the extensions of PSD for better excision and reduced recurrence rates. Superficial US has been suggested as an accurate modality for mapping the sepsis but proved more beneficial in distinguishing PSD from perianal fistulas [10, 11]. A recent consensus statement recommended MRI as a valuable tool for investigating complex PSD cases, especially in differentiating it from fistula in-ano [12]. Additionally, a study found MRI to be sensitive in distinguishing PSD and fistula-in-ano, suggesting that MRI can detect sepsis in both conditions with similar accuracy [13]. This study also found that, although perianal fistula and PSD share similar features on MRI, the absence of intersphincteric sepsis and internal opening in PSD distinguishes the two conditions. Preoperative MRI has been established as the standard of care for evaluating perianal fistulas based on several highly cited outcome studies [14,15,16,17], yet its use in PSD has not been widely adopted.
While there is extensive literature on PSD in terms of clinical data and surgical management of complicated recurrent cases, there is a notable lack of indexed medical literature on how to report PSD on MRI. Accordingly, we aimed to investigate interobserver agreement in identifying PSD on MRI and offer a practical guide for radiologists reporting PSD on MRI, highlighting the necessary information that surgeons require before surgery.
Materials and methods
Institutional Review Board approval was obtained. Need for consent was waived due to the retrospective nature of the study and the fact that the data presented would be anonymized.
Patients
Electronic records of all patients undergoing MRI fistulography for natal cleft sepsis at a tertiary referral hospital (n = 251) from January 2018 to December 2019 were reviewed using the local PACS system in the radiology department. Patients with a clinical diagnosis of pilonidal sinus disease were included, yielding 40 MRI studies of 39 discrete patients (36 male, 3 female). Patients with fistula-in-ano (n = 209) and hidradenitis suppurativa (n = 2) were excluded.
MR imaging
All patients were imaged on one of two 1.5-T MRI machines (Achieva or Intera, Philips Medical System) in the supine position using a pelvic phased-array coil. No oral or intravenous contrast agent was administered. T2–weighted images turbo spin-echo sequences were acquired in three planes: axial, coronal, and sagittal (repetition time ms/echo time ms (TR/TE) 4000/100, field of view (FOV) 240–260 mm, slice thickness 2–4 mm, gap 0–0.5 mm, number of signals acquired 2, flip angle 90, matrix 512 × 512). STIR (short tau inversion recovery) weighted images were acquired in three planes: axial, coronal, and sagittal (repetition time ms/echo time ms (TR/TE) 2600/60, inversion time 150 ms, field of view (FOV) 240–260 mm, slice thickness 2–4 mm, gap 0–0.5 mm, number of signals acquired 2, flip angle 90, matrix 512 × 512).
Image analysis
MRI studies were anonymized, and image analysis was done using RadiAnt DICOM viewer (Medixant). Five radiologists independently analyzed the images. One reader was a radiologist specialized in lower gastrointestinal (GI) and pelvic floor imaging (M.A.) with eight years of radiological experience. Two GI radiologists (N.M. and S.M.), each with nine years of radiological experience, and two general radiologists (S.A. and M.S.), each with eight years of radiological experience. The readers were blinded to the age, complaint, and clinical findings, but they were aware that all cases had natal cleft sepsis. Based on a recent systematic review of surgical classifications of PSD [6], a standardized checklist (Table 1) was formulated by a pelvic floor radiologist (M.A.) under the supervision of two senior GI radiologists (A.G. and M.O.) with 14 and 19 years of radiological experience, respectively. The checklist was transferred to an Excel spreadsheet (Microsoft Corporation). The data were represented as a drop-down list from which the readers could select the most appropriate choice to describe the natal cleft sepsis, as illustrated in Table 1. All measurements were standardized in millimeters. Prior to image analysis, an introductory meeting was held to clarify and discuss the checklist and define the different MRI features of PSD.
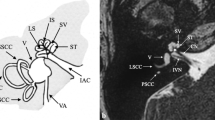
The natal cleft was identified as the midline intergluteal groove extending from the mid-sacral level blending inferiorly with the perineum [18]. The navicular area was defined as a ship-shaped region bounded laterally by the edges of the natal cleft and inferiorly by the apex of the anal triangle corresponding to the tip of the coccyx [19] (Fig. 1). Natal cleft sepsis indicative of PSD was recognized on MRI by the presence of high T2/STIR signal intensity at the midline or paramedian position within the natal cleft.
Morphological features of sepsis were described as either (i) “cyst/cyst-like” defined as a rounded/ovoid/short linear fluid signal, (ii) a “tract” defined as a longitudinal tubular structure roughly more than or equal 30 mm, or (iii) an “abscess” defined as an irregular fluid collection with or without surrounding cellulitis. The number of external skin openings was identified, with their location in relation to the navicular area noted as well.
Extension of the sepsis was described as “cranial” if extending cephalad within the subcutaneous tissue overlying the coccyx and/or sacrum. “Caudal” extension of the sepsis was defined if extending caudad beyond the tip of the coccyx. Additional note was made if the sepsis reached the anal sphincter complex (ASCX), whether it involved the external anal sphincter (EAS), extended beyond it to the intersphincteric plane (ISP), or reached the internal anal sphincter (IAS) [12]. “Lateral” extension referred to the extension of the sepsis beyond the lateral edges of the natal cleft reaching the gluteal region.
The proximity of sepsis to the coccyx was assessed if less than 10 mm. Note of abnormally elevated STIR signal intensity of the coccyx was suggestive of possible extension of sepsis deeply causing osteomyelitis [20].
Clinical survey
To evaluate the clinical relevance of the MRI features proposed in the standardized checklist and determine if they could potentially impact surgical management, a survey was designed and disseminated online using Google Forms (Google.com). It was conducted among general surgeons who treat patients with PSD. Details of the survey form and the results obtained can be found in Supplementary Material 1.
Statistical analysis
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 28 (IBM Corporation). Data were summarized using mean, standard deviation, median, minimum, and maximum for quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. Fleiss’ Kappa measure of agreement was used to test agreement between categorical variables. The value of Kappa (k) was used as an indicator of the strength of agreement where the Kappa statistics were interpreted as follows: 0.01–0.20 (slight agreement), 0.21–0.40 (fair agreement), 0.41–0.60 (moderate agreement), 0.61–0.80 (substantial agreement), and 0.81–0.99 (almost perfect agreement) [21]. Testing for inter-rater reliability in numerical data was done using the intra-class coefficient (ICC) and Cronbach’s alpha reliability coefficient with their 95% confidence interval (95% CI). p-values less than 0.05 were considered statistically significant.
Results
Study population
Forty MRI studies of 39 discrete patients were included: 36 male and 3 female. The mean age at the time of MRI was 31 years (age range 16–57 years). One patient underwent a repeat examination after 6 months with an additional finding. Symptoms at the time of MRI examination were natal cleft discharge in all patients (100%). Twenty-five (64%) patients were imaged preoperatively, while 14 patients (36%) had recurrent natal cleft discharge following surgery for PSD. The agreements on the different features of natal cleft sepsis of the 40 MRI studies between the 5 raters are illustrated in Table 2. The count and percentage of each individual rater of the different features of natal cleft sepsis are summarized in Supplementary Material 2.
Agreement on morphology
The overall agreement among the readers regarding the identification of morphology of the natal cleft sepsis was moderate (k = 0.59, 95% CI = 0.51–0.67). Similarly, the agreements for each independent category of morphology, i.e., tract, cyst, and abscess, were also moderate with kappa values of 0.55, 0.59, and 0.50, respectively.
Skin openings
For the number of sinus skin openings depicted on MRI, the overall agreement between the different readers was found to be fair with kappa of 0.27 (95% CI = 0.19–0.34). Similarly, the agreements on single versus multiple openings were fair with k = 0.24 and 0.35, respectively. The identification of the skin openings within the navicular area yielded slight agreement with a kappa value of 0.03.
Branching and extensions
There was substantial agreement among the different readers regarding the caudal extension of sepsis beyond the coccygeal tip with kappa of 0.71 (95% CI = 0.61–0.81). Similarly, the agreement of extension of the sepsis to reach the ASCX was also substantial, with a slightly higher kappa of 0.73. However, the overall agreement regarding the identification of the part of the sphincter involved was moderate (k = 0.47), with fair agreement for the involvement of the EAS (k = 0.21), moderate agreement for the involvement of the IAS (k = 0.42), and slight agreement for the ISP (k = 0.06). Further analysis of the inter-rater agreement of the caudal extension and the involvement of the ASCX based on the subspecialties of the readers is available in Supplementary Material 2.
The overall agreement for the lateral extension of the natal cleft sepsis to the gluteal region was substantial, with kappa of 0.64. However, the agreement for cranial (subcutaneous) extension between the readers was fair (k = 0.23).
Relationship to the coccyx
The overall agreement regarding the proximity of natal cleft sepsis to the coccyx was substantial (k = 0.62). Similarly, there was substantial agreement in the identification of the coccygeal abnormal signal suggestive of osteomyelitis (k = 0.67). However, for the measurements of the distance of PSD from the coccyx, the ICC was 0.22 (95% CI = 0.01–0.56), p-value = 0.018, and Cronbach’s alpha = 0.59 (95% CI = 0.059–0.87), p-value = 0.018. Additional details of the measurements of the PSD relationship to the coccyx are available in Supplementary Material 2.
Clinical survey
A summary of the answers recorded from the 48 surgeons who participated in the online survey is illustrated in Table 3.
Discussion
The results of our study revealed that the overall agreement for the extensions, branching, and relationship to the coccyx of the PSD using MRI was substantial. However, the overall agreement regarding the morphology of sepsis was moderate, and the agreement on the number and site of skin openings was fair to slight.
PSD originates subcutaneously and can extend along the fat planes cranially in the retro-coccygeal region, laterally to the gluteal region, and even caudally to reach the anal triangle [13]. We found substantial interobserver reliability regarding the presence of lateral extensions. A lateral extension of sepsis usually indicates a more complex process and could potentially alter the surgical plan to include a “rhomboid” excision with additional flap, especially if bilateral, to ensure adequate drainage and shorten healing time [22]. Consequently, we believe that radiological reports of PSD should include a comment on lateral extension/branching and its length from the natal cleft (Fig. 2).
When sepsis extends beyond the caudal tip of the coccyx and contacts the ASCX, confusion may arise regarding its origin, potentially overlapping with the diagnosis of perianal fistula [13]. Furthermore, a recent study listed the distance from the upper and lower edges of the PSD and the upper edge of the EAS on MRI as a possible prognostic factor after flap surgical techniques [23]. We found that the overall interobserver agreement regarding the caudal extension beyond the coccyx and the extension to reach the ASCX was substantial. However, the individual agreement for the different parts of the ASCX involved was moderate to slight, likely due to the different experiences of the raters and their familiarity with the ASCX anatomy. Additionally, 85% (41/48) of the surgeons who participated in our survey agreed that knowing the extension of the PSD to the anal triangle and its relationship to the ASCX could alter the surgical decision. This is consistent with a previously published survey of surgeons where the majority concurred that the proximity of the sepsis to the anal canal, although clinically challenging to determine, affects wound healing and impacts the choice of treatment [24]. Hence, we suggest that MRI reporting of PSD should include a comment on the caudal extension of the PSD beyond the coccyx, mention its relation to the anal triangle, and specify the individual parts of the ASCX involved if present (Fig. 3).
Sagittal STIR-weighted image (A) and axial T2-weighted image (B) of a 25-year-old patient complaining of recurrent natal cleft discharge after repeated operative interventions. A showing a large retro-coccygeal fluid collection with a caudal branch extending anteriorly within the posterior aspect of the perianal region, reaching the sphincteric complex (white arrow). B shows the caudal branch traversing the midline aspect of the deep external sphincter opposite 6 o’clock position to reach the left posterior quadrant of the intersphincteric plane, yet no definite penetration of the internal anal sphincter (black arrow)
Conversely, the interobserver agreement for the identification of the cranial extension was only fair (k = 0.23), likely due to the absence of an anatomical landmark to define where the sepsis extends cranially. Therefore, we suggest the inclusion of the upper border of the PSD using the opposing sacral/coccygeal parts as a reference, in addition to the length of the sepsis.
In terms of changes in coccygeal signal and proximity of sepsis to the coccyx, the interobserver agreement was substantial. Although coccygeal osteomyelitis secondary to PSD is a relatively rare complication, we believe that radiologists should be mindful of this serious complication and report it if present. Such findings may lead to a change in surgical decision, potentially requiring drastic procedures like coccygectomy [25]. One of the patients included in our study underwent two MRI scans with a 6-month interval between the two studies, following antibiotic treatment without surgical intervention. The second MRI revealed the development of an abnormal intrinsic signal in the coccyx, suggesting deep extension of the sepsis (Fig. 4).
Pilonidal sinus disease in a 27-year-old male patient who underwent two consecutive MRI examinations 6 months apart with no interval surgical intervention. A and B: Sagittal and axial STIR-weighted images, respectively, of the first MRI showing a fine tract of fluid signal intensity (white arrows) seen near the posterior surface of the first coccygeal segment with normal signal of the coccyx. C and D: Sagittal T2- and axial STIR-weighted images, respectively, from the MRI performed 6 months later showing progression in size to form a small collection associated with newly developed abnormally elevated STIR signal of the adjacent coccygeal segment (arrowhead) suggestive of developing osteomyelitis of the coccyx
The overall agreement regarding the morphological appearance of PSD was only moderate. While for radiologists semantics are generally fundamental, for surgeons treating patients with PSD, apart from the transverse and longitudinal measurements, the morphological distinction between cyst and tract might not be of importance (Fig. 5). In our online survey, most of the surgeons (68%) replied that the morphology of PSD would likely not impact the surgical decision. However, the implication of an intergluteal abscess is crucial because that degree of inflammation can affect the surgical timing, impact healing, and possibly lead to recurrence of the sepsis [26]. Accordingly, we suggest that MRI reports of PSD should confirm or negate the presence of features of acute abscess and surrounding cellulitis (Fig. 6).
(A) Sagittal STIR-weighted image showing an irregular branching subcutaneous retro-coccygeal fluid collection with surrounding extensive inflammatory changes suggestive of cellulitis and presumed two skin openings. (B) Axial T2 WI image showing the collection posterior to the coccyx with no evidence of deeper extension
The overall interobserver agreement regarding the number of external skin openings was only fair, indicating limitations in identifying the skin openings of PSD on MRI. However, this shortcoming in imaging is unlikely to be significant since clinical examination can easily depict the skin openings. In fact, 81% of the surgeons in our survey believed that clinical examination would be sufficient or even superior in detecting the external openings of PSD. Similarly, the overall agreement regarding the presence of skin openings within the navicular area was slight, suggesting that the assessment of the navicular area cannot be simply adopted from surgical and clinical literature to MRI. Additional anatomical landmarks could aid in mapping the disease more accurately.
Limitations
Our study does have limitations. As a retrospective study with no available surgical records of the included patients, we could not evaluate the possible alteration in the surgical planning or the effect on recurrences. Future studies are recommended to assess the impact of these MRI parameters on the surgical outcome and recurrences. Additionally, only one reader was specialized in pelvic floor imaging. While we believe this ensures the generalizability of our results, familiarity with ASCX anatomy could have improved agreement on the degree of involvement of the anal sphincter.
Conclusion
To our knowledge, no prior studies have evaluated the inter-rater agreement for PSD on MRI or proposed a reporting checklist for this condition (Table 4). Preoperative MRI can delineate the extensions and branching of PSD with substantial agreement, particularly for caudal and lateral extensions, which indicate a more complex condition and may necessitate a modification in the surgical approach. MRI is superior in describing the deep extensions of sepsis with better reliability than assessing the number and locations of the external openings. Further validity studies correlating MRI findings with surgical outcomes and postoperative recurrences are recommended.
Our study offers a foundation that can help create expert consensus agreement needed to establish the MRI features necessary for optimal MRI reporting of PSD. We believe that collaboration between radiologists and surgeons in developing a classification system for PSD can significantly enhance patient stratification, leading to tailored surgical management plans and reduced recurrence rates.
Abbreviations
- ASCX :
-
Anal sphincter complex
- CI :
-
Confidence interval
- EAS :
-
External anal sphincter
- IAS :
-
Internal anal sphincter
- ISP :
-
Intersphincteric plane
- MRI :
-
Magnetic resonance imaging
- PSD :
-
Pilonidal sinus disease
References
Bendewald FP, Cima RR (2007) Pilonidal disease. Clin Colon Rectal Surg 20(02):086–095. https://doi.org/10.1055/s-2007-977486
Søndenaa K, Andersen E, Nesvik I, Søreide JA (1995) Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis 10(1):39–44. https://doi.org/10.1007/BF00337585
Humphries AE, Duncan JE (2010) Evaluation and management of pilonidal disease. Surgical Clinics 90(1):113–124. https://doi.org/10.1016/j.suc.2009.09.006
Bascom J (1980). Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery 87(5):567–572
Johnson EK (2016) Pilonidal disease and hidradenitis suppurativa. In: Steele S, Hull T, Read T, Saclarides T, Senagore A, Whitlow C (eds) The ASCRS textbook of colon and rectal surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-25970-3_17
Beal EM, Lee MJ, Hind D et al (2019) A systematic review of classification systems for pilonidal sinus. Tech Coloproctol 23:435–443. https://doi.org/10.1007/s10151-019-01988-x
Grabowski J, Oyetunji TA, Goldin AB et al (2019) The management of pilonidal disease: a systematic review. J Pediatr Surg 54(11):2210–2221. https://doi.org/10.1016/j.jpedsurg.2019.02.055
Anand S, Chauhan S (2017). Pilonidal disease. In: Shiffman M, Low M (eds) Biofilm, pilonidal cysts and sinuses. Recent Clinical Techniques, Results, and Research in Wounds, vol 1. Springer, Cham. https://doi.org/10.1007/15695_2017_8
Idiz UO, Aysan E, Firat D, Bozkurt S, Buyukpinarbasili N, Muslumanoglu M (2014) Safety and/or effectiveness of methylene blue-guided pilonidal sinus surgery. Int J Clin Exp Med 7(4):927–931
Mentes O, Oysul A, Harlak A, Zeybek N, Kozak O, Tufan T (2009) Ultrasonography accurately evaluates the dimension and shape of the pilonidal sinus. Clinics (Sao Paulo) 64(3):189–192. https://doi.org/10.1590/S1807-59322009000300007
Youssef AT (2015) The value of superficial parts and endoanal ultrasonography in evaluating pilonidal disease and excluding perianal sepsis. J Ultrasound 18:237–243. https://doi.org/10.1007/s40477-015-0156-3
Halligan S, Tolan D, Amitai MM et al (2020) ESGAR consensus statement on the imaging of fistula-in-ano and other causes of anal sepsis. Eur Radiol 30:4734–4740. https://doi.org/10.1007/s00330-020-06826-5
Taylor SA, Halligan S, Bartram CI (2003) Pilonidal sinus disease: MR imaging distinction from fistula in ano. Radiology 226(3):662–667. https://doi.org/10.1148/radiol.2263011758
Lunniss PJ, Armstrong P, Barker PG, Reznek RH, Phillips RK (1992) Magnetic resonance imaging of anal fistulae. Lancet 340:394–396. https://doi.org/10.1016/0140-6736(92)91472-k
Buchanan G, Halligan S, Williams A et al (2002) Effect of MRI on clinical outcome of recurrent fistula-in-ano. Lancet 360:1661–1662. https://doi.org/10.1016/S0140-6736(02)11605-9
Chapple KS, Spencer JA, Windsor AC, Wilson D, Ward J, Ambrose NS (2000) Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum 43:511–516. https://doi.org/10.1007/BF02237196
Beets-Tan RG, Beets GL, van der Hoop AG et al (2001) Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology. 218(1):75–84. https://doi.org/10.1148/radiology.218.1.r01dc0575
Scott-Conner CE (2013). Scott-Conner & Dawson: essential operative techniques and anatomy. Lippincott Williams & Wilkins. ISBN: 978–1–45–115172–5
Tezel E (2007) A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis 9(6):575–576. https://doi.org/10.1111/j.1463-1318.2007.01236.x
Skalski MR, Matcuk GR, Patel DB, Tomasian A, White EA, Gross JS (2020) Imaging coccygeal trauma and coccydynia. Radiographics 40(4):1090–1106. https://doi.org/10.1148/rg.2020190132
Landis JR, Koch GG (1977). The measurement of observer agreement for categorical data. Biometrics, 159-s174
Guner A, Cekic AB, Boz A, Turkyilmaz S, Kucuktulu U (2016) A proposed staging system for chronic symptomatic pilonidal sinus disease and results in patients treated with stage-based approach. BMC Surg 16(1):1–7. https://doi.org/10.1186/s12893-016-0134-5
Zou Q, Zhang D, Xian Z et al (2022) Prognostic factors of flap techniques for pilonidal disease based on magnetic resonance imaging and clinical parameters. Asian J Surg 45(1):284–290. https://doi.org/10.1016/j.asjsur.2021.05.021
Wysocki AP, Andersson RE, Gips M, et al (2018). Towards a classification for sacrococcygeal pilonidal disease – Berlin 2017. PSJ 2018; 4(1):5–12.
Gordon KJ, Hunt TM (2016) Osteomyelitis as a complication of a pilonidal sinus. Int J Colorectal Dis 31(1):155–156. https://doi.org/10.1007/s00384-015-2184-z
Milone M, Velotti N, Manigrasso M, Anoldo P, Milone F, De Palma GD (2018) Long-term follow-up for pilonidal sinus surgery: a review of literature with metanalysis. Surgeon 16(5):315–320. https://doi.org/10.1016/j.surge.2018.03.009
Acknowledgements
Special thanks to Prof. Stuart Taylor, University College London, UK, who mentored Mohamed A. Abdelatty as part of the ESGAR research mentorship program throughout the different stages of this study. The authors are also grateful for Hussein Salem for providing the medical illustration.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Mohamed A. Abdelatty.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Amany Salem) has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some of the cases were presented at the RSNA 2020 educational exhibit as an electronic poster titled “MR Imaging of Natal Cleft Sepsis: Pilonidal Sinus Disease and Mimics”.
Methodology
-
Retrospective
-
Observational
-
Performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelatty, M.A., Elmansy, N., Saleh, M.M. et al. Magnetic resonance imaging of pilonidal sinus disease: interobserver agreement and practical MRI reporting tips. Eur Radiol 34, 115–125 (2024). https://doi.org/10.1007/s00330-023-10018-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10018-2